Introduction
Pyelogram is an x-ray procedure that uses radiopaque fluid to provide an image of the renal pelvis and urinary system. In other words, it is a radiographic examination of a renal pelvis following the injection of radiopaque material through the ureter or into a vein.
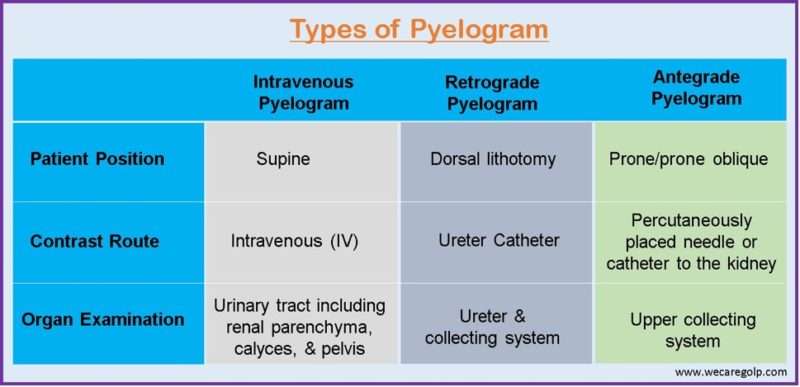
Type of pyelogram
- Intravenous pyelogram
- Retrograde pyelogram
- Antegrade pyelogram
Intravenous pyelogram
- Intravenous pyelogram (IVP), often known as intravenous urography, is a diagnostic technique that uses intravenous contrast and X-ray imaging of the urinary system.
- After the intravenous injection of the contrast medium, the radiological examination of the urinary tract including the renal parenchyma, the calyces, and the pelvis is carried out.
- It remains the primary modality for visualization of the pelvicalyceal system and ureter.
- The iodinated contrast is filtered into the collecting system after passing via the renal vasculature and illuminating the anatomic features on the X-ray picture.
- It is frequently used to evaluate hematuria and renal stone disease, as well as a follow-up following the operation.
- The urography imaging sequence is optimized for depicting particular regions of the urinary system.
- When filled with contrast material, portions of the urinary system seem opaque.
Indication
- IVP is used to evaluate flank and lower back discomfort, as well as hematuria.
- To detect congenital urinary tract malformations, urinary calculi, enlarged prostate, neoplasms of the kidney, ureter, and bladder, as well as scars and strictures of the urinary system.
- Suspected urinary tract pathology
- Repeated urinary tract infections (UTIs)
- Investigation of hypertension not controlled by medication at a young age
- Renal colic.
- Trauma (Abdominal injury)
- To assess for synchronous upper tract disease in those with bladder transitional cell carcinoma
- Ureteric fistulas and strictures
- To determine the state of the urinary tract’s integrity following a trauma.
Contraindications
There is no absolute contraindication. The relative contraindications are:
- Multiple myeloma
- Hepatorenal syndrome
- Previous allergy to the contrast agent/iodine
- Renal failure (increased serum creatinine level greater than 1.5 mg/dL)
- Generalized allergic conditions
- Infancy
- Pregnancy
- Thyrotoxicosis
- Anuria
- Diabetes mellitus
- Congestive heart failure
- Pheochromocytoma
- Sickle cell anemia
Procedure
Patient Preparation
- Review of blood chemistry
- Light evening meal before the procedure
- Bowel-cleansing laxative
- NPO after midnight (minimum of 6-8 hours)
- Enema on the morning of the examination
- Voiding before the procedure (if the bladder is too full, it could rupture especially if compression is applied early in the exam, urine in the bladder can dilute the contrast medium)
- Inform the patient about the procedure
- Informed consent
- Take careful notes on the patient’s allergies, comorbidities, prior illnesses, and medication history
- Before the procedure, request that the patient remove all jewelry and other metal items
- Check that the patient is not pregnant at the time of the surgery if she is a female. Take preventive precautions to protect the fetus from radiation exposure if she is pregnant.
