Introduction
Acute kidney injury (AKI) is a rapid and generally reversible loss of kidney function manifested by an elevation of serum creatinine level and a reduction of urine output. The synonyms of AKI are acute renal failure and acute renal insufficiency.
- AKI can cause a buildup of water, salt, and other metabolic products.
- It can also cause a variety of electrolyte problems. The body’s electrolytes and volume are therefore dysregulated, as is the aberrant retention of nitrogenous waste.
- Chronic kidney disease (CKD), in which the kidneys steadily lose function over time, is distinct from AKI. AKI can occur within a few hours or days with sudden kidney damage.
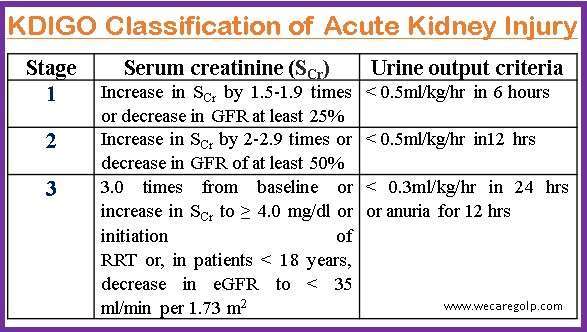
- The Kidney Disease: Improving Global Outcome (KDIGO) definition of AKI is based on changes in serum creatinine and urine output. KDIGO defines AKI as the presence of any of the following:
- Within 48 hours, increase of serum creatinine levels by 0.3 mg/dL or more (26.5 micromoles/L or more).
- Serum creatinine levels increased to 1.5 times or higher than normal within the previous seven days.
- For at least 6 hours, urine volume less than 0.5 mL/kg/h
Incidence
- AKI prevalence estimates range from 1% to 66%. These variances can be attributed to both demographic differences and uneven use of standardized AKI categorization criteria.
- AKI etiology and incidence vary across high- and low-to-middle-income nations. AKI is less common in high-income nations than in low-to-middle-income countries where polluted water and endemic illnesses like malaria lead to a high burden of AKI.
- Moreover, AKI outcomes are also worse in low-income nations in comparison to those of patients in high-income nations.
- AKI (defined by RIFLE or KDIGO criteria or as a 50% rise in blood creatinine levels from baseline) is expected to occur in 11-30% of patients after heart surgery.
- Serious AKI needing Renal Replacement Therapy (RRT) is anticipated to occur in 1-2% of these individuals.
- AKI accounts for approximately 95% of all nephrology consults.
Classification of Acute Kidney Injury
The classifications of acute kidney injury are based on the severity of the disease.
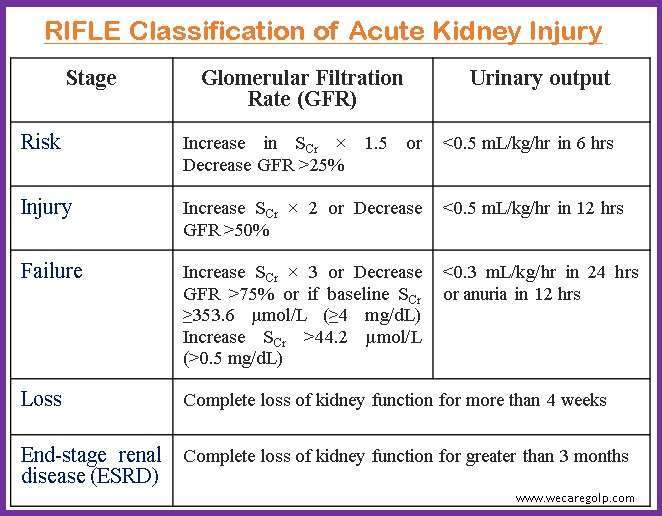
RIFLE
The RIFLE classification system (Risk, Injury, Failure, Loss, End-stage renal disease) was the first generally acknowledged approach for categorizing AKI and was developed in 2004. Changes in serum creatinine (SCr) levels and GFR are used to determine the RIFLE criterion. The RIFLE classification system divides AKI severity into five stages.
