Introduction
Cardiogenic shock (CS) is a life-threatening condition characterized by low cardiac output and compromised tissue perfusion. When the heart cannot pump enough blood to meet the oxygen and nutrient demands of the body, it occurs. Usually, several heart diseases are the reason for a severe reduction in the pumping capacity of the heart.
Cardiogenic shock occurs when more than 40% of the left ventricle dies, usually because of the obstruction of major coronary veins. It can lead to multiple organ failure and, if left untreated, death. It is a severe kind of cardiac failure that requires prompt medical attention.
To understand the related medical terms, please click here.
Incidence
- It is the leading cause of death among heart attack victims.
- As men have a higher prevalence of coronary artery disease, they are more likely than women to experience cardiogenic shock.
- In the United States, it affects between 40,000 and 50,000 persons annually. According to the American Heart Association (AHA), it occurs in approximately 7-10% of patients with acute myocardial infarction (MI).
- Recent studies show that the mortality rate for cardiogenic shock cases due to acute MI has dropped to 56% – 67% from 80% – 90%.
Causes of Cardiogenic Shock
- Coronary causes (most common)
- Acute MI
- Non-coronary causes (Conditions that stress the myocardium and conditions that result in an ineffective myocardial function belong to non-coronary causes of cardiogenic shock.)
- Severe hypoxemia
- Acidosis
- Hypoglycemia
- Other causes
- Severe Heart Failure
- Cardiac Arrhythmias
- Structural Heart Problems (e.g., valvular disease, ventricular septal defect)
- Endocarditis (infection of heart valves)
- Myocarditis (inflammation of the heart muscle)
- Drug Overdose (specific medications like beta-blockers or calcium channel blockers)
- Cardiac Tamponade (fluid or blood accumulation around the heart)
- Tension Pneumothorax (air buildup around the lungs)
- Massive Pulmonary Embolism (large blood clot in pulmonary arteries)
- Severe Hypertension
- Poisoning with substances that can affect heart-pumping ability.
Signs and Symptoms of Cardiogenic Shock
General Symptoms
- Hyperventilation (rapid respiration)
- Tachypnea (rapid breathing)
- Severe breathlessness
- Tachycardia (sudden, accelerated heartbeat)
- Loss of consciousness
- Weak pulse
- Profound hypotension
- Profuse sweating
- Cyanosis (paleness of skin)
- Cold extremities (hands or feet)
- Reduced urine output (≤30 ml/hr)
- Low oxygen saturation
Symptoms associated with a Heart Attack
- Sensation of pressure, fullness, or tightness in the center of the chest lasting for more than a few minutes
- Pain radiating to the shoulder, one or both arms, back, or even the teeth and jaw
- Increasing occurrences of chest pain
- Perspiration
- Light-headedness or sudden dizziness
- Nausea and vomiting
- Fatigue (extreme tiredness and a lack of energy)
- Feelings of doom (a sense of impending danger, anxiety, or a feeling of doom).
Risk Factors of Cardiogenic Shock
- Advanced age: Individuals aged 75 and older are at an increased risk.
- Race or ethnicity: Asian Americans and Pacific Islanders have a higher risk compared to other racial or ethnic groups.
- Gender: more common in women than in men.
- Pre-existing heart and blood vessel problems: Conditions such as coronary heart disease, heart failure, and high blood pressure.