During Procedure
Equipment required
- 600mA fluoroscopy-guided x-ray unit
- Abdominal compression equipment
- Medium/regular film screen
- Pads and immobilization aids
- Emergency drugs and equipment
- Intravenous administration equipment: 50ml syringe, butterfly cannula, contrast media
Contrast media
- Nonionic contrast media (iohexol-omnipaque):
- Adult dose: 300mg I/ml, 40-80ml
- Children below 7 kg- 240 mg I/ml, 4 ml/kg
- Children above 7 kg: 2ml/kg
- Ionic contrast media:
- Adult dose: 300-600 mg iodine equivalent/kg body weight, maximum of 40gm of iodine
- Children: Meglumine iothalamate or diatrizoate 60% containing equivalent of 280 mg I/ml of iodine, the dose is 1-2 ml/kg body weight.
Preliminary images
- To enhance the visibility of stones and heighten the contrast between soft tissues, images should be collected consistently.
- Imaging must cover the region below the pubic symphysis and above the suprarenal region.
- The calcification fields must be assessed before the infusion of contrast.
- When the patient may have urinary tract calculus symptoms but none are otherwise visible on the anterior-posterior (AP) view, the site and kind of calcifications are confirmed by oblique radiography.
- Based on early images, adjustments can be done following contrast delivery.
- The initial scans are extremely important since they assist identify urinary causes of the patient’s discomfort and indirectly aid in the identification of additional abdominal pathologies.
- In inspiration, supine, full-length anterior-posterior of the abdomen, the lower border of the cassette is at the symphysis pubis level, and the X-ray beam is centered in the mid-line at the iliac crests.
- If required, the location of overlaying opacities can be established further by:
- In expiration, a supine AP film of the renal regions.
- The X-ray beam is centered in the mid-line at the lower costal margin.
- 35° posterior oblique views (interest side toward the film) or
- a kidney tomography.
- The examination should not proceed until the radiologist or radiographer has seen and approved these images.
Phases of the IVP procedure
The venous access must be established. To enhance the density of the nephrogram, the cannula/needle gauge should allow the injection to be administered swiftly as a bolus.
Immediate film
- This covers the renal regions’ AP.
- This film is exposed 10-14 seconds after injection.
- Its goal is to display the nephrogram at its densest point, which is the renal parenchyma opacified by contrast media in the renal tubules.
- Tomography or ultrasonography may be used to help evaluate the renal outline or potential masses.
5-min film
- This includes the AP of the renal regions.
- Prior to applying compression, this film provides a first assessment of pathology, especially the presence or lack of blockage.
- A compression band is then placed midway between the anterior-superior iliac spines, directly across the ureters as they pass the pelvic brim.
- The goal is to cause pelvicalyceal distension.
- But compression is contraindicated in the following cases:
- After recent abdominal surgery
- After renal trauma
- If there is a large abdominal mass or aortic aneurysm
- When the 5-min film shows already dilated calyces, which point to obstruction.
10-min film
- This includes the AP of the renal regions.
- By this time, the pelvicalyceal systems are generally sufficiently distended with opaque urine.
- The compression is released once the pelvicalyceal system has been demonstrated to be effective.
- If the compression film is insufficient, it should be examined and adjusted if necessary, and an additional 50 ml of contrast media should be provided, followed by the film after 5 minutes.
Release film
- The ureters are shown in this film.
- Supine AP abdomen is taken right after the compression is released.
- The patient is asked to empty their bladder if this film meets the expectations.
After micturition film
- It includes AP abdomen supine full length.
- The goals of this film are:
- To evaluate bladder emptying
- Show drainage of the upper tracts
- Help in the identification of bladder malignancies
- Confirm ureterovesical junction calculi
- Show a urethral diverticulum in females, in rare cases.
After Procedure
- The patient should be observed for 6 hours after the procedure
- The needle wound site should be dressed and checked for extravasation
- Watchful in regards to late contrast reactions (swelling of lips or tongue or both, rash in trunk, face or limbs, difficulty in breathing)
- The patient should be encouraged to take plenty of fluid to prevent dehydration
- Renal function tests should be performed on high-risk patients to watch for deterioration.
- For patients with diabetes under medication, the regular medication should be started after 48 hours of the procedure.