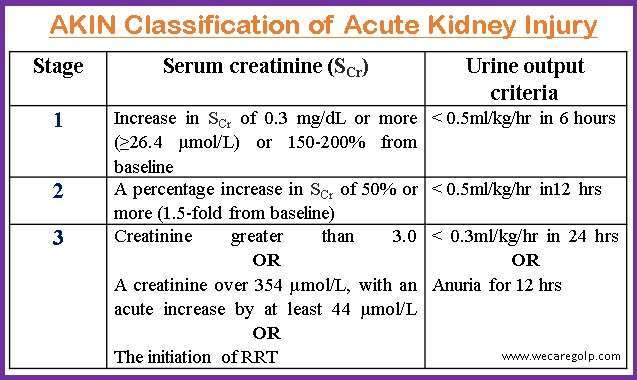
AKIN
The AKIN (Acute Kidney Injury Network) categorization system was created in 2007 as an adaption of the RIFLE criteria. Changes in serum creatinine levels and GFR are also used by the AKIN classification system to determine the severity of AKI. The AKIN criteria distinguish three levels of AKI severity.
KDIGO
As an update to the RIFLE and AKIN criteria, the KDIGO categorization system was established in 2012. Changes in serum creatinine levels and GFR are also used by the KDIGO criteria to diagnose the severity of AKI. The KDIGO criteria distinguish three levels of AKI severity.
Causes of Acute Kidney Injury
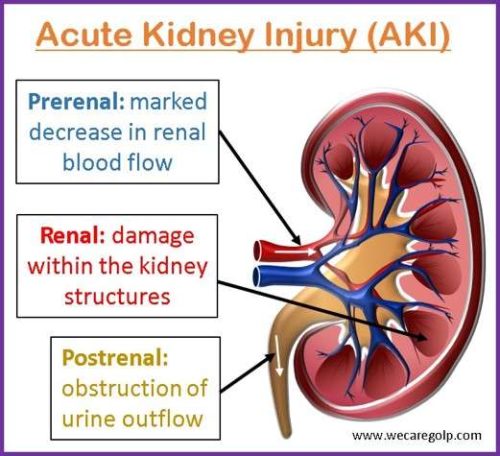
AKI can result from several factors and can understand as prerenal, intrinsic, and renal causes.
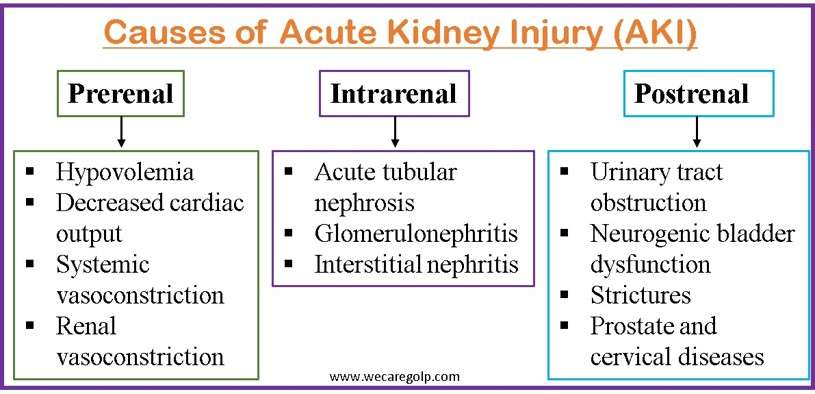
Prerenal
Prerenal causes (50-80%) reduce the blood supply to the kidneys, impairing their capacity to filter waste from the blood. This might be a hallmark of systemic hypoperfusion brought on by hypovolemia or hypotension, or it could be the result of selective kidney hypoperfusion, such as that brought on by renal artery stenosis and aortic dissection. The glomerular and tubular functions, however, frequently remain normal. These are a few instances of prerenal AKI’s mechanism:
- Hypovolemia
- Hemorrhage
- Severe burns
- Gastrointestinal fluid losses via diarrhea, vomiting, and excessive ostomy
- Decreased cardiac output/Cardia failure
- Cardiogenic shock
- Major pulmonary embolism
- Acute coronary syndrome.
- Systemic vasoconstriction
- Septic shock
- Allergy
- Anesthetic administration
- Hepatorenal syndrome
- Renal vasoconstriction
- Non-steroidal anti-inflammatory drugs (NSAIDs)
- Iodinated contrast
- Amphotericin B
- Calcineurin inhibitors
- Hepatorenal syndrome
Intra(renal)
Renal or intrinsic causes (10-30%) damage to the structure of the kidneys. Vasoconstrictors are released from the renal afferent pathways in connection with this underlying glomerular or tubular damage. The most frequent ones are prolonged renal ischemia, sepsis, and nephrotoxins. It is important to note that if the offending element is exposed for long enough to induce cellular damage, prerenal injury can develop into a renal injury.
