Introduction
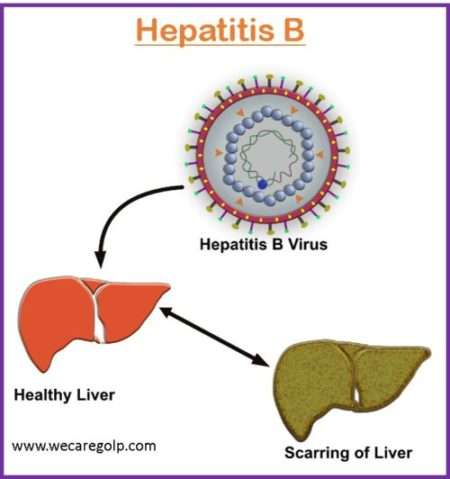
Hepatitis B is a serious and common infectious disease of the liver caused by a Hepatitis B virus (HBV), an enveloped virus containing a partially double-stranded DNA genome belonging to the ‘Hepadnaviridae’ family
- HBV is a non-cytopathic hepatotropic virus with the potential to cause a persistent infection leading to chronic hepatic insufficiency, cirrhosis, and hepatocellular carcinoma (HCC).
- Hepatitis B is a “silent epidemic” as asymptomatic HBV carriers can spread the disease for many years.
- Despite of availability of preventable vaccine, chronic hepatitis B (CHB) infection affects approximately 296 million individuals worldwide.
Incidence
- According to the WHO, approximately 296 million people were living with CHB infection in 2019, and 1.5 million new infections each year around the world.
- It contributes to an estimated 820,000 deaths every year, mostly from cirrhosis and hepatocellular carcinoma.
- Its prevalence is high in the WHO Western Pacific Region and WHO African Region, where 116 million and 81 million people are infected respectively, and also remains disproportionately high in low and middle-income countries, particularly in Asia and Africa.
Types of Hepatitis B Infection
There are two types of hepatitis B infections:
Acute Hepatitis B Infection
- It is the initial phase of the HBV infection.
- Many people do not show any symptoms during this phase and for those who have symptoms the illness is usually mild.
- The virus eliminates from the body within 6 months and liver heals completely and the person becomes immune to hepatitis B infection for the rest of his life.
Chronic Hepatitis B Infection
- Chronic hepatitis B (CHB) infection occurs when the immune system is unable to eradicate the virus and the infection persists for at least six months.
- It can lead to cirrhosis (scarring) of the liver, liver cancer, and liver failure.
- Infants born to mothers infected with HBV are at high risk of developing CHB infection.
Causes of Hepatitis B
The hepatitis B virus (HBV) causes hepatitis infection. Infected blood, sperm, or bodily fluids carry the virus from one person to another.
Risk Factors of Hepatitis B
- Children born to hepatitis B virus-infected mother
- Anyone who has come in direct contact with hepatitis B virus-infected bodily fluids (semen, vaginal secretions, blood)
- People who had unprotected sex with infected persons
- Intravenous drug abusers
- People working or living in a place where there is high exposure to infected blood such as health care institutions or correctional facilities.
- People having multiple sex partners
- Men having sex with men
- People living in close quarters with a person with chronic hepatitis infection
- People who are on predialysis and dialysis (including home dialysis, hemodialysis, and peritoneal dialysis)
- People with hepatitis C and HIV infection
- People with diabetes at the discretion of the treating clinician
- Individuals born in countries where it is common (Asia, Africa, South America<Eastern Europe, Pacific Islands, and Middle East).
- International travelers to countries with high or intermediate levels of endemic HBV infection (HBsAg prevalence of ≥2%)
- All pregnant women
Mode of Transmission of Hepatitis B
The hepatitis virus is often transmitted through the blood and sexual fluids. Most commonly the transmission can occur in the following ways:
- Sharing of needles-People sharing contaminated needles and syringes easily get infected with Hepatitis B Infection.
- Sexual contact-People having unprotected sex with an infected person easily get the infection because the virus can pass if the infected person’s blood, saliva semen, or vaginal secretion enters the body.
- Mother to the child-The virus can pass to the babies from the infected pregnant women or during childbirth.
- Accidental needle sticks– It transmits to the person who comes in direct contact with infected blood.
Incubation Period
- According to WHO, the incubation period of the HBV ranges from 30 to 180 days.
- The virus may be detected within 30 to 60 days after infection and can persist and develop into CHB when transmitted in infancy or childhood.
