Peritoneal Dialysis
Peritoneal dialysis (PD) is a renal replacement procedure for the treatment of renal insufficiency.
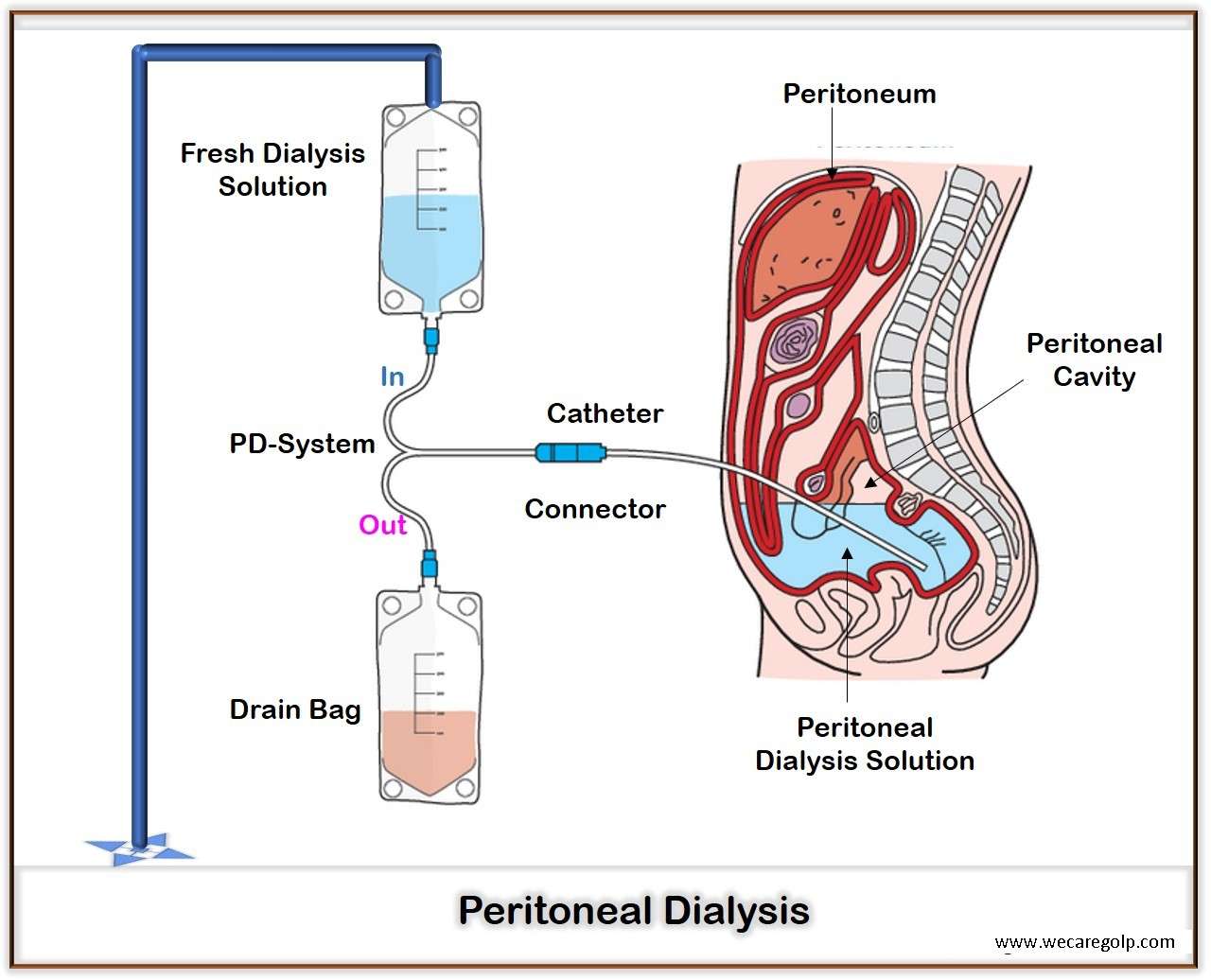
- PD is a procedure to remove waste products (such as creatinine and urea) and extra water through the blood vessels that line the walls of the abdomen when the kidneys are no longer working effectively. The lining of the abdomen called the peritoneum acts as a dialysis membrane.
- This procedure filters the blood in a different way than does the more common blood-filtering procedure called hemodialysis.
- It does not cure or treat the underlying kidney disease like hemodialysis (HD). However, it is intended to replace as many functions of the failing kidneys as possible.
Principle of Peritoneal Dialysis
- Uremia toxins and water take up from the blood of the peritoneal capillaries by a solution let into the abdominal cavity, the PD solution, and removed with it after a specific residence time.
- The PD solution contains electrolytes, buffers and osmotically active molecules, mainly glucose.
- Parietal and visceral peritoneum act as a semipermeable membrane. Molecules and water transfer occur by diffusion and osmosis.
- Filled volume is 1.5 to 2.5 L in the abdomen.
- The UF of water can vary by the concentration of the osmotic agent in the PD solution.
- Final removal of ultrafiltrate and solute occurs at the time by draining the dialysate to the outside.
Procedure of Peritoneal Dialysis
- A soft catheter places a few weeks before a patient start treatment on the abdomen by surgery.