Advantages
- IVP provides a clear image of the whole urinary system which allows the detection of even mild hydronephrosis.
- It is easier to identify an obstructing stone when there are multiple pelvic calcifications.
- Can reveal non-opaque stones as filling defects.
- Reveals renal function and offers verification that the opposite kidney is working normally.
- Urinary tract imaging with IVP is a minimally invasive treatment.
- IVP images give vital, comprehensive information to help doctors diagnose and treat urinary tract diseases ranging from kidney stones to cancer.
- An IVP can frequently offer enough information regarding kidney stones and urinary tract obstructions to direct drug treatment and avoid more invasive surgical treatments.
- After an x-ray examination, no radiation is left in the patient’s body.
- In the conventional diagnostic range for this scan, X-rays typically have no adverse effects.
Disadvantages
- There is a need for intravenous contrast material.
- The procedure may provoke an allergic response.
- It may not have enough opacification to define the anatomy and point of obstruction.
- It requires a significant amount of exposure to radiation and this may not be ideal for young children or pregnant women.
- If the bowel preparation is not done properly, the image quality is poor, and misdiagnosis is common.
- Furthermore, abdominal compression may cause discomfort in the patient.
Complications
Due to contrast media
- An allergic reaction to the contrast substance (hives, skin rash, and, in rare cases, anaphylactic shock).
Due to technique
- Intolerable discomfort or hypotension (due to incorrectly applied compression in the abdomen)
- Urethral trauma or rupture
- Extravasation of contrast (due to the use of excessive pressure in stricture)
- Swelling and pain during injection
Interpretation
- The typical kidney length ranges from 9 to 13 cm.
- The average renal parenchymal thickness in the polar areas is 3 to 3.5 cm, and 2 to 2.5 cm in the interpolar regions.
- The right kidney’s top pole is normally about the level of the 12th rib, while the left kidney is somewhat higher than the right.
- The kidney’s vertical axis is parallel to the ipsilateral upper part of the psoas major.
- In the case of a growing tumor, parenchymal breakdown and twofold contour may be evident.
- Post-inflammatory and stone-related scarring can both exhibit abnormal calyceal structures.
- Early and minor urinary tract obstruction might cause rounding of the forniceal margins.
- Extensive contrast material collections in the parenchyma might indicate an inflammatory reaction.
- Chronic blockage causes papillary impression loss and calyces clubbing.
- Diverticula are shown by outpouchings of contrast material.
- Renal cell cancer may cause abnormal papillae.
- Phantom calyx development can occur in both benign and malignant neoplasms due to a filling deficiency.
- Static contrast columns on numerous pictures show blockage or ureteral ileus.
- A medial deviation is defined as a separation of less than 5 cm between the ureters. If the ureter extends more than 1cm beyond the tip of the transverse process of the vertebrae, this is referred to as ureter lateral deviation.
- Narrowing of the ureteral lumen can be caused by both internal and external factors.
- Tuberculosis of the urinary system causes the following symptoms, which are evident on a pyelogram: moth-eaten calyces, sawtooth ureter, pipe stem ureter, and thimble bladder. Due to significant mural fibrosis, the bladder seems tiny and constricted.
- In the ureterocele, the cobra head sign on an IVP is apparent.
Retrograde Pyelogram
- When the IVP cannot be performed or is not warranted due to a history of allergic responses to contrast material or other contraindications, retrograde pyelography is performed to view the morphology of the ureter and collecting system.
- It entails injecting contrast material directly into the ureters retrogradely following their cystoscopic cannulation to observe the collecting system and the ureter without relying on renal contrast excretion.
- Typically, urine is produced in the kidney and passes anterogradely through the ureter before being deposited in the bladder. Retrograde refers to the direction in which the contrast is introduced.
- During the examination, it is also feasible to biopsy suspected urothelial lesions.