There are several potential intrinsic causes including:
- Acute tubular necrosis (ATN)
- ATN is the most prevalent cause of renal AKI causing a lack of blood flow and oxygen to the kidney and damaging them.
- ATN develops when the tubular cells are destroyed, resulting in a loss of function.
- Medication (such as NSAIDs, aminoglycosides, and contrast agents), toxins, and ischemia can all induce ATN.
- Glomerulonephritis
- Glomerulonephritis is a collection of disorders that cause inflammation and damage to the glomeruli, which are the small structures in the kidneys that filter waste from the blood.
- Infections, autoimmune illnesses, and other reasons can all cause glomerulonephritis.
- Interstitial nephritis
- It is a disorder in which the tissue between the tubules of the kidney becomes inflamed, causing kidney damage.
- It is caused by medications such as beta-lactam antibiotics, penicillins, NSAIDs, proton pump inhibitors (PPIs), and 5-ASA, as well as infections and autoimmune disorders (SLE, IgG -disease).
- Acute interstitial nephritis is a type of interstitial nephritis with a quick onset and significant inflammation.
Postrenal
Postrenal causes (5-10%), also called obstructive uropathy, affect by mechanical blockage of the urine collecting system, which includes the renal pelvis, ureters, bladder, or urethra. Obstructive causes, which induce filtration system congestion and a change in the filtration driving forces, are the most common postrenal causes.
The possible postrenal causes are:
- Obstruction of the urinary tract (a blockage in the ureters, bladder, or urethra, which can be due to kidney stones, tumors, blood clots, or an enlarged prostate gland)
- Neurogenic bladder dysfunction (the bladder loses control owing to nerve injury, causing urine to back up into the kidneys due to diseases like multiple sclerosis, diabetes, and Parkinson’s disease)
- Strictures (narrowing of the ureters or urethra)
- Other postrenal cause
- Benign Prostate Hyperplasia (BPH)
- Prostate and cervical cancer
- Retroperitoneal fibrosis
Risk Factors of Acute Kidney Injury
- Ageing (adults older than 75 years)
- Diabetes or preexisting CKD
- Medical problems like sepsis, liver failure, cardiac failure
- Exposure to contrast agents
- Cardiac surgery
Signs and Symptoms of Acute Kidney Injury
- Hypertension
- Edema
- Decreased urine output
- Shortness of breath
- Anorexia
- Nausea
- Sleep disturbances
- Altered mental status
- Maculopapular rash
- Keratitis, iritis, uveitis, dry conjunctivae
- Jaundice: Liver disease
- Irregular rhythms
- Uremic pericarditis
- Increased jugular venous distention
- Pulsatile mass or bruit
- Abdominal or costovertebral angle tenderness
Pathophysiology of Acute Kidney Injury
The pathophysiology of acute kidney injury involves a complicated interplay between vascular, tubular, and inflammatory components, followed by a healing process that can either lead to the progression of fibrotic CKD or normal epithelial differentiation and function.
- AKI is frequently caused by reduced renal blood flow, which can be caused by a variety of reasons such as hypovolemia, hypotension, or decreased cardiac output. The decrease in blood flow causes a decrease in oxygen and nutrition to the renal tissues, triggering the pathophysiological cascade.
- A reduction in oxygen delivery causes cellular hypoxia, which causes a cascade of cellular reactions such as oxidative stress, inflammation, and cell death.
- The renin-angiotensin-aldosterone system (RAAS) is activated: The reduction in renal blood flow causes the release of renin from the kidney’s juxtaglomerular cells, which activates the RAAS. Angiotensin II, a powerful vasoconstrictor, is generated, causing additional constriction of the renal arterioles.
- This lowers renal blood flow even further and exacerbates cellular hypoxia.
- Tubular cell damage and death: Cellular hypoxia causes tubular cell injury and death in the kidney. This harm can also be induced by the buildup of poisons or medicines that are not efficiently removed as a result of the reduced GFR.
- As tubular cells are injured and die, the permeability of the tubular basement membrane increases, resulting in filtrate back leak into the interstitial space. This lowers the GFR even more and adds to the buildup of waste products and electrolytes in the body.
- Tubular cell damage and death cause an inflammatory response, which results in the production of cytokines and chemokines, which draw immune cells to the site of injury. This aggravates the damage and may result in further tubular cell death. Inflammation and damage both stimulate the coagulation system, resulting in the development of microthrombi inside the renal vasculature. This decreases renal blood flow even further, exacerbating cellular hypoxia and tubular damage.
