Introduction
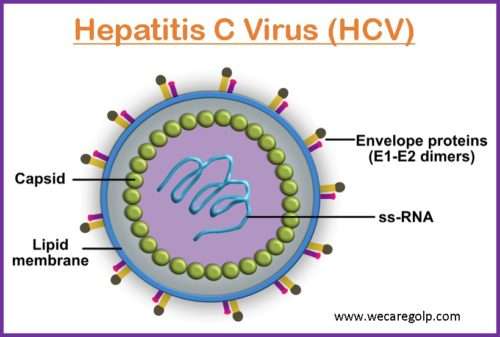
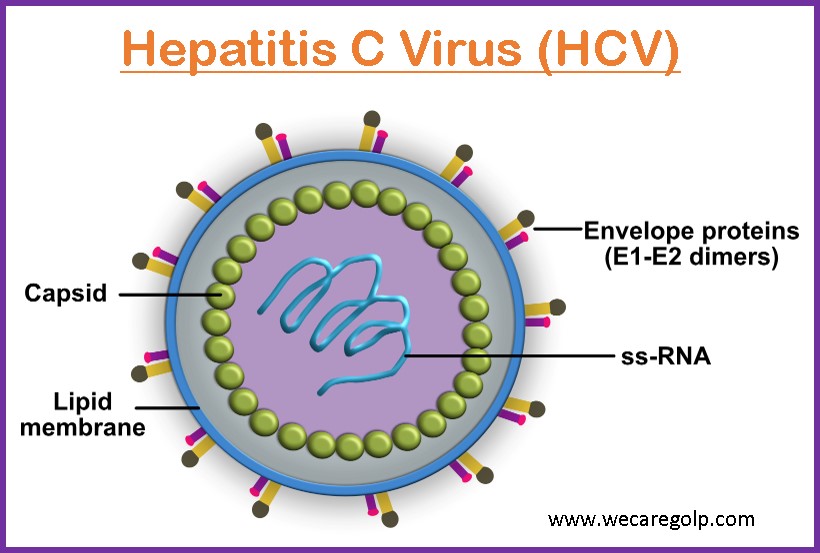
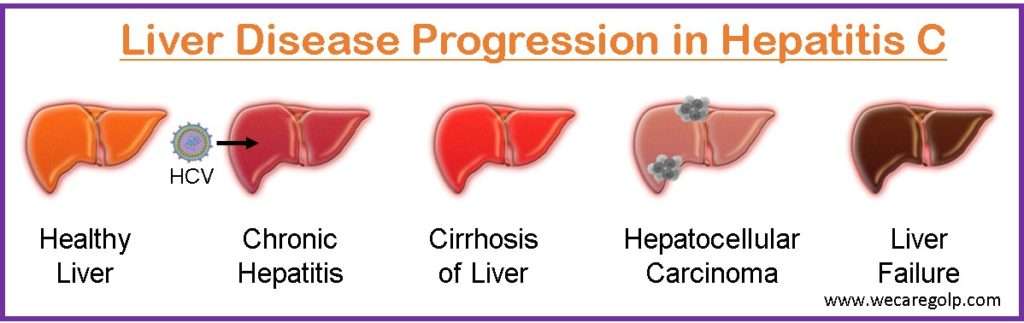
Hepatitis C is a contagious liver disease that results from infection with the hepatitis C virus (HCV). HCV is a hepatotropic RNA virus that belongs to the family Flaviviridae. HCV causes progressive liver damage, which might result in liver cirrhosis and hepatocellular carcinoma.
- It is the most common virus infecting the liver and is considered a major cause of parenterally transmitted hepatitis.
- Infection with HCV remains chronic in 70-80% of the infected individuals.
- There are eight known hepatitis C genotypes distributed across different regions. At the global level, most infections are caused by genotype 1, followed by genotypes 3, and genotypes 2 and 4.
- There is no prophylactic vaccine or specific immunoglobulin against it.
- Effective antiviral treatment exists which results in an effective prognosis for the disease.
Types of Hepatitis C
Acute Hepatitis C
- It is a short-term infection where symptoms can last up to 6 months.
- Most people do not show any symptoms during this phase, some do have symptoms and the illness is so mild that they do not even recognize having the liver disease.
- The immune system fights off the infection from the body and virus goes away and liver heals completely.
Chronic Hepatitis C
- When a body is unable to fight off the virus and the infection persists for more than six months, the persistent state is known as chronic hepatitis C.
- The liver becomes more inflamed and scared over years.
- Early diagnosis and treatment of chronic hepatitis can prevent liver damage.
Incidence
- According to WHO the highest burden of disease is seen in the Eastern Mediterranean Region and European Region, infecting 12 million people chronically in each region.
