What is Hemodialysis (HD)?
Hemodialysis (HD) is a type of dialysis which is an effective and the most common artificial blood purification procedure (or renal replacement therapy) used in renal failure to replace the detoxification and excretion function.

- Hemodialysis removes uremic toxins from blood primarily by the transport mechanism of diffusion.
- The ultrafiltration method helps to remove excess fluid from the blood.
- In hemodialysis, the blood on one side and the dialysis solution (dialysate) on the other are allowed to flow along a semipermeable membrane of the dialyzer. The pore size of the semipermeable membrane determines (selectively) which molecules can diffuse from the blood into the dialysis solution and vice versa.
- The membrane is permeable to water, small and medium molecules. Blood cells and larger molecules, e.g., proteins, cannot pass through the membrane. In hemodialysis, the transport rate of a substance depends, among other things, on the concentration gradient between blood and dialysis solution and the size of the molecules (unit of measurement: Dalton). The concentration gradient determines by the direction of blood flow and the dialysis fluid composition—a distinction made between counter-current and c- current.
When is Hemodialysis done?
Hemodialysis is used:
- For a few episodes in acute kidney failure or cases of poisoning
- As a permanent therapy for chronic kidney failure in the advanced stage, it means stage 5, where GFR is under 15 ml/min. The patient may have symptoms such as nausea, vomiting, swelling and fatigue, and hypertension.
What are the indications of Hemodialysis?
Absolute indications that require immediate initiation of treatment with renal replacement therapy in End-Stage Renal Disease (ESRD) are:
- Metabolic acidosis
- Hyperkalaemia
- Uremic pericarditis
- Therapy-refractory hypertension
- Hypervolemia with pulmonary oedema and peripheral oedema that can no longer treat with diuretics
- Uremic nausea and vomiting
- Progredient, uremic, central (encephalopathy) or peripheral neuropathy with confusion, myoclonus, flutter tremor, seizures
- Uremic gastroenteritis
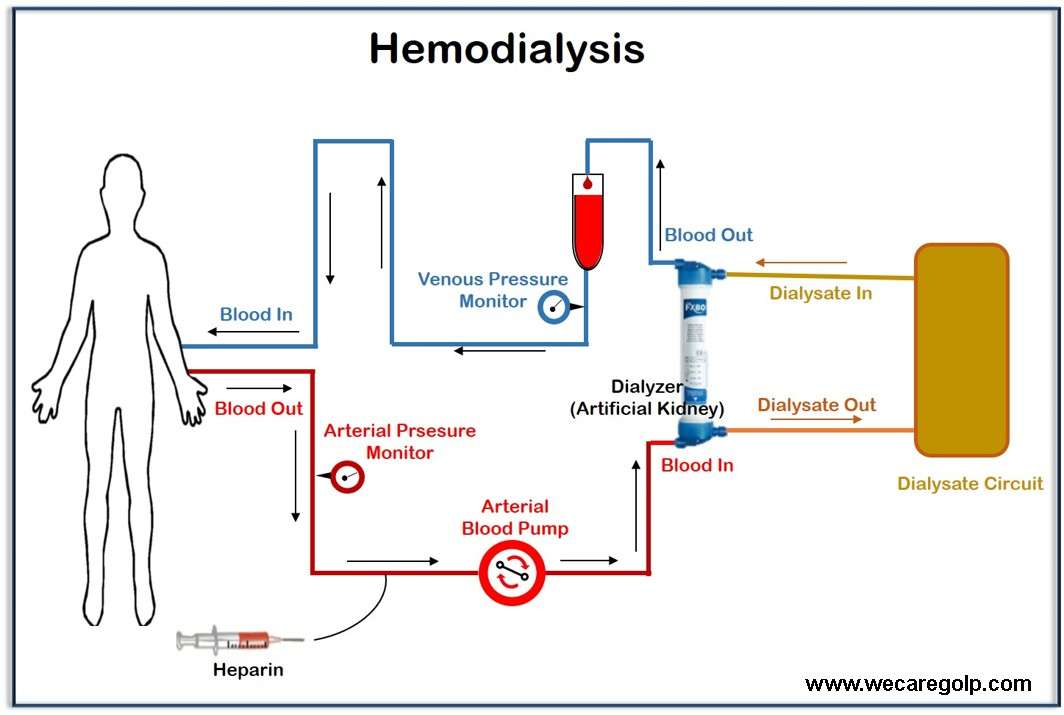
How does Hemodialysis work?
- In hemodialysis, the blood takes outside the body with the help of a blood pump through a dialysis tube into a dialysis machine. While your blood is in the machine, it goes through a filter called a dialyzer.
- The dialyzer is a hollow plastic tube that contains many tiny filters.
- There are two sections in the dialyzer: the section for the blood and dialysate. The two sections are divided by a semipermeable membrane. The semipermeable membrane allows the dialysate and blood to pass through but does not allow them to mix.