Symptoms of Hepatitis B
Symptoms of Acute Hepatitis B
There are three phases of acute hepatitis B and symptoms occur depending on the stage
Initial stage (Prodromal stage)
- Fever
- Joint pain or arthritis
- Rash
- Edema
Preicteric phase
- Fatigue
- Loss of appetite
- Nausea
- Vomiting
- Fever
- cough
- Abdominal pain
- Dark urine
- Clay-colored bowel movements
Icteric phase
- Jaundice
- Anorexia, Nausea, and vomiting may worsen.
- Irritated skin lesions may develop
Symptoms of Chronic Hepatitis B
Most patients with chronic infections are asymptomatic unless their disease progress.
Some patients experience worsening of the infection and develop signs and symptoms similar to acute hepatitis.
When a patient with chronic hepatitis progress to cirrhosis they will develop signs and symptoms of liver failure including-
- Jaundice
- Splenomegaly
- Ascites (fluid retention in the abdomen)
- Peripheral edema
- Encephalopathy- when the liver is not working properly, toxins will not get clear from the body and get build up in the blood affecting the functions of the brain and leading to confusion)
- Hepatocellular carcinoma.
Pathophysiology of Hepatitis B
- The HBV is transmitted through percutaneous inoculation or mucosal exposure to infectious body fluids.
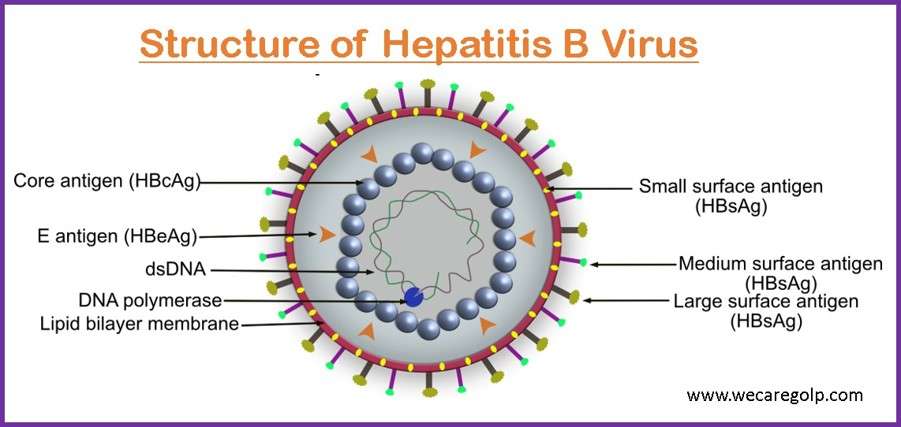
- The virus, also referred as Dane particles, is constructed of an outer capsule containing HBsAg (hepatitis B surface antigen), an inner core containing HBcAg (hepatitis B core antigen)) and HBeAg (hepatitis B e-antigen).
- As the blood gets exposed to HBV, HBsAg and other nucleocapsid proteins on cell membranes promote a cell-mediated immune response by sending cytotoxic T cells and natural killer cells to the virus and releasing inflammatory cytokines. The greater the immune response, the greater the chance of fighting with the virus.
- When HBV infiltrates and enters hepatocytes, they appear as “ground glass” on histological examination because HBsAg invades the cytoplasm of the cell- this distinguishes HBV from other forms of hepatitis.
- As the hepatocytes continue to proliferate, the HBV is continuously shed into the blood, promoting chronic infection.
Diagnosis of Hepatitis B
It begins with medical history assessment and physical examination. Following investigation is done for analysis of other findings related to the infection.
Blood Tests
Antibody/antigen tests
- The detection of viral DNA in replicating virus by PCR is more sensitive.
- The antigen detection and PCR prove the presence of the replicating virus.
- The antibodies detect an immune response of the host.
- Antibody detection (anti-HBc only in the long-term) is possible even in a recovered person.
- Antibody/antigen tests are
- HBsAg
- Anti-HBs
- Anti-HBc
- Anti-HBe
- Anti-HBc IgM and IgG
Aminotransferase (ALT)
- It is considered as best liver enzymes test for detecting hepatitis.
- Typically, elevation occurs prior to other symptoms like jaundice.
Alkaline phosphatase (ALP)
- Usually slightly elevated unless the severe biliary obstruction is present.
Complete blood count
- RBC is decreased because of the shortened life span of RBCs-liver enzyme alterations or hemorrhage.