- Globally 58 million people are infected with chronic hepatitis C, with about 1.5 million new infections occurring per year.
- Around 3.2 million adolescents and children are diagnosed with chronic infection.
- As per WHO, approximately 290,000 people died from hepatitis, because of end-stage liver disease (cirrhosis and hepatocellular carcinoma) in 2019.
- In the United States, HCV is the most common cause of chronic hepatitis.
Causes of Hepatitis C
- Hepatitis C is caused by the hepatitis C virus (HCV) and the infection spreads through contaminated blood and body fluids.
Risk Factors of Hepatitis C
- Injecting street drugs or sharing a needle with infected people
- Having dialysis for a long period
- Having regular contact with blood at work (health care worker)
- Having unprotected sex with an infected person
- Baby born from HCV-infected mother
- Receiving tattoos or piercing with unsterilized needles
- HIV infected patient
- Organ transplant patients
Mode of transmission
HCV is commonly transmitted through
Parenteral
- Transfusion of infected blood or its products.
- Using non-sterile syringes, needles, and medical instruments.
- Transplantation of infected donor organs or tissues.
- Occupational exposure with infected blood.
Sexual
- The risk is higher among persongs having multiple sex partners.
Mother to child
- The chance of vertical transmission of HCV is about -7%. The risk increases if HCV viral load in the mother’s blood is high.
Incubation Period
- The incubation period for hepatitis C is 2 weeks to 6 months.
Signs and Symptoms of Hepatitis C
Following initial infection, approximately 80% of people do not exhibit any symptoms.
Acute Hepatitis C
- Fever
- Fatigue
- Decreased appetite
- Nausea
- Vomiting
- Abdominal pain
- Dark urine
- Grey colored feces
- Joint pain
- Jaundice
Chronic Hepatitis C
- Ascites
- Easy bleeding
- Easy bruising
- Hepatic encephalopathy-confusion, drowsiness, and slurred speech
- Jaundice of the skin
- Hives or rashes
- Itchy skin
- Spider angiomas-spidery blood vessels under your skin.
- Swollen legs
- Weight loss
Pathophysiology of Hepatitis C
- HCV enters a susceptible host either directly, through inoculation or transfusion of contaminated blood, or breakage of a percutaneous barrier.
- The hepatitis C RNA virus enters the hepatocytes or other susceptible cells, through unique surface molecules or molecules, as the viral receptor.
- After uptake, the virus uncoats and releases the genome to begin replication. The viral genome serves as the template for translation of the polyprotein.
- The processed nonstructural proteins then form a complex with the genome and initiate synthesis of the negative strand synthesis.
- The replication complex resides in a membranous compartment in the cytoplasm, derived from the endoplasmic reticulum.
- The RNA replicative intermediate matures and interacts with the core and envelope proteins to assemble into a virion.
- Some non-structural proteins play critical roles in viral replication and produce infections.
Diagnosis of Hepatitis C
Different test helping in the diagnosis includes
Blood test
- A series of blood tests include complete blood count, Glomerular Filtration Rate (GFR), thyroid function, INR, prothrombin time, etc..
- Enzyme immunoassay (EIA) helps in detecting HCV antibodies.
- A PCR test helps in identifying the activeness of the virus and measuring the amount of virus in the blood.
Genotype test
- It reveals which hepatitis C genotype is present for the selection of an effective treatment approach.
Liver function test
- Normal AST, ALT, PT, and albumin become abnormal if cirrhosis occurs.
Liver biopsy
- A small piece of tissue from liver is taken and sent as a sample for cell abnormalities.
- It helps in identifying liver damage.
Magnetic resonance elastography (MRE)
- It combines magnetic resonance imaging (MRI) technology with patterns formed by sound waves bouncing off the liver showing gradients of stiffness of the liver.
- Stiff liver tissue indicates scarring of liver tissues.
Transient elastography
- It is an ultrasound that transmits vibration into the liver and measures the speed of dispersal through liver tissue to estimate its stiffness.
Treatment of Hepatitis C
It does not always require treatment because some people’s immune response will clear the infection and some people with chronic infection do not develop liver damage.
Alpha interferon
- It is a host protein that is made in response to viral infection and has an antiviral capacity.
Combination therapy
- A combination of anti-viral therapy with interferon and ribavirin has been the mainstay of treating Hepatitis C which requires weekly injections for 48 weeks.
Direct antiviral agents (DAAs)
- Recently developed antiviral drugs called DAAs are more effective, safer, and better tolerated.
- This therapy cures most persons with HCV infection and treatment is shorter usually 12 weeks.
Complications
Delaying in diagnosis and long-term untreated infection can result in the following complications.
Cirrhosis
- It is a condition in which liver slowly breaks down and is unable to function normally.