- The patient will train on how to do PD once the surgery area heals.
- The catheter will use transfer the dialysis solution (dialysate) from a bag into the abdominal cavity and use to drain it out.
- The dialysate contains water with electrolytes and salt. It soaks up extra fluids and wastes from the body with the help of the osmosis and the diffusion process.
- The dialysate remains in the abdominal cavity for a few hours called the dwell time.
- After the dwell time or the filtering process is finished, the dialysate with filtered wastes and extra fluid will drain into an empty bag. This process is called an exchange.
- The number of exchanges and amount of dwell time depends on the method of PD you use and other factors.
- When the abdominal cavity is empty, fresh dialysis solution will again fill in the abdominal cavity.
- When the fresh dialysate bag is empty, the catheter will disconnect and place a cap on the catheter so you can move around and do your normal activities.
- While the dialysis solution is inside your abdomen, it absorbs wastes and extra fluid from the body.
- You can throw away the drained solution in a toilet or tub.
- In this way, the process will repeat further. The emptying and refilling process can take 20 to 30 mins and can do four or six times every day.
- The exchanges can perform during the daytime, or at night using a machine that pumps the fluid in and out.
Indications of Peritoneal Dialysis
- Patient request, professional rehabilitation, home dialysis without a partner
- Cardiac instability
- Lack of vascular access
- Bleeding complications under Hemodialysis (HD)
- Terminal renal failure in childhood
- Hypotonic circulatory conditions under HD
- Heparin intolerance
Contraindications of Peritoneal Dialysis
- Lack of home dialysis capability (for example severe mental or physical disability)
- Extensive peritoneal adhesions
- Large (untreated) hernia
- Severe space-occupying cystic kidneys (but to a lesser extent, APD is possible)
- Chronic inflammatory bowel disease
Advantages of Peritoneal Dialysis
- Continuous, slow ultrafiltration (UF)
- Residual kidney function preserves longer
- Freer nutrition
- Low electrolyte fluctuation
- Independent of vessels
- No anticoagulation
- Few infections (like Hepatitis B, Hepatitis C)
Disadvantages of Peritoneal Dialysis
- Glucose load-worsening of diabetic metabolic condition
- Unfavourable for lipid metabolism (lipoprotein)
- Weight gain
- Protein loss
- Patient is alone
- Prosthetic effect due to the disease
- Increased intraabdominal pressure hernia
Complications of Peritoneal Dialysis
- Catheter outlet infection
- Peritonitis
- Hernias
- Metabolic problems
- Ultrafiltration loss
- Outflow problems
- Catheter leakage
Types of Peritoneal Dialysis
There are two kinds of PD:
Manually: CAPD (Continuous Ambulatory Peritoneal Dialysis)
- Most exchanges are done typically during the day.
- Four exchanges are done in the morning after waking up, around lunchtime, late afternoon or early evening and just before bedtime.
- Each exchange takes about 20 – 30 minutes.
- Dialysis takes place during the time the PD solution is in the abdominal cavity.
- The abdominal cavity is constantly filled with dialysate and can perform on an outpatient basis.
Automatically: APD (Automated Peritoneal Dialysis)
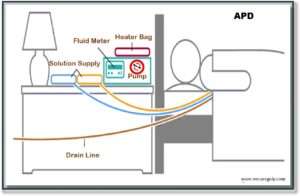
- Most exchanges are done during the night with the help of a machine, called a cycler.
- The patient is connected to the cycler which infuses the PD solution through tubing set for approximately 8–10 hours.
- The cycler fills and drains the peritoneal cavity automatically by a pump, while the patient is sleeping.
- There are different ways to perform APD depending on the lifestyle and medical condition of the patient.
APD treatment procedures:
CCPD (Continuous Cycling Peritoneal Dialysis):
- Patients with fast transport characteristics benefit particularly
- Excellent clearance values can achieve with short residence times and a high total volume
IPD (Intermittent Peritoneal Dialysis):
- The patient comes to a dialysis center three times a week.
- Here follows approx. 8-12 hours of PD using a cycler.
NIPD (Nightly Intermittent Peritoneal Dialysis):
- NIPD differs from CCPD in that the abdominal cavity is empty during the day.
- This method is only possible in patients with very good residual diuresis.
TPD (Tidal Peritoneal Dialysis):
- A variation of both IPD and CCPD is tidal dialysis.
- Here, the abdominal cavity is filled with 2.5 – 3.0 L of dialysate at night.
- The cycler is programmed to exchange only 50-70% of this volume at a time but in shorter intervals.
- However, the clearance targets, especially for medium and larger molecules, are often missed
- The incomplete exchange of the dialysate in each case brings advantages for the patients who get pain during dialysate input with the other procedures.
References
- Peritoneal dialysis – Mayo Clinic
- Peritoneal Dialysis | NIDDK (nih.gov)
- Peritoneal Dialysis – Learn about risks and benefits about this treatment – American Kidney Fund (AKF)
- PD – NephCure Kidney International ®
- What is Peritoneal Dialysis? – The National Kidney Foundation (NKF) Singapore (nkfs.org)
- Dialysis (Hemodialysis): Purpose, Procedure, and Complications (webmd.com)
- Peritoneal Dialysis at Home | Fresenius Kidney Care