Introduction
Oxygen therapy is a type of medical treatment used to provide supplemental (additional) oxygen (O2) to patients who may have low O2 levels in the blood (hypoxemia) due to some disease conditions like respiratory problems. It has the potential to improve overall health and respiratory function significantly. In different healthcare settings, including hospitals, clinics, and home care, oxygen therapy is widely used.
Its primary objective is to raise blood oxygen saturation levels by supplying more O2 to the tissues and organs. It can help alleviate respiratory symptoms and complications. Although oxygen therapy is life-saving means for many patients, it can be dangerous if it is not handled properly.
Medical professionals should always direct and supervise the administration of this therapy. They will monitor the patient’s response to treatment and determine the appropriate oxygen flow rate and therapy duration. Regular therapy assessment helps achieve maximum benefits and avoid potential risks from oxygen toxicity or inadequate oxygenation.
Read also: Understanding Medical Terms
Oxygen (O2)
O2 is the air that we breathe which is colorless, tasteless, and odorless. It is also considered a highly reactive gas element that is required for living. This is a basic element found on the earth. Normally, the atmosphere contains 21% of O2. It plays an important role in the biochemical and physiological processes that enhance daily living. Normally, O2 enters the body through breathing and is transported into the bloodstream via the gas exchange in the alveoli. Being a basic property, O2 is essential for proper body function and helps in gas exchanges so that cells get O2 for energy production.
A healthy oxygen level is called oxygen saturation and it should be 95% and more. If the oxygen saturation drops below 88%, the healthcare provider administers oxygen therapy.
The following tests can measure oxygen saturation:
- Pulse oximeter
- Spirometry
- Arterial blood gas (ABG) analysis
Purposes of Oxygen Therapy
- To increase the oxygen saturation level in the tissues, organs, and blood
- To correct hypoxemia by raising alveolar and blood levels of O2
- To reduce respiratory complications
- To enhance the cell’s metabolic functions
- To provide humidity to liquefy the bronchial secretion
Indications of Oxygen Therapy
A change in the respiratory rate or pattern may be the indicator for oxygen therapy.
Physiologically, oxygen therapy may be indicated in people with
- Arterial oxygen partial pressure (PaO2) ≤ 55mmHg (7.3kPa) or
- Arterial oxygen saturation (SaO2) ≤ 88%
Some conditions that may need oxygen therapy are
- Respiratory disorders
- Acute respiratory failure
- Pneumonia (distress)
- Chronic obstructive pulmonary disease (COPD)
- Chronic bronchitis
- Asthma
- Emphysema
- Lung cancer
- Sleep apnea
- Shock
- Poisoning (cyanide and carbon monoxide)
- Myocardial infraction
- Heart failure
- Anemia
- During anesthesia for recovery
- Burn
- Head injury
- Severe trauma
- Altitude sickness
Contraindications of Oxygen Therapy
- Pneumothorax
- History of thoracic surgery
- Concurrent upper respiratory tract infection
- Seizure disorder
- Chronic sinusitis
- Epilepsy
- Metastatic cancer
- Sickle cell anemia
- Emphysema with carbon dioxide (Co2) retention
- Uncontrolled high fever
Types of Oxygen Therapy
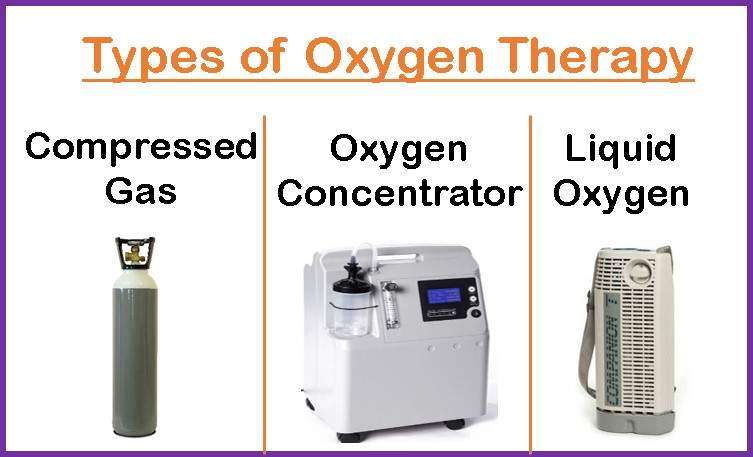
Compressed Gas
It is the most preferable type of oxygen therapy containing large metal cylinder which stores 100% O2 as a gas under pressure. This cylinder contains black color with white boarder on upside. Mostly it is used in hospital and domiciliary setting.
The cylinder contains:
- Cylinder valve
- Flowmeter
- Cylinder concentration
- Cylinder pressure gauze
- Delivery pressure gauze
- Pressure adjusting screw
Oxygen concentrator
An oxygen concentrator is an electrical medical device for oxygen therapy that pulls O2 from the air and removes nitrogen selectively simultaneously. A concentrator will never run out of O2 and does not require to fill. It is small and portable versions are also available nowadays. O2 is supplied from a tank through a tube. The patient receives the O2 through nasal tubes, face masks, or tubes inserted directly into the trachea (tracheostomy).
