Introduction
Hypoglycemia is an urgent medical condition in which blood sugar (glucose) level is lower than the standard range, typically below 70 mg/dL (3.9 mmol/L). However, symptoms may occur if plasma glucose levels fall below 55 mg/dL (3.0 mmol/l). Hypoglycemia is often related to diabetes treatment. But other drugs and several conditions can cause low blood sugar in people who do not have diabetes.
Incidence
- Hypoglycemia is more common with type 1 diabetes, particularly in those who are receiving insulin therapy.
- Patients with type 2 diabetes experience hypoglycemia less frequently as compared to type 1 diabetes because of medication like metformin that commonly does not induce hypoglycemia
- There are no reported disparities in incidents based on gender. So. it is common for both males and females.
Classification of Hypoglycemia
Hypoglycemia can be classified according to severity.
- A state of mild hypoglycemia is one in which the patient can recognize the signs of hypoglycemia and manage them on their own. Consuming oral glucose (sweets/juice) is one way to raise blood glucose levels.
- Patients may experience symptoms but are unable to treat it themself. They require the assistance of a family member or caregiver. Patients will need foods high in sugar to raise their blood glucose levels.
- When patients have severe hypoglycemia, they may reach the stage of coma, indicating an immediate medical problem.
- If the patient is showing signs of hypoglycemia, no one should try to force them to feed.
- It is characterized by severe neurological symptoms and the majority of patients require intravenous dextrose and glucagon.
Types of non-diabetic hypoglycemia
Fasting hypoglycemia
- It is caused by
- A too-long gap between meals
- Medications like quinine (malarial treatment), pentamidine, salicylates (aspirin), and sulfonamides (antibiotics).
Reactive hypoglycemia
- It occurs a few hours after eating a meal with high-carbohydrate.
Causes of Hypoglycemia
Diabetics
When receiving treatment, type 1 diabetes patients are three times more likely to experience hypoglycemia than patients with type 2 diabetes.
- Diabetic drugs like insulin, sulfonylureas, and biguanides because of poor dose management.
- Take medicines but forget a meal (absence of carbohydrates)
Hypoglycemic unawareness
- Hypoglycemia unawareness (HU) is defined as the inability to detect a significant drop in blood glucose levels.
- It is the onset of neuroglycopenia (shortage of glucose in the brain) prior to the appearance of autonomic warning symptoms.
- HU occurs in approximately 40% of people with type 1 diabetes mellitus (T1DM) and less frequently in type 2 diabetes (T2DM).
- Although HU is caused by a variety of factors, some potential causes include
- Prolonged exposure to low blood glucose
- Previous hypoglycemia
- Recurrent severe hypoglycemia and
- The failure of counter-regulatory hormones.
- HU is dangerous because the patients experience the symptoms of hypoglycemia at far lower glucose levels.
Non-diabetics
- Withhold food and drink (as a part of the treatment).
- Sepsis (the body uses large amounts of glucose for energy).
- Liver failure (any damage in the liver leads to decrease glucose production)
- Renal failure (the kidney fails to remove insulin from the body)
Drugs
Various medications have been identified that cause hypoglycemia. They are as follows:
- Non-steroidal anti-inflammatory drugs (NSAIDs), e.g., Indomethacin
- Anti-malarial drugs, e.g., Quinine
- Lithium
- Antihypertensive drugs, e.g., Angiotensin-converting enzymes, Angiotensin receptor blockers, and Beta-adrenergic blockers.
- Antibiotics, e.g., Levofloxacin, Trimethoprim-sulfamethoxazole
- Anti-coagulant, e.g., Heparin
- Chemotherapeutic, e.g., Mercaptopurine
- Diabetic medications, e.g., Insulin, Glinides, Sulfonylureas
Excessive alcohol drinking
- The body’s gluconeogenesis is stymied by alcohol, but glycogenolysis is unaffected. As a result, hypoglycemia occurs after consuming alcohol for many days and depleting glycogen stores.
Hormone deficiencies
- Addison’s disease leads to low levels of cortisol (stress hormone), decreasing glucose production
- Hypopituitarism causes less secretion of growth hormone, which is also associated with low glucose production.
Surreptitious insulin use
- The deliberate use of insulin preparation to induce hypoglycemia is called factitious hypoglycemia.
Inborn errors of metabolism
- Rare genetic disorders known as “inborn errors of metabolism” involve the improper breakdown or storage of carbohydrates, proteins, and fatty acids. It results in hypoglycemia in infants.