- Repair and regeneration: The kidneys have an amazing ability to heal and regenerate, and with the right therapy and eradication of the underlying cause, destroyed tubular cells may be replaced and renal function restored.
Diagnosis of Acute Kidney Injury
A thorough patient history and physical examination, with a focus on evaluating the patient’s volume status, are essential for determining the etiology of acute kidney injury.
- The history should reveal any usage of nephrotoxic drugs or systemic diseases that may have resulted in poor renal perfusion or directly impairing renal function.
- A physical examination should be performed to determine intravascular volume status and any skin rashes that may indicate systemic disease.
- AKI can be diagnosed if any one of the criteria introduced by the KDIGO definition in 2012 is present (see above in the introduction section).
Blood test
- Serum creatinine
- Blood urea nitrogen (BUN)
- The ratio of BUN to creatinine
- Glomerular filtration rate (GFR)
- Blood gas analysis (BGA)
- Complete blood count
- Low hemoglobin may indicate chronic anemia or abrupt blood loss.
- Elevated WBC may be an indication of infection
- Thrombocytopenia may be a sign of portal hypertension or thrombotic microangiopathy.
Urinalysis
- Measurement of 24 hours urine output
- Urine protein
- Urine osmolality
- Urine albumin to creatinine ratios
Electrolytes in urine
- The amount of salt (sodium) eliminated from the body through urine in comparison to the amount filtered and reabsorbed by the kidney is called fractional excretion of sodium (FENa).
- In individuals with oliguria, measuring FENa can assist distinguish between prerenal and intrinsic renal causes of acute kidney damage.
- The following formula defines FENa:
- Less than 1% denotes a prerenal cause
- More than 2% denotes an intrinsic renal cause
- Greater than 1% may be caused by diuretic-induced natriuresis
- Less than 1% can also be found in other disorders like contrast nephropathy, rhabdomyolysis, acute glomerulonephritis, and urinary tract obstruction.
Urine dipstick
The National Institute for Health and Care Excellence (NICE) AKI guideline in the United Kingdom recommends performing urine dipstick testing for blood, protein, leucocytes, nitrites, and glucose in all patients as soon as AKI is suspected or detected to avoid missing any potentially treatable glomerular or tubular pathologies. These are some examples:
- Glomerulonephritis (with hematuria and proteinuria)
- Acute pyelonephritis (pyuria/leukocyturia with urine nitrites)
- Interstitial nephropathy (occasionally with eosinophiluria)
Imaging modalities
- Most patients with acute kidney damage, particularly older men, should have a renal ultrasonography to rule out blockage (i.e., a postrenal cause).
- The presence of more than 100 mL of postvoid residual urine (as measured by a bladder scan or urethral catheterization if a bladder scan is not available) signals postrenal acute kidney damage and necessitates renal ultrasonography to detect hydronephrosis or outlet blockage (neurogenic bladder dysfunction).
- Other imaging modalities, such as computed tomography or magnetic resonance imaging, may be necessary to determine extrarenal sources of blockage (e.g., pelvic tumors).
Renal biopsy
- Renal biopsy indicates for
- Prerenal and postrenal causes of acute kidney damage
- Unknown cause of AKI
- Rejection of kidney transplant
- It is especially crucial when clinical evaluation and laboratory studies reveal a diagnosis that must be confirmed before disease-specific treatment (e.g., immunosuppressive medicines) is started.
- Patients with oliguria who have quickly developed acute kidney damage, hematuria, and red blood cell casts may require an immediate renal biopsy. In this case, the biopsy may support the commencement of specific treatments, such as plasmapheresis, in addition to showing a diagnosis requiring immunosuppressive medication.
Management of Acute Kidney Injury
Individuals with acute kidney injury should be hospitalized unless the disease is mild and obviously caused by a treatable cause.
Volume (fluid) management
- The key to successful management is to achieve and maintain hemodynamic stability avoiding hypovolemia and hypervolemia.
- Isotonic solutions (e.g., normal saline) are preferred in case of intravascular volume depletion.
- Volume overload occurs in certain AKI patients and should be treated as soon as possible to minimize pulmonary and cardiac consequences. The primary indication for using diuretics is to control excess volume.
- Furosemide, a cornerstone in the management of such patients, can be used to reach a euvolemic condition.