Liquid oxygen
Liquid oxygen is highly concentrated O2 that can be stored in a thermos-like portable container at low temperatures. During the use of O2, it is allowed to boil, releasing gaseous O2. The container is refillable. The gas will evaporate if it is stored long period.
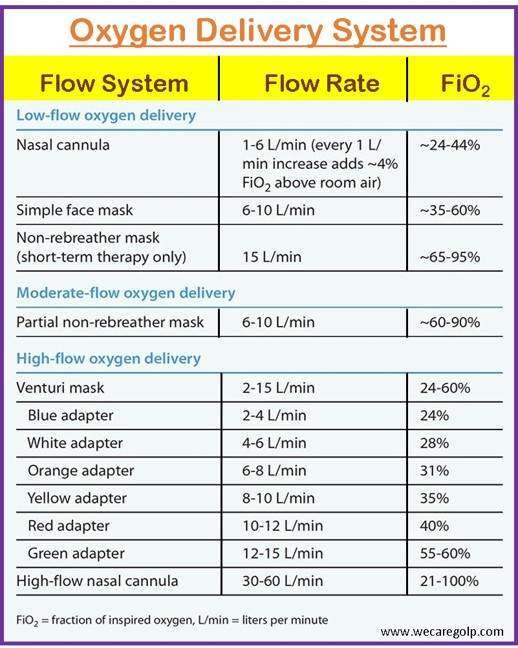
Oxygen Delivery System
Oxygen delivery systems can be classified into low-flow and high-flow systems. The purposes of selecting these systems are to treat and prevent hypoxemia and prevent complications of hyperoxygenation. The flow rate can be set between 0 – 15 L per minute.
Various factors to consider when choosing the right oxygen delivery system and device are:
- The presence of underlying disease
- Age of the patient
- Amount of oxygen required
- The presence of artificial airway
- Environmental settings (home or hospital)
- Tolerance and compliance of the patient
- A need for accurate and consistent oxygen
Low-flow system
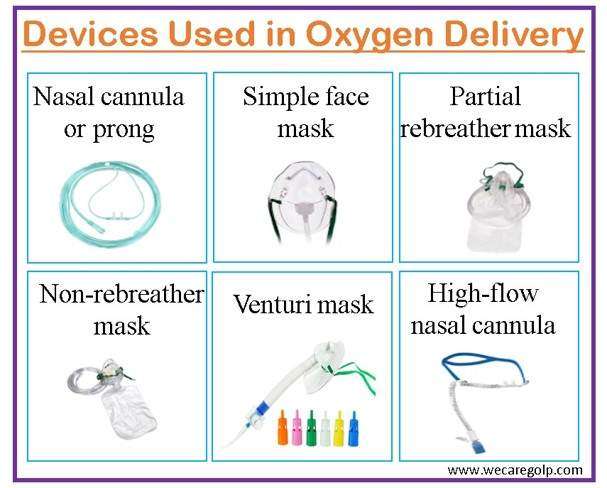
It contributes partially to the inspired gas the patient breathes. The amount of inspired oxygen changes as the patient’s breathing changes. As a result, the fraction of inspired oxygen (FiO2) cannot be accurately calculated using these oxygen delivery systems. The low-flow oxygen can be administered via different devices, e.g., nasal prongs, simple face mask, partial re-breather mask, and non-rebreather mask.
High-flow system
It provides the total amount of inspired air. As it provides higher O2 flows, the FiO2 remains stable and unaffected by the breathing pattern. It is indicated for the patient who requires a constant and precise amount of O2. Means of delivering high-flow oxygen are venture mask (aerosol mask, face tent, and T-piece) and high-flow nasal cannula.
Advantages of Oxygen Therapy
- Increase stamina
- Decrease shortness of breath
- Circulate more O2 to bloodstream which improve energy levels and decrease fatigue
- Induce better sleep
- Reduce the inflammation and swelling, strength the immune system by stimulating the release of steam cells
- Promote growth of new tissues and healing process
Disadvantages of Oxygen Therapy
- Drying and irritation of mucosa membrane of the respiratory tract
- Some physical symptoms like epistaxis (nasal bleeding), fatigue, and morning headache
- False reassurance of respiratory status
- Risk of infection if used equipment is contaminated
- Uncomfortable to use
- Frequent measurement of oxygen saturation (with pulse oximeter)
Complications of Oxygen Therapy
Because oxygen therapy is not without potential risk, patients receiving oxygen therapy may experience the following complications.
- Oxygen toxicity (if used high concentration over extended periods causing lungs damage)
- Absorption atelectasis
- Infection
- Drying of the mucous membrane
- Retinopathy of prematurity (ROP) in infants
- Hypercapnia (raised arterial pressure of carbon dioxide (PaCO2)) in those patients who have respiratory insufficiency or chronic respiratory obstruction
- Circulatory depression (rare complications)
Special Precautions
Patient Safety
- Check the O2 levels of an O2 tank regularly. The O2 level helps identify the amount of O2 consumed or reserved in the tank.