- Diabetes
- Excess weight
- Existing cardiac diseases
- History of coronary artery bypass grafting (CABG)
- Pneumothorax
- Sepsis
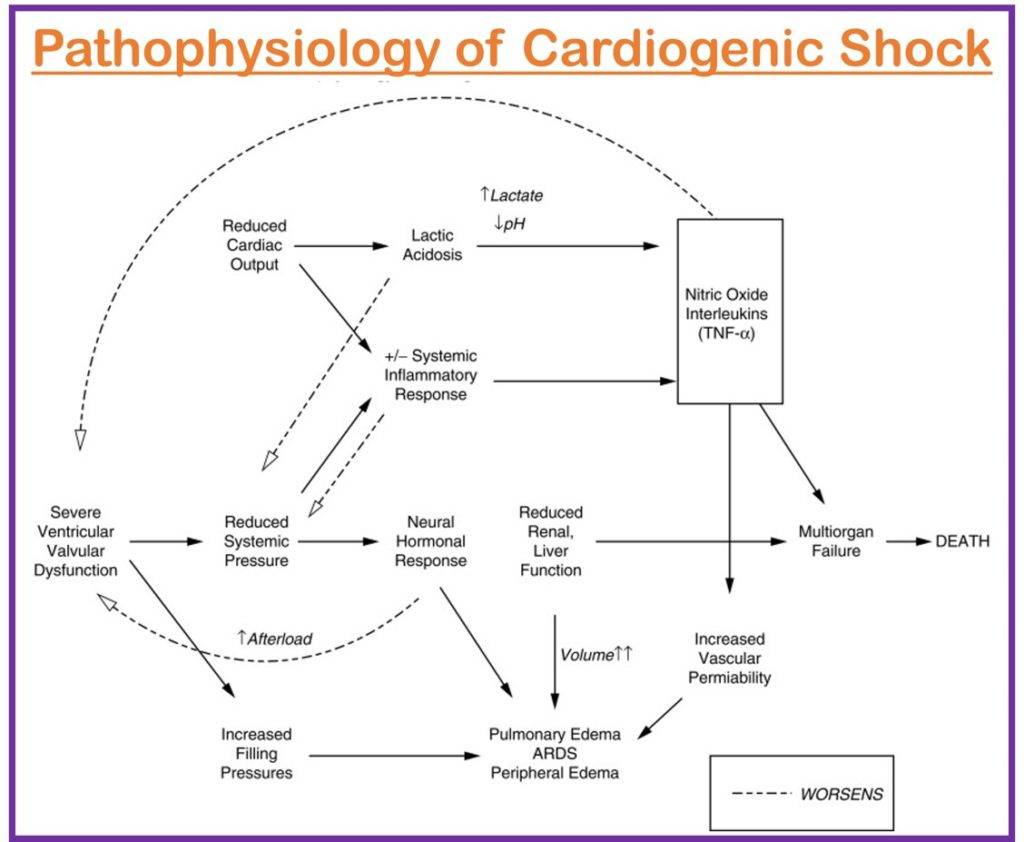
Pathophysiology of Cardiogenic Shock
Due to the poor pumping ability of the heart, a severe decrease in cardiac output leads to hypoperfusion to the tissue and oxygen scarcity to vital organs. The following several interconnected factors describe the pathophysiology of cardiogenic shock.
- Several causes like acute MI, severe arrhythmias, or myocarditis reduce the heart’s contractile function significantly. Consequently, it can impair the pumping ability of the heart.
- Myocardial dysfunction reduces the heart’s stroke volume (the amount of blood pumped out with each beat). Hence, there is a low blood supply into the systemic circulation.
- The body activates its compensatory mechanism to maintain cardiac output. The compensatory mechanism elevates the heart preload volume (volume that fills the heart from the venous return). Elevated preload volume stretches the myocardium, resulting in further dysfunction.
- Again, the body increases heart afterload (systemic vascular resistance) to compensate for reduced cardiac output. But it makes a weakened heart more difficult to pump out the blood into the arteries.
- The activation of the sympathetic nervous system enhances cardiac contractility and increases heart rate. However, prolonged neurohormonal activation may worsen ischemia and dysfunction. Additionally, there is a risk of vasoconstriction and fluid retention due to activation of the renin-angiotensin-aldosterone system (RAAS).
- Myocardial ischemia enhances the death of myocardial cells and worsens cardiac function.
- The possibility of organ hypoperfusion is high due to decreased cardiac output. The low oxygenated blood supply to vital organs leads to multiple organ dysfunction, including renal failure, liver failure, and altered mental status.