Indication
- To evaluate persistent intraureteral or intrapelvic filling defects on IVP
- If IVP does not provide satisfactory visualization of the renal collecting system
- For a biopsy of a suspected lesion
- To demonstrate the exact site of a ureteral fistula
- To evaluate the renal collecting system in patients who are contraindicated to receive intravenous contrast medium
- To assess ureteral obstruction
- To detect filling disorders like stones or tumors
- To facilitate percutaneous access by delineating the entire collecting system (non-hydronephrotic kidneys
- To facilitate ureteroscopy and stent placement
- To assess hematuria and trauma
- To confirm the diagnosis of ureteropelvic junction obstruction (UPJO) and pinpoint the specific position and type/nature of the obstruction. This procedure can be performed before or during UPJO intervention.
Contraindications
There is no absolute contraindication. The relative contraindications are
- Acute UTI
- In patients with contaminated urine or even bacteremia, this technique should be performed with caution.
- If the patient is severely ill and/or septic (for example, obstructive calculi with hydronephrosis, acute UTI), a stent should be inserted using gentle retrograde pyelography to guarantee optimal stent placement.
- Allergy to contrast
- Patients who have a known allergy to contrast material usually do quite well during this operation since the contrast is not taken into circulation in any meaningful amount, preventing an allergic response.
- However, if contrast is supplied under high pressure, backflow of the contrast material may occur, exposing it to the bloodstream.
- To avoid this problem, the physician should take particular steps to assure the safe distribution of contrast to these patients.
- Pregnancy
- Recent instrumentation
Procedure
Patient Preparation
- Prophylactic antibiotics must be given to every patient having ureter manipulation surgery. Fluoroquinolones and TMP-SMX are the preferred medications. If these medications are not accessible or cannot be administered due to adverse effects, aminoglycosides with ampicillin and first-/second-generation cephalosporins may be utilized.
- A recent urine test (within 2 weeks before the operation) should be conducted to check that the patient does not have a urinary infection.
- Before the procedure, the patient should fast and limit fluids for 8 hours, or as directed. Fasting may be prescribed as a precaution against aspiration caused by nausea and vomiting.
- Concerning the patient’s risk of bleeding, the patient should be informed to avoid ingesting natural products and drugs with known anticoagulant, antiplatelet, or thrombolytic properties before the procedure or to reduce the dose as directed.
- Inform the patient about the procedure.
- Take careful notes on the patient’s allergies, comorbidities, prior illnesses, and medication history.
- Before the procedure, request that the patient remove all jewelry and other metal items.
- The patient is usually given general anesthesia depending on the rationale for the retrograde pyelography.
During Procedure
- The technique begins after the patient has been anesthetized by assuring adequate placement of the patient in the dorsal lithotomy posture.
- A cystoscopy is conducted once the placement is complete. The cystoscope is to locate the left and right ureteral orifices.
- The physician next cannulates the ureter which must be scanned with a 5F or 6F open-ended or cone-tipped catheter. The ureteral catheter is flushed prior to cannulating the ureteral orifice to ensure that there are no air bubbles within the catheter’s lumen. This prevents erroneous readings of filling problems in the collecting system.
- At this time, radiographs are done to check that the catheter is properly placed.
- After confirming placement, the physician may administer the contrast through the catheter. To thoroughly opacify the ureter and renal collecting system, 5-8 mL of contrast is often required. Several fluoroscopy pictures are captured while the contrast is being injected.
Three films are taken during the procedure
- A scout film (without contrast media): to check the technique, position, and placement of the ureteral catheters
- 3 to 5 ml of contrast is injected where the film demonstrating the renal pelvis and calyces is taken
- Withdrawing of the catheter and film of the contrast-filled ureters is taken.
After Procedure
- Following the procedure, the patient will be brought to the recovery room to be monitored. If the patient is conscious, blood pressure, pulse, and respiration are stabilized, the discharge process can be initiated.
- The patient’s urine output will be constantly monitored for volume and evidence of blood.
- The patient may experience discomfort while urinating. Analgesics may be prescribed.
- The patient should notify the physician if any following clinical signs are present.
- Fever or chills
- Redness, swelling, and bleeding or other drainage from the urethra
- Increased pain around the urethra
- Increase in the amount of blood in the urine
- Trouble urinating
Complications
- Pyelovenous backflow
- Backflow occurs when contrast is injected at high pressure and escapes from the collecting system.