- Use only the prescribed amount of O2 at a specific time with close monitoring to avoid oxygen toxicity.
- Clean nasal prong, facemask, or reservoir mask before using. Be sure that these pieces of equipment are dry before using.
- Watch for dryness of the respiratory mucous membrane of the patient while having oxygen therapy.
- Do not use O2 continuously. Remove the nasal prong or face mask for a few hours or minutes to prevent dryness or irritation.
- Nebulizer therapy for asthma patients should utilize O2 at a rate greater than 6 L/m. After the therapy completion, patients should be back to their previous O2 equipment.
- Hypoxic patients should be positioned upright unless prohibited (in case of loss of consciousness or spinal injuries). The supine position reduces oxygenation.
- The ideal saturation range for COPD patients ranges from 88% to 92% to avoid the risk of hypercapnic respiratory failure.
- For the management and regulation of oxygen therapy in acutely ill patients, oxygen saturation levels may necessitate additional ABGs.
Environment Safety
Usually, oxygen therapy belongs to a safe treatment option. However, O2 does support combustion even though it is not a flammable gas. An oxygen concentrator is much safer than oxygen tanks. The following precautions can enhance safety.

- Maintain well ventilation in the room.
- Turn off the O2 supply immediately when not in use.
- Keep the O2 cylinder straight in an upright position and secure. Do not lean it or tilt it. Even do not cover it with any cloth or plastic. It helps avoid pressure in the tank and prevent an explosion.
- Do not smoke near the O2 container. Use the sign “No Smoking” to prevent fire.
- Keep a minimum distance of at least 5-8 feet from flames or heat-producing objects, including heaters, gas stoves, candles, fireplaces, electrical devices, and firepits when using O2. Avoid direct sunlight in the O2 cylinder or concentrator.
- Avoid petroleum-based products while handling O2 tanks because they contain alcohol, which increases the fire risk.
- Avoid the use of sprays and alcohol products near the concentrator.
- Transfer the O2 cylinder, tank, and container safely and correctly.
- Be sure the tube or vent is straight and not blocked before using it.
- Check O2 humidification regularly. Humidify before use and avoid dry air.
Hyperbaric Oxygen Therapy
A different kind of oxygen therapy called hyperbaric oxygen therapy (HBOT) involves inhaling pure O2 through a pressure chamber or tube. HBOT makes it possible for the lungs to take in up to three times as much O2 as they would if you breathed O2 through normal air pressure. Hemoglobin serves as a secondary transport medium when pure O2 is inhaled at a pressure greater than one atmosphere. Physical dissolution in the plasma is the only way to increase O2 absorption. Patients get HBOT only in the health care setting. It can take 45 to 300 mins, depending on the type of disease. The objective of HBOT is to supply the blood with sufficient O2 for tissue repair and normal body function.
The mechanisms of HBOT are:
- Strengthen the body’s immune system by blocking the activities of harmful microorganisms
- Prevent reperfusion injury
- Encourage the growth of new skin cells and collagen
- Aid in wound healing by delivering oxygen-rich plasma to oxygen-starved tissue
HBOT is useful to treat some conditions include
- Carbon monoxide poisoning
- Decompression sickness
- Gas gangrene
- Gas or air embolism
- Diabetic chronic wound
- Actinomycosis (chronic infection)
- Delayed radiation injury
- Refractory osteomyelitis, etc.
Summary
Oxygen therapy is an artificial way of providing O2 when oxygen saturation is low due to different causes. O2 is a basic unit of life. The main indication for oxygen therapy is hypoxemia resulting from different disease conditions. It can use for short-term as well long-term treatment.
Continuous use of O2 can also cause side effects that lead to hazardous health conditions. According to the patient’s need, healthcare providers can regulate the O2 supplementation using different devices like nasal cannulas, face masks, high-flow nasal cannulas, etc. Compressed gas, liquid oxygen, and oxygen concentrator are the methods of O2 storage.
References
- Cohen, J. (2022, Dec 15). 5 Benefits of Oxygen Therapy + Side Effects. SelfDecode. Retrieved on 2023, June 2 from https://health.selfdecode.com/blog/oxygen-therapy/
- myDr. (2011, Nov 12). Home oxygen precautions. Retrieved on 2023, June 2 from https://mydr.com.au/respiratory-health/home-oxygen-precautions/
- Nadali, A. (2021, Apr 12). EHS’ Quick Guide to Compressed Gas Cylinder Safety. The Elm. Retrieved on 2023, June 1 from https://elm.umaryland.edu/elm-stories/Elm-Stories-Content/EHS-Quick-Guide-to-Compressed-Gas-Cylinder-Safety.php
- Stubblefield, H. (2017, Jul 9). Oxygen Therapy. Healthline. Retrieved on 2023, June 2 from https://www.healthline.com/health/oxygen-therapy
- Dr. Trynaadh. (2020, June 6). Oxygen Therapy. Retrieved on 2023, June 3 from https://drtrinadh.wordpress.com/2020/06/06/oxygen-therapy/