- Moreover, the body’s inflammatory response can lead to systemic inflammation. It may further impact the tissue perfusion negatively and worsen cardiogenic shock.
- Pulmonary congestion and edema may result due to the fluid accumulation in the lungs, as the ventricle cannot fully pump out blood volume during systole.
- Furthermore, the reduction of cardiac output and ineffective systemic circulation may increase through electrical abnormalities in the case of ventricular tachycardia and fibrillation.
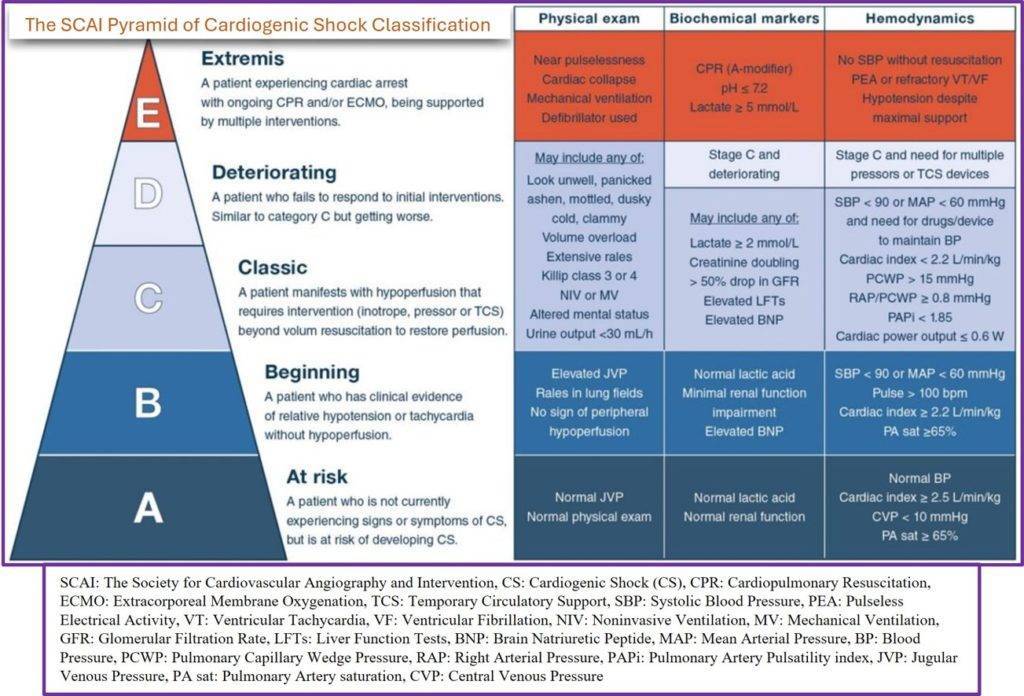
Stages of Cardiogenic Shock
The following different stages of cardiogenic shock can be classified based on numerous factors like clinical characteristics, severity, and underlying causes.
- A (At risk): No signs of shock, linked to heart disease like heart failure or heart attack
- B (Beginning): Presence of warning signs like low blood pressure and low heart rate
- C (Classic): Requirement of medicine or devices to reach the blood to organs
- D (Deteriorating): No response to the treatment (medicine or device) and getting worse
- E (Extremis): Cardiac arrest and needs CPR, ventilator, and defibrillator
The following SCAI pyramid and the clinical findings help us understand the classification of cardiogenic shock.
Diagnosis of Cardiogenic Shock
Cardiogenic shock is typically diagnosed in an emergency setting. The diagnostic process involves the following tests:
- History Taking :
- History of symptoms of heart attack on patient and family
- History of medications
- Physical examination:
- Signs and symptoms
- Auscultation may reveal a gallop rhythm, feeble heart sounds, and, possibly, a holosystolic murmur if the shock is caused by a rupture of the ventricular septum or papillary muscles.