Insulinomas
- Insulinoma is a pancreatic B-cell tumor that produces excessive insulin, more than the body can use, leading to hypoglycemia.
Insulin autoimmune syndrome
- Insulin autoimmune syndrome (IAS), also called autoimmune hypoglycemia (AIH) is a rare condition characterized by
- Recurrent hypoglycemia
- Hyperinsulinemia
- Positive insulin autoantibodies (IAAs)
- The body produces immune cells called antibodies.
- They usually attack foreign objects like bacteria and viruses, but they can also attack normal human cells, which can cause an autoimmune disorder.
- In the same way, the antibodies can attack insulin resulting in autoimmune hypoglycemia.
Non-β-cell tumor
- The non-β-cell tumors cause an elevated level of insulin, particularly insulin-like growth factor II, resulting in lower glucose levels.
- Such non-β-cell tumors are hepatomas, carcinoid tumors, and adrenocoticoid carcinomas.
Post-gastric bypass postprandial hypoglycemia
- A weight loss surgery called Roux-en-Y gastric bypass may cause post-gastric bypass postprandial hypoglycemia.
- In this condition, GLP- (glucagon-like peptide-1) hormone increases insulin production, causing low glucose levels.
- Healthy newborns younger than 48 hours who have not eaten in a few hours may experience low blood sugar.
- Following birth, the neonate adjusts glucagon and epinephrine levels for 48 hours, which may result in transient hypoglycemia.
Risk Factors of Hypoglycemia
- Excessive amounts of Insulin or insulin secretagogues drugs, inappropriate timing, or type of administration
- Decreased glucose intake (missed meals and overnight)
- Increased glucose needed during exercise
- Decreased endogenous glucose production after alcohol intake
- Insulin sensitivity is increased due to:
- Weight loss
- Improved glycemic control
- Physiologically in the middle of the night
- Renal failure may cause decreased Insulin clearance.
Glucose Metabolism
- Glucose is the major source of energy. The sources of plasma glucose are
- Dietary carbohydrates absorbed by the intestine and
- Endogenous glucose production (EGP) by glycogenolysis (breakdown of glycogen) or gluconeogenesis (synthesis of sugar without using carbohydrates).
- The fundamental biological process of EGP and glucose utilization are regulated by three hormones:
- Insulin
- Glucagon and
- Epinephrine
- When plasma glucose levels rise, pancreatic beta cells secrete insulin, which reduces glucose production and promotes glucose absorption from the blood into the target tissues like muscle, fat, and the liver.
- Low plasma glucose levels stimulate glucagon (an insulin antagonist) to increase hepatic glucose production primarily by stimulating glycogenolysis.
- Epinephrine (secreted by adrenal glands) increases glucose production directly by EGP.
Pathophysiology of Hypoglycemia
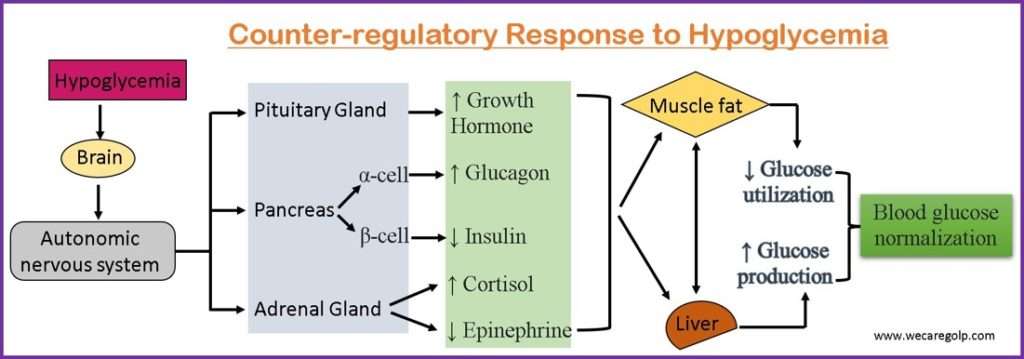
- When the blood glucose levels fall beyond the physiologic range, the counter-regulatory responses activate as a defensive response.
- The counter-regulatory mechanism utilizes three physiological defensive factors against hypoglycemia.
- Decrease insulin secretion by pancreatic β-cell
- Increase glucagon secretion by pancreatic α-cell
- Increase epinephrine secretion by adrenal glands.
- Decreased insulin secretion is the first response to hypoglycemia. The decreased insulin level leads to hepatic glycogenolysis and hepatic/renal gluconeogenesis.
