Renal Anemia
Anemia
Before learning about renal anemia, first, you should know about anemia. Anemia is defined as a reduced hemoglobin (Hb) level or too low proportion of erythrocytes in the blood volume (hematocrit). In other words, anemia is a medical condition of an insufficient transport of oxygen in the blood.
According to the WHO definition, anemia exists when the hemoglobin concentration is < 12 g/dL (women) or < 13 g/dL (men).
There are different types of anemia. Renal anemia is one of them.
Renal Anemia
- Renal anemia is caused by the kidneys producing too little erythropoietin (EPO) hormone due to a functional deficiency. In simple, anemia in chronic kidney disease (CKD) is called renal anemia.
- Erythropoietin (EPO) stimulates the formation of red blood cells in the bone marrow.
- Renal anemia can be the result of chronic kidney disease or kidney damage.
- The resulting renal anemia is usually aggravated by a shortened lifespan of red blood cells.
- Managing kidney disease may help to delay or prevent renal anemia from getting worse.
- Renal anemia leads to left ventricular hypertrophy; also, myocardial ischemia and cardiac decompensation are possible.
Symptoms of Renal Anemia
The typical symptoms in all type of anemia are complaints resulting from the low supply of oxygen to the body.
Classic symptoms
- Fatigue
- Dizziness and
- Shortness of breath.
Others are
- Headache
- Reduced mental and physical performance
- Fast or unusual heart beat
- Pale, dry and easily bruised skin
- Cold hands and feet
- Chest pain
- Brittle nails
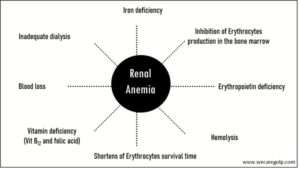
Causes
- Erythropoietin deficiency – kidney disease, uremic toxins
- Inhibition of Erythrocytes production in the bone marrow
- Iron deficiency
- Hemolysis – uremic toxins
- Shortens Erythrocytes survival time
- Vitamin deficiency – Vit B12 and folic acid
- Inadequate dialysis
- Blood loss
Anemia Screening
Renal anemia can occur with GFR<60 ml/min. Anemia Screening is therefore indicated:
- For GFR < 60 ml/min annually
- Below 30 ml/min at least twice a year
- In case of anemia, follow-up is necessary at least quarterly
- In end-stage renal failure (G5) monthly
Diagnosis of Renal Anemia
For diagnosis, at least the determinations of the following factors are required.
- Hemoglobin (Hb)
- Hematocrit (Hct)
- Erythrocyte indices (MCV,MCH)
- Reticulocytes
- Ferritin
- Transferrin saturation (TSAT)
- Vitamin B12 and folic acid
Treatment of Renal Anemia
Erythropoiesis-Stimulating Agents (ESAs):
- EPO (erythropoietin) is underproduced when renal function is impaired.
- An ESA may prescribe to treat renal anemia. It sends a signal to your bone marrow to make more red blood cells.
- If a patient is on hemodialysis, he may receive IV or subcutaneous ESAs during dialysis treatments.
- Iron supplements may prescribe to help ESAs work better.
- It may ease your symptoms and help to avoid blood transfusion.
- The goal of clinical erythropoietin substitution is to increase hematocrit (EPO – Therapy Begin: Hb ≤ 10g/dl; Target – 11.5 g/dl: not >13g/dl ).
- There are several recombinant human erythropoietin (rhEPO).
- Epoetin alfa (Abseamed, Eprex, Epogen, Procrit)
- Epoetin beta (NeoRecormon)
- Darbepoetin alfa (Aranesp)
- Darbepoetin alfa (Aranesp) differs from epoetin (alfa and beta) by:
- Two extra carbohydrate chains, which delay the degradation of the protein.
- Two to three times longer half-life (Epoetin: i.v.: 8.5 h, s.c.: 16-24 h and Darbepoetin: i.v.: 21 h, s.c.:49 h)
- The frequency of application can be significantly reduced.
Iron supplements:
- In renal disease, oral iron administration is thought to be less effective due to increased hepcidin levels. Therefore, intravenous iron is most commonly used. Target parameters are:
- Serum ferritin 100 – 500 µg/l, transferrin saturation 20 – 30 %.
- In dialysis patients: serum ferritin 200 – 500 µg/l, transferrin saturation 30 – 50 %.
- Iron substitution should be performed when transferrin saturation is below 30%, and ferritin level is below 500 ng/ml (µg/l).
- Evaluation of iron stores should be done at least every three months.
- More frequent controls are necessary, especially in active bleeding (consider blood losses during dialysis) and after starting ESA therapy (Erythropoiesis-Stimulating Agents).
- In case of systemic infections, iron therapy should be interrupted.
Red blood cell transfusion:
- In some cases, blood transfusion is used to treat severe anemia in CKD.
- A blood transfusion can quickly increase the number of red blood cells and temporarily relieve the symptoms of anemia.
- Blood transfusion can sometimes lead to other health problems (that´s why, it may limit or avoid) including:
- The body may develop antibodies over time that damage or destroy the donor blood cells and may delay or reduce the possibility of a future kidney transplant.
- Iron from transfused red blood cells can build up in the body and damage organs, called iron overload or hemochromatosis.
Vitamin supplements:
- Vitamin supplements such as vitamin B12 or folate may need to make healthy blood cells.
Causes of non-response of ESAs are
Common causes
- Absolute or functional iron deficiency
- Infections
- Inadequate dialysis
- Hyperparathyroidism/ ostitis fibrosa
- Chronic blood loss
- Malnutrition
Secondary causes
- Inadequate ESA dose
- Systemic diseases
- Folic acid, vitamin B12 deficiency
- Bone marrow disease (Myelodysplastic syndrome)
- Other malignant diseases
- Hemoglobinopathies
- Hemolysis
- Drugs: cytotoxic, immunosuppressive drugs
- Aluminium toxicity
- Antibodies against EPO (PRCA = pure red cell aplasia)
Side effects of ESAs
Usually, there is significantly less side effect of ESAs. Most common side effects of therapy with recombinant human erythropoietin:
- Headache
- Gastrointestinal discomfort
- Tachycardia
- Coagulation disorders (like fistula thrombosis)
- Hypertension
References
- Anemia: Causes, Symptoms, Diagnosis, Treatments (webmd.com)
- Anemia in Chronic Kidney Disease | NIDDK (nih.gov)
- Anemia Symptoms, Causes, and Treatments – American Kidney Fund (AKF)
- Anemia of Chronic Kidney Disease | Michigan Medicine (uofmhealth.org)
- Renale Anämie – DocCheck Flexikon
- Anemia in Chronic Kidney Disease: Causes, Treatment and More (healthline.com)
- How the Target Hemoglobin of Renal Anemia Should Be? – FullText – Nephron 2015, Vol. 131, No. 3 – Karger Publishers