- The introduction of microorganisms into the circulation from potentially contaminated urine and the chance of an allergic reaction to the contrast are the two key concerns with this complication.
- To avoid this problem, clinicians should make every effort to provide contrast at low pressure.
- Furthermore, suitable preoperative antibiotics should be given.
- Extravasation of contrast
- Under high pressure, forniceal ruptures of renal calyces can occur, resulting in contrast extravasation.
- This is visible with fluoroscopy and can result in bleeding and/or infection.
- Forniceal ruptures usually heal on their own following decompression.
- Complications of general anesthesia
- Chemical pyelitis if there is stasis of contrast medium
- Mucosal damage to the ureter
- Perforation of the ureter or pelvis by the catheter
- A contrast medium may be absorbed from the renal pelvis which gives rise to adverse reactions
Antegrade pyelogram
- Antegrade pyelography is the administration of radiopaque contrast material into the kidney and collecting system by a percutaneously placed needle or catheter system.
- Because of the present availability of less invasive radiographic procedures (e.g., intravenous urography, ultrasonography, magnetic resonance imaging, computed tomography, retrograde investigations), it is seldom performed alone, although it is a frequent step toward more complex endoscopic interventions.
- It is the procedure that assesses the upper collecting system fluoroscopically by infusing water-soluble contrast through the nephrostomy catheter.
Indications
- Vesicoureteral reflux
- Study of the urethra during micturition
- Abnormalities of bladder
- Stress incontinence
- To check for extravasation, filling defects (such as residual stones or hematomas), the bladder’s upper tract collecting system’s patency, and the proper placement of PCN (Percutaneous Nephrolithotomy)
Contraindication
- Acute UTI
- Hypersensitivity to contrast
- Fever within the past 24 hours
Procedure
Patient Preparation
- The procedure should to be explained to the patient, and consent should to be obtained.
- Coagulation tests are not required if the antegrade puncture is simply being performed for diagnostic or drainage purposes unless clinically indicated.
- However, a hematocrit assessment and coagulation investigations are advised prior to the treatment if more extensive modifications are planned.
- If there is evidence of a urinary infection or if a plan is afoot to enlarge the urinary system or remove stones, antibiotics are advised.
- Commonly, an aminoglycoside and ampicillin combination are given an hour before the surgery.
- In order to reduce anxiety but still allow for complete patient compliance, the treatment is typically performed under local anesthetic and light sedation.
During Procedure
- The procedure for antegrade pyelography is done under local anesthesia, except for children who could need sedation. The sole absolute contraindication to the procedure is untreated bleeding diatheses.
- With the patient laying prone or prone oblique, the examination is performed under fluoroscopic guidance.
- When lying flat, the collecting system may be accessed immediately posteriorly from behind the 12th rib without the need to angle the needle.
- Although this method is more challenging, it does allow for a larger transcortical passage of the needle since the cortex creates a strong seal around the needle, lowering the risk of extravasation and enhancing the usefulness of pressure readings. The patient is more at ease when they are lying prone-oblique as opposed to prone.
- By using ultrasound, CT, or intravenous contrast agents, the collecting system may be localized.
- The collecting system in the non-functioning kidney cannot be localized properly after intravenous contrast. Thus, imaging with ultrasonography or CT, which is independent of renal function, is required. However, CT is seldom applied in real life. Real-time ultrasound devices are more portable and user-friendly than CT, and they often resolve mildly dilated calyces better.
- Ultrasound can also be used to track the progress of the needle as it approaches the collecting system.
- However, in the presence of significant obstruction, pelvicalyceal pressures may be considerably elevated by diuresis and intravenous contrast may be potentially hazardous.
- Following IV contrast in the functioning kidney, there is a diuretic effect that may increase the degree of calyceal dilatation, making puncture slightly easier. The preferred technique is ultrasound.
- An appropriate antiseptic is used to prepare the skin, and a tiny plunge incision is performed after the local anesthetic has been injected into the puncture site.
- The patient should be in suspended respiration when a 22-gauge flexible needle is used to puncture the collecting system.