- Scar tissues replace the healthy liver tissue and partially block the blood flow through the liver.
Liver failure
- It is an end-stage liver disease where the liver can no longer perform functions or replace damaged cells.
Liver cancer
- Hepatitis-associated cirrhosis increases the risk of liver cancer.
Prevention
There is no vaccine available to prevent hepatitis C. However, the preventive measures can be the following.
- Avoiding injecting drugs through unsterilized injection.
- Following universal precautions and safely handle needles and other sharps instruments.
- Avoiding sharing personal care items that might contain blood on them such as razors, and toothbrushes)
- Using latex condoms every time to prevent the spread of infections.
- Tattooing and piercing through sterilized needles only.
- Avoiding direct exposure to blood infected with hepatitis C.
- Educating people at high risk for infection (people infected with HIV, or immunocompromised diseases)
- Immunization with hepatitis A and hepatitis B vaccines to prevent co-infection from the hepatitis virus to protect the liver.
- Regularly monitoring and testing for the diagnosis of chronic liver disease.
Prognosis
- The prognosis for most people with hepatitis C who receives treatment is good.
- The prognosis depends on the type of virus causing it. Many people may not know they are having hepatitis C infection, half of the cases clear on their own.
- For chronic infection, the prognosis depends on a person’s overall health, the degree of liver damage, how soon treatment is received, and response to treatment.
- Drug therapies are improving the success rates of the treatment. Additionally, early diagnosis improves the prognosis.
- It can be a lifelong infection if left untreated and cause serious health problems including liver damage, cirrhosis, liver cancer, and even death.
Hepatitis C and Pregnancy
- Most women with hepatitis C who become pregnant have a healthy pregnancy in which HCV does not transmit to the fetus.
- An increased risk of undesirable consequences for the fetus including low birth weight and fetus growth restriction is associated with infection during pregnancy.
- Hepatitis C during pregnancy can cause cholestasis of pregnancy, where bile acids accumulate and lead to itching and sometimes adverse fetal outcomes.
- The chance of HCV transmission from pregnant mother to fetus is about 5%.
- HCV can be transmitted to the infant in utero or during the labor or postpartum period through contact with the blood.
- The CDC recommends screening all pregnant persons for Hepatitis C infection during each pregnancy so that risk stratification can be performed and measure is taken to reduce perinatal transmission.
- Pregnant women and nursing mothers should avoid taking any of the currently available HCV treatments.
- All the infants of HCV-positive mothers are tested when the baby is at least 18 months old because the baby will have maternal antibodies in their blood which can lead to a false positive when it is done too early.
- Babies becoming infected with HCV will need regular monitoring and ongoing medical care.
Summary
- HCV causes a liver infection called hepatitis C.
- The infection can be transmitted through infected blood or body fluids and may be transmitted during child birth, through IV drug, and sexual intercourse.
- It can cause both acute and chronic hepatitis C ranging from mild to serious, lifelong illness.
- It is diagnosed by testing for the presence of HCV antibodies and HCV RNA.
- Most people are not aware of their infection because they do not possess any symptoms.
- The best way to prevent HCV infection is by avoiding behavior that can spread the disease.
References
- Chaudhari, R., Fouda, S., Sainu, A., Pappachan, J.M. (2021, Apr 7) Metabolic complications of hepatitis C virus infection. World journal of gastroenterology, 27(13):1267-1282. doi: 10.3748/wjg.v27.i13.1267
- Society for Maternal-Fetal Medicine (SMFM). Hughes, B.L., Page, C.M., Kuller, J.A. (2017, Nov 1). Hepatitis C in pregnancy: screening, treatment, and management. Am J Obstet Gynecol, 217(5), B2-B12. doi: 10.1016/j.ajog.2017.07.039. Epub 2017 Aug 4. PMID: 28782502.
- Basit, H., Tyagi, I., Koirala, J. (2022 Nov 26). Hepatitis C. StatPearls Publishing; 2022 Jan-. Retrieved 2023, Jan 4 from: https://www.ncbi.nlm.nih.gov/books/NBK430897/
- Manns, M.P., Buti, M., Gane, E., Pawlotsky, J.M., Razavi, H., Terrault, N., Younossi, Z. (2017, Mar 2). Hepatitis C virus infection. Nat Rev Dis Primers, 3,17006. doi: 10.1038/nrdp.2017.6
- Maness, D.L., Riley, E., Studebaker, G. (2021, Dec 1). Hepatitis C: Diagnosis and Management. Am Fam Physician, 104(6),626-635. PMID: 34913652.
- Center for Disease Control and Prevention. (2020, July 28). Hepatitis C. Retrieved 2023, Jan 4 from https://www.cdc.gov/hepatitis/hcv/index.htm