- Intravenous loop diuretics, administered as a bolus or continuously, can be beneficial in this situation.
- Nevertheless, in the absence of volume overload, diuretics do not improve morbidity, mortality, or renal outcomes and should not be used to prevent or treat acute kidney injury.
Hyperkalemia Management
It is critical to pay attention to electrolyte abnormalities (e.g., hyperkalemia, hyperphosphatemia, hypermagnesemia, hyponatremia, hypernatremia, and metabolic acidosis). If hyperkalemia develops, it must be treated aggressively since it can be fatal in AKI patients. Methods for lowering potassium levels in the body include:
- Dietary restrictions
- The inhalative administration of β-mimetics (e.g., albuterol) – 2 strokes. The β-mimetics induce potassium transport from extracellular to intracellular. The effect occurs after just a few minutes, it is not particularly pronounced, but it is an important first step as an immediate measure.
- IV dextrose and insulin: The intravenous administration of 50% dextrose and 5 to 10 units of regular insulin can move potassium from extracellular to intracellular.
- Potassium-binding resins: Sodium polystyrene sulfonate (SPS) increases colonic potassium excretion
- Calcium gluconate (10%): slowly inject 10ml over 3-4 minutes in case of cardiac arrhythmia
- Hemodialysis with low potassium concentration
Conservative Management
- Antibiotics
- Proper nutrition
- Mechanical ventilation
- Glycemic control
- Erythropoiesis Stimulating Agents (ESA) for the treatment of renal anemia
- Pulse steroids, cytotoxic treatments, or a combination may be explored in individuals with rapidly developing glomerulonephritis, usually after a kidney biopsy confirms the diagnosis.
Hemodialysis
It is an effective type of renal replacement therapy until the kidneys recover. The typical indications of hemodialysis to treat AKI complications are
- Persistent and non-responsive hyperkalemia
- Uremic pericarditis or pleuritis
- Pulmonary edema
- Oliguric phase of acute tubular nephrosis
- Electrolyte imbalances
- Acid-base imbalances
- Fluid overload unresponsive to medical care
- Uremic encephalopathy
- Intoxications (e.g., ethylene glycol, lithium)
Continuous Renal Replacement Therapy (CRRT)
- Patients who are unable to tolerate hemodialysis because of hypotension or anticoagulants may also benefit from continuous renal replacement therapy.
- It is a continuous, slower method of hemodialysis that can be done for up to 72 hours at a time.
- Different types of CRRT are
- Continuous venovenous hemofiltration (CVVH)
- Continuous venovenous hemodialysis (CVVHD)
- Continuous venovenous hemodiafiltration (CVVHDF)
Complications of Acute Kidney Injury
- Hyperkalemia: Severe hyperkalemia can produce arrhythmias; hence renal replacement treatment is essential in extreme instances.
- Metabolic acidosis is caused by the kidney failure to eliminate acids, which may demand systemic injection of bicarbonate or citrate buffers.
- Hyperphosphatemia is typically preventable by reducing food intake or utilizing phosphate binders.
- Additional side effects include pulmonary edema as a result of volume overload and peripheral edema as a result of an inability to eliminate bodily fluids. This is particularly prevalent during the oliguric phase of acute tubular necrosis. It is possible that diuretics or renal replacement medication will be required.
- Pericarditis
- Encephalopathy
- Gastrointestinal bleeding
- Thrombotic thrombocytopenic purpura (TTP)
- Hemolytic uremic syndrome (HUS)
- Uremic neuropathy
- Chronic kidney disease (CKD)
- End-stage renal disease (ESRD)
Prevention of Acute Kidney Injury
- Maintain adequate hydration: It is crucial to maintain hydration in order to avoid AKI. By maintaining appropriate blood flow to the kidneys and flushing out toxins from the body, fluid consumption is beneficial.
- Management of medications: AKI can be caused by various medicines, including non-steroidal anti-inflammatory drugs (NSAIDs), some antibiotics, and contrast chemicals used in medical imaging. Careful drug management is essential, particularly for people who already have renal disease.
- Avoiding nephrotoxic substances: AKI can be brought on by several substances, including alcohol, chemicals, and heavy metals. AKI can be avoided by avoiding exposure to certain drugs.
- Avoiding hypotension and GI bleeding: It helps prevent the limitation of blood flow to the kidneys.
- Frequent renal function testing: To monitor kidney function and identify any abnormalities early, people who are at risk of having AKI should get regular kidney function testing.