- It should be pointed towards the main calyx. As soon as the needle enters the collecting system, there is a tiny “give,” and aspirating urine or pus from a pyonephrosis verifies the needle’s proper location.
- The needle and a flexible tube are attached to a manometer, and the zero point of the manometer is placed level with the needle tip to measure the resting pelvic calyceal pressure (typically less than 10 cm H2O).
- To conduct cytological, bacteriological, and biochemical research, a sample of pus or urine is collected.
- Particularly if the urine is contaminated or the resting intrapelvic pressure is high, the volume of contrast medium that is injected should not be greater than the volume of urine that is aspirated (more than 22 cm H2O)
- To prevent hiding minor obstructing intraluminal or mural lesions during fluoroscopy, a contrast medium with low iodine content (such as Urografin 150) is utilized.
- Spot films showing the appropriate anatomical features and anomalies are displayed. Finding obstructing lesions may be easiest while the patient is upright. If it is discovered that the collecting system is entirely blocked, as much contrast as possible is injected.
After Procedure
- The follow-up of the antegrade pyelogram is the same as that of the retrograde pyelogram.
Complications
The following are some antegrade pyelogram potential complications:
- Bleeding
- Sepsis
- Reaction to the contrasting material
- Mild reactions include nausea, vomiting, and hot flashes
- More severe complications like breathing difficulties, hypotension, and swelling of the mouth can occur
- A cyst filled with urine developing (urinoma)
- Blood clots in the bladder or, if a nephrostomy tube is utilized, in the tube itself
Summary
- Pyelogram is a radiologic procedure used to assess the genitourinary system most specifically the kidneys, ureters, and bladder with the use of radiopaque material.
- Types of pyelograms are IVP, retrograde pyelogram, and antegrade pyelogram.
- An IVP is the radiographic examination of the urinary tract including the renal parenchyma, calyces, and pelvis after the intravenous injection of the contrast media.
- Retrograde pyelogram involves injecting contrast material directly into the ureters retrogradely following their cystoscopic cannulation to observe the collecting system and the ureter without relying on renal contrast excretion.
- Antegrade pyelography is the administration of radiopaque contrast material into the kidney and collecting system by a percutaneously placed needle or catheter system.
References
- Cheuck, L. (2019, January 16). Retrograde pyelography. Medscape. Retrieved 2023, January 20 from https://emedicine.medscape.com/article/2113562-overview
- Dale, J., Gupta, R. T., Marin, D., Lipkin, M., & Preminger, G. (2017). Imaging advances in urolithiasis. Journal of Endourology, 31(7), 623-629. https://www.liebertpub.com/doi/abs/10.1089/end.2016.0695
- Djajadiningrat, R. S., Walz, J., van Dijk, L. C., & Roshani, H. (2020). Antegrade pyelography, a survey among urologists. Irish Journal of Medical Science (1971-), 189(3), 843-848. https://link.springer.com/article/10.1007/s11845-020-02180-z
- Krantz, T. E., McFerren, S. C., Riley, J. M., Dunivan, G. C., & Alba, F. M. (2019). Tips and Tricks for Performing a Retrograde Pyelogram. Urology, 129, 234. https://www.sciencedirect.com/science/article/abs/pii/S0090429519303322
- Mallya, A., Karthikeyan, V. S., Manohar, C. M. S., & Keshavamurthy, R. (2019). Bilateral retrograde pyelography leading to anuria. National Medical Journal of India, 32(1). Doi: 10.4103/0970-258X.272110
- Mathur, M. (2022, December 1). Urography. Medscape. Retrieved 2023, January 20 from https://emedicine.medscape.com/article/1890669-overview#a1
- Mehta, S. R., & Annamaraju, P. (2022, Jan). Intravenous Pyelogram. StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK559034/
- Siraj, R., Shamim, B., Mansoor, M. A., Ali, I., Kumar, A., & Siraj, M. I. (2021). Effect of Intravenous Pyelogram on Vital Parameters: A Study Focusing on Complications. Asian Journal of Research in Medicine and Medical Science, 55-61. https://www.globalpresshub.com/index.php/AJRMMS/article/view/1332/1105