- Glucagon is released if blood glucose levels continue to drop. It has glycogenolysis effects.
- In case of failure of the action of glucagon, adrenomedullary epinephrine is secreted.
- Epinephrine acts on the liver and increases hepatic glycogenolysis and gluconeogenesis.
- It converts the glycogen (stored in the liver) to glucose by glycogenolysis and produces glucose by gluconeogenesis by mobilizing gluconeogenic precursors from muscle (alanine and lactate) and fat (glycerol).
- Additionally, it restricts insulin secretion and reduces glucose clearance by insulin-sensitive tissues.
- If the counter-regulatory mechanism fails to achieve euglycemia (normal condition of blood glucose), growth hormone and cortisol are released to continue glycogenolysis and gluconeogenesis after prolonged hypoglycemia. Compared to epinephrine, the effects of growth hormone and cortisol are less potent.
Sign and Symptoms of Hypoglycemia
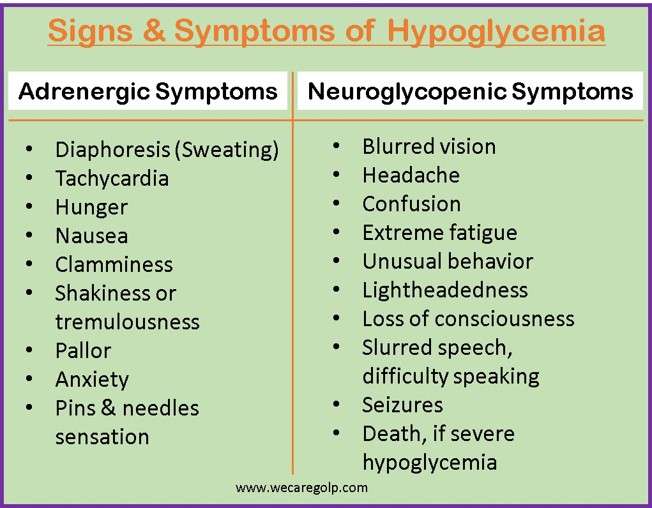
Hypoglycemic symptoms are divided into two main categories. Please be aware that each person’s symptoms may differ.
- Adrenergic symptoms result from the activation of the sympathetic nervous system and may be no danger for the patient. These symptoms are early warning features and precede neurobehavioral features.
- Neuroglycopenic symptoms occur through the lack of glucose supply in the brain (central nervous system). If the warning signs (adrenergic) are ignored, the blood glucose level falls continuously and may lead to a severe hypoglycemia. Finally, it may alter mental function that proceeds to debilitating conditions.
Diagnosis of Hypoglycemia
Whipple’s triad
- The Whipple triad describes the typical clinical manifestation in the presence of an insulinoma.
- The essential three symptoms/finding of the Whipple triad are:
- Hypoglycemia with blood sugar levels below 50 mg/dl
- Neurological and autonomic symptoms associated with hypoglycemia (sweating, tremors, tachycardia, palpitations, dizziness, confusion, paresthesia)
- Rapid clinical improvement after ingestion of glucose.
Other tests
Further diagnostic testing is required to determine the cause of hypoglycemia in individuals who do not have a history of diabetes.
- Plasma glucose level, not point-of-care measurement
- Insulin level
- C-peptide level
- Proinsulin level
- Beta-hydroxybutyrate level
- Oral hypoglycemic agent screen
- Response of blood glucose level to glucagon
- Insulin antibodies
Management of Hypoglycemia
Immediate Hypoglycemia Treatment
In a conscious patient
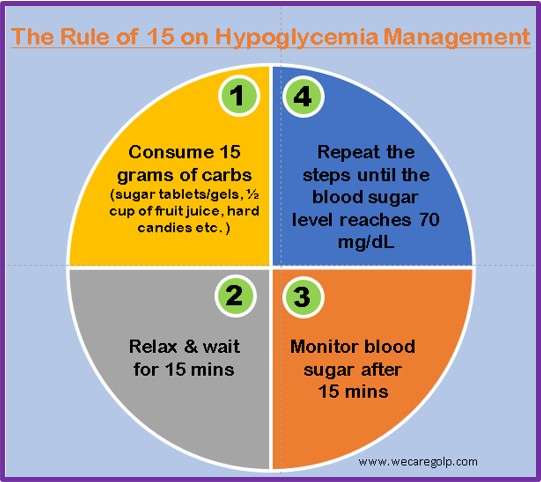
- Consume 15 to 20 grams of quick-acting carbohydrates, free of protein and fat, that quickly turn into sugar.