- Monitoring blood pressure and blood sugar levels: AKI can eventually result from chronic renal disease, which is mostly brought on by high blood pressure and diabetes. In those with these diseases, monitoring and managing blood pressure and blood sugar levels helps avoid AKI.
- Treatment of infections in a timely manner: Sepsis and urinary tract infections (UTIs) are two illnesses that can lead to AKI. AKI can be avoided by promptly treating certain infections.
Prognosis
- With supportive therapy, most acute kidney injury victims fully recover; however, the prognosis largely relies on the cause of the AKI as well as the existence or absence of preceding renal disease or decreased eGFR.
- If the underlying disease is treated promptly, most AKI cases due to prerenal causes recover fully. However, if the underlying cause is acute tubular necrosis, the damage might not fully heal.
- The recovery from individual episodes may be full or partial, but repeated AKI might result in a cumulative decline in renal function. AKI has a mortality rate of 40–50%, whereas ICU patients have a mortality rate of over 50%.
- Acute kidney injury raises the risk of developing CKD in the long-term. Additionally, they are more likely to develop end-stage renal disease and premature death.
Summary
- An abrupt and frequently reversible loss in kidney function is referred to as acute kidney injury. It is distinguished by a significant rise in serum creatinine and a decrease in urine production.
- Dehydration, kidney injury from toxins or drugs, the decreased blood supply to the kidneys, or blockage of the urinary system are the etiological factors of AKI.
- Blood and urine tests are used to identify AKI, and the underlying cause determines how it should be treated. Reversing the damage in certain instances may only need treating the underlying cause and supportive treatment, such as fluids and electrolyte balance.
- To avoid complications and save the patient’s life, more aggressive therapy, such as dialysis, may be required in other circumstances. Improved patient outcomes and the prevention of irreversible kidney damage depend on the early diagnosis and treatment of AKI.
References
- Barasch, J., Zager, R., & Bonventre, J. V. (2017). Acute kidney injury: a problem of definition. The Lancet, 389(10071), 779-781. https://doi.org/10.1016/S0140-6736(17)30543-3
- Basile, D. P., Anderson, M. D., & Sutton, T. A. (2012). Pathophysiology of acute kidney injury. Comprehensive Physiology, 2(2), 1303-1353. doi: 10.1002/cphy.c110041
- Kellum, J. A., Bellomo, R., & Ronco, C. (2008). Definition and classification of acute kidney injury. Nephron Clinical Practice, 109(4), c182-c187. https://doi.org/10.1159/000142926
- Kellum, J. A., Romagnani, P., Ashuntantang, G., Ronco, C., Zarbock, A., & Anders, H. J. (2021). Acute kidney injury. Nature reviews Disease primers, 7(1), 52. https://doi.org/10.1038/s41572-021-00284-z
- Levey, A. S., & James, M. T. (2017). Acute kidney injury. Annals of internal medicine, 167(9), ITC66-ITC80. https://doi.org/10.7326/AITC201711070
- Palevsky, P. M. (2020). Definition and staging criteria of acute kidney injury in adults. In: Motwani S, ed. UpToDate. Waltham, Mass.: UpToDate. https://www.medilib.ir/uptodate/show/7238
- Patschan, D., & Müller, G. A. (2015). Acute kidney injury. Journal of Injury and Violence Research, 7(1), 19-26. doi: 10.5249/jivr.v7i1.604
- Ronco, C., Bellomo, R., & Kellum, J. A. (2019). Acute kidney injury. The Lancet, 394(10212), 1949-1964. https://doi.org/10.1016/S0140-6736(19)32563-2
- Srisawat, N., Hoste, E. E., & Kellum, J. A. (2010). Modern classification of acute kidney injury. Blood purification, 29(3), 300-307. https://doi.org/10.1159/000280099
- Thomas, M. E., Blaine, C., Dawnay, A., Devonald, M. A., Ftouh, S., Laing, C., … & Ostermann, M. (2015). The definition of acute kidney injury and its use in practice. Kidney international, 87(1), 62-73. https://doi.org/10.1038/ki.2014.328
- Workeneh, B. T. (December 10,2021). Acute Kidney Injury (AKI). Medscape. Retrieved on 2023, Feb 28 from https://emedicine.medscape.com/article/452289-overview
- Zuk, A., & Bonventre, J. V. (2016). Acute kidney injury. Annual review of medicine, 67, 293-307. https://doi.org/10.1146/annurev-med-050214-013407