- WBCs may be abnormally low(leucopenia) or high (leukocytosis), monocytes may be increased (monocytosis) and lymphocytes may be increased and atypical in appearance.
Serum Albumin
- Measures the main body protein manufactured by the liver, its level may increase.
Prothrombin time
- Evaluates the body’s ability to produce a clot in a reasonable amount of time, which may be prolonged due to liver dysfunction.
Serum Bilirubin
- Increased level indicates the liver is incapable of adequate removal of bilirubin on time due to blockage of bile ducts or liver diseases, such as acute hepatitis.
Diagnostic Test related to Liver
Liver scan
- It is done to identify underlying chronic liver disease, or for evaluating organ function.
- It helps to estimate the severity of parenchymal damage.
Liver Biopsy
- It is considered if the diagnosis is uncertain or if a clinical course is atypical or prolonged.
- It provides an initial assessment of disease severity.
Urinalysis
- Urine test shows elevated bilirubin levels, proteinuria and hematuria may occur.
Stool Analysis
- Clay-colored stools indicate a lack of normal bile excretion into the intestine.
Treatment of Hepatitis B
- Supportive treatment is provided to people with acute infections depending on their symptoms.
- For the majority of people, the symptoms resolve and a person can clear the infection within 6 months.
- People with CHB are monitored regularly for signs of liver diseases and need possible treatment to stop or reduce the activity of the virus from damaging the liver by limiting the replication of the virus.
- Treatment helps to reduce the risk of liver disease and prevents passing infections to others.
- When the liver is severely damaged, liver transplantation is necessary.
Treatment with medications
Alpha –interferon
- It is the single modality of therapy that is used to treat CHB.
- A regimen of 5 million units daily or 10 million units three times a week for 16 to 24 weeks results in the remission of disease in approximately one-third of patients.
Lamivudine (Epivir)
- It is an antiviral agent that has revealed improved seroconversion rates, loss of detectable virus, improved liver function, and reduced progression to cirrhosis of the liver.
- Decompensated cirrhosis patients who are awaiting liver transplantation may benefit from it.
Adenovir (Hepsera)
- It may be effective in patients who are resistant to lamivudine.
Antacids and Antiemetics
- It helps to control dyspeptic symptoms and general malaise.
Interferon injections
- Interferon alfa-2b (Intron A) is a man-made version of the substance produced by the body to fight against infection.
- It is mainly used for people with hepatitis B who wish to avoid long treatment or women who want to get pregnant within a few years, after completion of the course of therapy.
Complications of Hepatitis B
Many people with hepatitis B infection do not feel sick or even know they have it unless it is in the last stage but some people may have serious complications. It can lead to
- Cirrhosis or scarring of the liver– The Hepatitis B infection can lead to extensive liver scarring (cirrhosis), which may impair the liver’s ability to function.
- Liver cancer-People with CHB have an increased risk of liver cancer.
- Liver failure– In acute liver failure, the liver’s essential functions stop working. For survival, a liver transplant is necessary.
- Kidney diseases- It can lead to various kidney diseases.
- Blood vessels problems– It leads to inflammation of blood vessels.
- Reactivation of the hepatitis B Virus-People with CHB who have suppression of their immune system is prone to reactivation of the hepatitis virus. This can lead to significant liver damage or even failure.
Prevention of Hepatitis B
- Infants born to mothers positive for HbsAg should receive both HBIG and the first dose of hepatitis B vaccine, optimally within 4 hours of birth.
- Use new latex condoms every time you have sex.
- Avoid sharing personal care items that have blood on them like razors, toothbrushes
- Healthcare or public safety worker should follow universal blood/body fluid precautions and safely handle needles and others sharps.
- Be cautious while tattooing, body piercing, or acupuncture about the sterility of the instrument used for doing it.
- Active Immunization (Hepatitis B vaccine) can protect from the infection.
Vaccine

The hepatitis B vaccine provides long-term protection against HBV infection.
- The World Health Organization (WHO) recommends HBV for
- All newborns
- Children up to the age of 18
- Adults at higher risk for infection.
- The U.S. Centers for Disease Control and Prevention (CDC) recommends the hepatitis B vaccine for
- All newborns
- Children up to age 18
- Adults 19-59 years of age
- Adults 60 and older who are at high-risk for infection
- The vaccine is also suggested for everyone who is at a high risk (see above) of getting the virus.