- Blood pressure measurement: Low blood pressure is a characteristic sign of shock.
- Electrocardiogram (ECG or EKG): This noninvasive test uses electrodes put on the skin to record the electrical activity of the heart. It aids in the detection of anomalies in the electrical signals of the heart, which may indicate
- Cardiac muscle injury or
- Fluid collection around the heart.
- Chest X-ray: It is a painless and fast imaging test to collect information like:
- The size, shape, and presence of fluid in the lungs
- The size and form of the heart.
- Blood tests: Blood samples are collected to
- Assess organ damage,
- Detect infection, and
- Identify signs of a heart attack.
- Arterial blood gas (ABG) test: It can also be used to determine b
- Blood oxygen levels,
- Metabolic acidosis, and
- Hypoxia.
- Cardiac catheterization (angiogram): A long, thin tube called a catheter is placed into an artery in the arm, groin, or neck and guided to the heart during this procedure. Contrast dye is administered through the catheter using X-ray pictures to
- Detect blockage or narrowing in the coronary arteries,
- Diagnose heart diseases,
- Plan a treatment after having a heart attack.
Management of Cardiogenic Shock
Cardiogenic shock needs immediate medical attention and outcomes can vary significantly depending on underlying causes and patient’s response to therapy.
The goals of the management of cardiogenic shock are:
- To limit further myocardial damage
- To improve cardiac function by increasing cardiac contractility, decreasing ventricular afterload, or both.
- To stabilize the patient and restore tissue perfusion.
Medical Management
- Oxygenation: Supplemental oxygen is given to keep oxygen saturation levels above 90%.
- Mechanical breathing support: Devices like ventilators can protect the airway and supplement oxygen.
- Pain Control: To ease chest pain, widen blood vessels, and lessen anxiety, IV morphine is administered.
- Measurement of laboratory markers: B-type natriuretic peptide [BNP] and cardiac enzyme levels help assess myocardial damage and dysfunction.
- ECG and ST segment monitoring: To detect ischemia abnormalities, continuous ECG and ST segment monitoring is done.
- Fluid Therapy: Excessive fluid administration can worsen pulmonary congestion. Fluid overload can be avoided using diuretics.
- Continuous renal replacement therapy (CRRT): In case of acute kidney failure (AKI), it filters the waste from the blood continuously.
- Pharmacologic Therapy: The following medication therapy aims to restore and maintain adequate cardiac output.
- Vasopressors: These medications, such as dopamine, epinephrine, and norepinephrine, are used to treat low blood pressure.
- Inotropic agents: Drugs like dobutamine, dopamine, and milrinone help improve the pumping function of the heart.
- Aspirin: It is given immediately to reduce blood clotting and maintain blood flow through narrowed arteries
- Antiarrhythmic drugs: These drugs are used to normalize the heart rate while considering conditions such as hypoxia, electrolyte imbalances, and acid-base abnormalities.
- Beta-blocker: Beta-blocker decreases workload in the heart.
- Calcium channel blocker: It improves coronary blood flow.
- Thrombolytic drugs: These drugs are used to dissolve certain types of blood clots. Ex. Streptokinase, Urokinase
Surgical Management:
- Angioplasty and stenting: To open a clogged artery, a catheter with a balloon is inserted. To maintain the artery open, a stent may be implanted.
- Balloon pump: A device is put into the aorta to help with blood flow and minimize the workload on the heart.
- Extracorporeal membrane oxygenation (ECMO): A heart-lung machine delivers oxygen and eliminates carbon dioxide by pumping blood outside the body.
- Coronary artery bypass graft: If alternative therapies fail, surgery, such as coronary artery bypass graft (open heart surgery) to construct a new blood flow conduit or correct a heart injury or broken valve, may be indicated.
- Ventricular assist device (VAD): A mechanical device implanted in the abdomen that assists the heart in pumping blood. It is commonly used in patients with end-stage heart failure who are awaiting a transplant.