- Hemodialysis uses the principle of diffusion. If substances are present in a higher concentration on one side of the membrane than on the other side, then these migrate through the membrane until the substance concentration is equalized (diffusion).
- The blood has a different concentration of urinary substances and blood salts than the dialysate. As a result, these substances migrate from the blood into the dialysate.
- Conversely, during hemodialysis, the patient’s blood can enrich with appropriate substances (electrolytes) through a specific composition of the dialysate.
- This means that harmful substances remove from the blood and desired substances add again.
- Then, it returns to the patient’s body.
Vascular Access
To perform HD, a surgeon will create vascular access to your bloodstream.
This can be done in a few ways:
Arteriovenous (AV) Fistula
- A surgically created AV fistula is the first choice of dialysis access because of its effectiveness and safety. It is a connection between an artery (a blood vessel that carries blood from the heart) and a vein (a blood vessel that carries blood to the heart) under the skin of the arm. It is usually done in the non-dominant arm.
- An A-V fistula needs six weeks or longer to heal after surgery. Then, it can use for many years after its maturation.
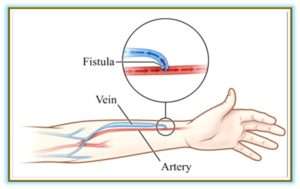
AV Fistula
Arteriovenous (AV) Graft
- It is also called arteriovenous (AV) graft.
- It is the second-best option of vascular access.
- If the blood vessels are too small to form an AV fistula, the surgeon uses a flexible, synthetic tube is used to join an artery and vein under your skin in the arm.
- This heals in only two weeks, so you can start hemodialysis faster.
- This won’t last as long as a fistula. The risk of infection and blood clots is greater with a graft.
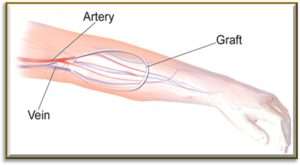
AV Graft
Central venous catheter
There are two types of a central venous catheters based on the duration of dialysis.
- Temporary (uncuffed catheter): It usually uses for a short period of time like in emergency conditions or when dialysis needs only for a few days. It is put into a vein in the neck or groin. These are more prone to infections because the barrier for bacteria to enter the bloodstream is reduced.
- Permanent (cuffed or tunneled catheter): It uses for a long-time duration. A tunneled catheter most often connects to a vein in your neck (jugular vein). It is safe to use. This method is an option if a patient needs to start hemodialysis very quickly or there is no possibility for a fistula.
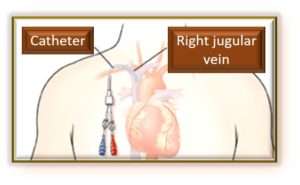
Central Venous Catheter
Where is hemodialysis done?
Hemodialysis can perform in different settings.
Dialysis center
- The kidney nurse performs all the tasks required during treatment.
- Hemodialysis is most often done at a dialysis center.
- Hemodialysis will do about three treatments a week and takes normally four hours each time.
Home Hemodialysis
- Either, you can do the treatment yourself, or you can have someone help you. A kidney nurse can train you and an assistant on how to do home dialysis. Training can take a few weeks to a few months.
- It can perform in several different ways.
- Conventional hemodialysis: three times a week for three or four hours per session
- Shorter treatments: at least 5 to 7 days per week and last about two to three hours each
- Longer, nightly treatments: 3 to 6 nights per week while you sleep
Nocturnal Hemodialysis
- Nocturnal hemodialysis can be done in a dialysis center or at home.
- It takes over 6 to 8 hours and is done at night while sleeping.
- Patients generally receive it 3 to 6 nights each week depending on how their bodies respond.
What are the Complications of Hemodialysis?
- Arterial hypotension
- Muscle cramps
- Hemolysis
- Disequilibrium syndrome
- Electrolyte imbalances
- Emboli
- Disconnections and twist of tubes
- Allergic reactions
- Infections
- Cardiac complications
How will I know if my hemodialysis is working?
- Your energy level may increase and you may have a better appetite. You should have less shortness of breath and swelling as well because hemodialysis reduces salt and fluid build-up.
- If you are careful about the sodium in your diet, your blood pressure should be controlled, you should be able to reach your ideal dry weight at the end of every HD treatment. Ideal dry weight is the weight when you don´t have extra fluid at the end of hemodialysis in your body.
- A blood test can show the effectiveness of hemodialysis. It helps measure urea reduction ratio (URR) and total urea clearance (Kt/V) to see how well your hemodialysis is removing waste from your body.
References
- What Is Hemodialysis? – DaVita
- The Advantages & Disadvantages of Hemodialysis | Laminate Medical
- Hemodialysis – Definition, procedure, and types | National Kidney Foundation
- Hämodialyse: Definition, Gründe und Ablauf – NetDoktor
- Dialysis (Hemodialysis): Purpose, Procedure, and Complications (webmd.com)