- The vaccine is administered intramuscularly in 3 doses. The third dose is very important for producing prolonged immunity.
- Dose 1: 0 month
- Dose 2: 1 month after first dose
- Dose 3: 6 months after first dose
- Moreover, hepatitis B vaccination is recommended for pre-exposure and post-exposure prophylaxis. If administered immediately after (or within seven days of) exposure to the infection, HBIG may be effective for unvaccinated individuals.
Vaccine and Dialysis Patients
- In dialysis patients, the vaccination results are poor because of immune deficiency. Therefore, serological success controls are necessary.
- Furthermore, dialysis patients get double vaccine doses.
- Nevertheless, around 20% of those vaccinated do not develop a protective antibody response.
- Anti-HBs is formed as a vaccine antibody, which provides secure immunity to infection.
- If the antibody titer falls below 100 IU/l, a regular booster dose is indicated.
- Patients who never develop a protective antibody titer should receive a maximum of 6 individual injections, after which further vaccinations are not promising.
- Successfully vaccinated patients (anti-HBs > 10 IU/l) can be dialyzed together with hepatitis B virus carriers.
Prognosis
- Some people may rapidly improve acute hepatitis B, while others may have a prolonged disease course with very slow improvement over several months, or with periods of improvement followed by worsening of symptoms.
- A small group of people (about 1% of infected people) suffer rapid progression of their illness during the acute stage and develop severe liver damage (fulminate hepatitis), which may occur for several days to weeks and may be fatal.
Hepatitis B and Pregnancy
- Pregnant women infected with the HBV virus infection pose a serious risk to their infant at birth.
- Babies born to a mother infected with Hepatitis B have a greater than 90% chance of developing CHB if they are not treated properly.
- When babies become infected with hepatitis B, they have a higher chance of developing lifelong, chronic infection, if left untreated 1 in 4 children who have chronic hepatitis will eventually die due to health problems related to their infection.
- Pregnant mother needs to know their Hepatitis B status so that precaution can be maintained during delivery to prevent passing the virus on to their baby.
- At their first prenatal visit, all pregnant women should be tested for HBV, according to the CDC.
- HbsAg-positive women with high viral loads (>200,000 IU/ml) should receive tenofovir between 28-32 weeks of gestation, to reduce the risk of perinatal transmission.
- WHO and CDC recommend that neonates born to mothers with HBV should receive HBIG as well as the HBV vaccine within 24 hours of birth for an infant who has received HBIG and HBV vaccine, breastfeeding is safe.
- Routine administration of all infants with the hepatitis B vaccine series, with the first dose administered within 24 hours of birth is recommended.
Summary
- Hepatitis B is a potentially serious viral infection of the liver and is acquired through contact with infected blood, blood products, or other body fluids.
- It remains a major contributor to the global burden of disease despite access to and adoption of the vaccine. It is the most common serious liver infection in the world.
- Virus attacks and injures the liver and causes the liver to swell and prevents it from working.
- Persistent HBV infections can lead to severe liver diseases including liver cirrhosis and cancer, which can eventually lead to death.
- Proper screening, vaccination, and post-exposure prophylaxis are key interventions to reduce the infection.
References
- Iannacone, M., Guidotti, L. G. (2022, Jan). Immunobiology and pathogenesis of hepatitis B virus infection. Nat Rev Immunol,22(1):19-32. doi: 10.1038/s41577-021-00549-4.
- Terrault, N. A., Lok, A.S.F., McMahon, B.J., Chang, K., Hwang, J. P., Jonas, M. M., Brown, R. S., Bzowei, N. H., Wong, J. B. Wong. (2018, Feb 5). Update on prevention, diagnosis, and treatment of chronic hepatitis B: AASLD 2018 hepatitis B guidance. Hepatology, 67 (4), 1560-1599. https://doi.org/10.1002/hep.29800
- Hepatitis B. Am Fam Physician. 2019 Mar 1;99(5): Online. PMID: 30811170.
- Dekker, S. E., Green, E. W., Ahn, J. (2021, Nov). Treatment and Prevention of Acute Hepatitis B Virus. Clin Liver Dis,25(4):711-724. doi: 10.1016/j.cld.2021.06.002
- WHO Guidelines on Hepatitis B and C Testing. Geneva: World Health Organization; 2017 Feb. EXECUTIVE SUMMARY. Available from: https://www.ncbi.nlm.nih.gov/books/NBK442292/