- Glucose tablets (see instructions)
- Gel tube (see instructions)
- 4 ounces or a half cup of fruit juice or non-diet soda
- A serving of jellybeans and hard candies (check the package for serving size)
- A cup or 8 ounces of milk
- 1 tablespoon of sugar, honey, or corn syrup
- 2 tablespoons of raisins
- Wait for 15 minutes
- After 15 minutes of treatment, check blood sugar levels.
- If the blood sugar is still below 70 mg/fL (3.9 mmol/L), eat or drink another 15 to 20 grams of fast-acting carbohydrates
- Recheck your blood sugar level 15 minutes later
- Repeat these steps until the blood sugar level reaches 70 mg/dL (3.9 mmol/L).
- Consume a snack with a slow-release carbohydrate to avoid recurrent hypoglycemia.
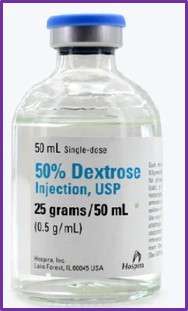
- In healthcare settings, the 15-15 rule is used if the patient is conscious and able to swallow. If this does not help the patient get back to normal blood glucose levels or if the patient is unconscious, 25 grams of 50% dextrose is usually given.
Immediate Treatment of Severe Hypoglycemia
- If a person has severe hypoglycemia and is unable to eat, they must immediately receive an intravenous glucose solution or glucagon injection.
- A glucagon kit is generally recommended for insulin-treated diabetics in case of emergency. In case of an emergency, friends, and family need to know where to find the kit and how to use it.
- If there is no glucagon kit available, call for emergency medical help.

Complications
If hypoglycemia is not treated on time, it can lead to severe symptoms like:
- Seizures
- Unconsciousness
- Falls/Accidents
- Death
Prevention of Hypoglycemia
- Identifying the symptoms and taking immediate action is the primary preventive measure.
- Health education should be given to family and friends regarding symptoms of hypoglycemia and immediate treatment to get timely help.
- Educate the patients and families regarding
- Warning signs of hypoglycemia
- Immediate treatment method
- Predisposing factors
- Meal planning
- Proper use of medicines and their side effects.
- For some people with diabetes, continuous glucose monitoring (CGM) is a good option.
- Regular consultation with a doctor is necessary for any alteration in dosage and medication.
- Wear a medical alert bracelet or badge to let people know episodes of hypoglycemia
Prognosis of Hypoglycemia
- With treatment, hypoglycemia usually has a good prognosis.
- Prolonged, severe, and timely untreated hypoglycemia can be fatal.
- Patients with diabetes should also talk to their doctors if they have frequent hypoglycemic episodes. They may need changes to their medication, meal plans, or even their exercise and activity schedule.
- Non-diabetic patients who exhibit hypoglycemia symptoms should consult their doctor for further evaluation.
Summary
- Hypoglycemia in an urgent medical condition in which blood glucose level is low than normal standard level
- Major causes of hypoglycemia are Type 1 and Type 2 diabetes mellitus.
- It causes irregular or rapid heartbeat, pale skin, and sweating.
- Immediate management of hypoglycemia is giving fast acting carbohydrates and checking blood sugar frequently.
- For healthcare management 50% dextrose is administered and glucagon may be needed.
References
- Tomky, D. (2005, Jan 1). Detection, Prevention, and Treatment of Hypoglycemia in the Hospital. Diabetes Spectr, 18(1), 39-44. https://doi.org/10.2337/diaspect.18.1.39
- Mathew, P., Thoppil, D. (2022, July 23.). Hypoglycemia. StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK534841/
- Brouhard, R. (2022, May 26). Symptoms of Hypoglycemia (Low Blood Sugar). Verywellhealth. Retrieved 2023, Jan 22 from https://www.verywellhealth.com/hypoglycemia-symptoms-1298883
- Sitaram Bhartia Team. (2019, Jun 20). Management of Hypoglycemia – How to Treat Low Blood Sugars. Sitaram Bhartia Institute of Science & Research. Retrieved 2023, Jan 22 from https://www.sitarambhartia.org/blog/endocrinology/management-of-hypoglycemia/
- Sprague, J. E., Arbela´ez, A. M. (2011, Sep). Glucose Counterregulatory Responses to Hypoglycemia. Pediatr. Endocrinol Rev, 9(1), 463-475. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3755377/