- Heart transplant: In severe cases where other treatments are ineffective, a heart transplant may be considered as a last resort.
Long-Term Management
- Follow up care
- Lifestyle modification
- Monitoring for potential complications
- Adherence to medicines
Complications of Cardiogenic Shock
- Dysrhythmias
- Cardiac arrest
- Renal failure
- Ventricular aneurysm
- Stroke
- Thromboembolism
- Death
Prevention of Cardiogenic Shock
Keeping the heart healthy is the best way to prevent cardiogenic shock. The following lifestyle changes can help prevent cardiogenic shock:
- Quit smoking
- Keep yourself healthy and manage your weight
- Consume less cholesterol and saturated fat
- Reduce salt intake
- Limit sugar consumption
- Moderate alcohol intake
- Engage in regular exercise
- Act promptly in case of a heart attack. If you suspect a heart attack, seek emergency medical help immediately
Prognosis
- Cardiogenic shock has a poor prognosis and is the leading cause of death in patients with an acute MI.
- Historically, the mortality rate for cardiogenic shock cases due to acute MI was 80% to 90%.
- Unfortunately, the mortality rate lies at over 30% despite the advanced therapy methods and good specialists.
- Recent studies show that the rate has dropped to 56% to 67% because of the introduction of thrombolytics, improved interventional procedures, and better therapies.
- The proportion of cardiogenic shock cases due to acute decompensated heart failure has steadily increased.
Summary
Cardiogenic shock is an emergency condition in which the body cannot get enough blood due to a sudden and severe decrease in cardiac output. Generally, the common cause of cardiogenic shock is acute MI (heart attack). However, other heart diseases like cardiomyopathies, severe arrhythmias, or valvular heart disease may also be responsible for cardiogenic shock. The pumping inability of the heart leads to symptoms like shortness of breath, tachycardia, hypotension, cold and clammy skin, low urine output, etc.
Timely recognition and intervention like emergency support and long-term management like lifestyle modifications, regular follow-up, and monitoring for potential complications may enhance the prognosis. However, it has a more than 30% mortality rate even with optimum treatment. Avoiding risk factors like obesity, smoking, pre-existing heart illness, etc., and regular check-ups can help prevent cardiogenic shock.
Read Also:
- OXYGEN THERAPY: ENHANCING RESPIRATORY SUPPORT
- SEPTIC SHOCK: RISK FACTORS, SYMPTOMS, MANAGEMENT
- ABG ANALYSIS (ARTERIAL BLOOD GAS TEST)
References
- Silvestri, L. A., & Silvestri, S. A. (2023). Saunders Comprehensive Review for the NCLEX-RN Examination (9th ed.). Elsevier.
- Mandal, G. N. (2015). Textbook of Medical-Surgical Nursing. Makalu publication house.
- Cheever, K. H., & Hinkle. J. K. (2014). Brunner & Suddarth’s Textbook of Medical-Surgical Nursing. Lisa McAllister.
- Kosaraju, A., Pendela, V. S., & Hai, O. (2023, April 7). Cardiogenic Shock. StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK482255/
- Belleza, M. (2023, May 14). Cardiogenic Shock. Retrieved on 2023, June 28 from https://nurseslabs.com/cardiogenic-shock/
- Vahdatpour, C., Collins, D., Goldberg, S. (2019). Cardiogenic Shock. Journal of the American Heart Association, 8(8),e 011991. https://doi.org/10.1161/JAHA.119.011991
- Berg, D., D., Bohula, E. A., Morrow, D.A. (2021, August). Epidemiology and causes of cardiogenic shock. Current Opinion in Critical Care, 27(4), 401-408. DOI: 10.1097/MCC.0000000000000845.
- Cleveland Clinic. (2022. May 1). Cardiogenic Shock. Retrieved on 2023, June 26 from https://my.clevelandclinic.org/health/diseases/17837-cardiogenic-shock