Introduction
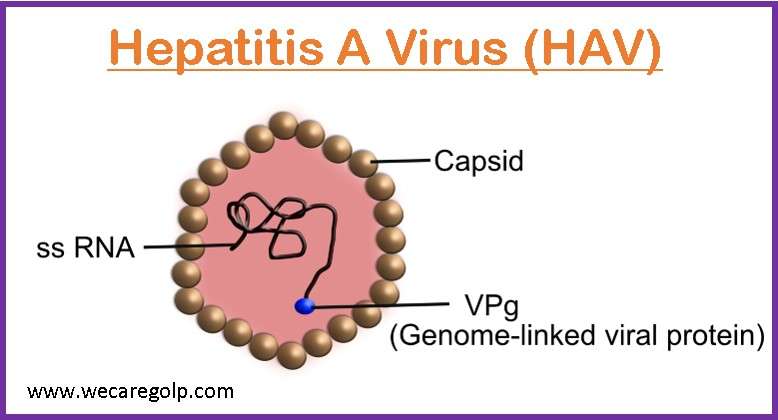
Hepatitis A is a highly contagious, short-term liver illness caused by the hepatitis A virus (HAV), a member of the Picornaviridae family of viruses with a single standard RNA and no envelope. Although it affects people everywhere, impoverished countries are where it is most common. The virus is frequently found in high amounts in the stool of persons who are genuinely ill because it replicates in the liver, is excreted in the bile, and is produced in the liver.
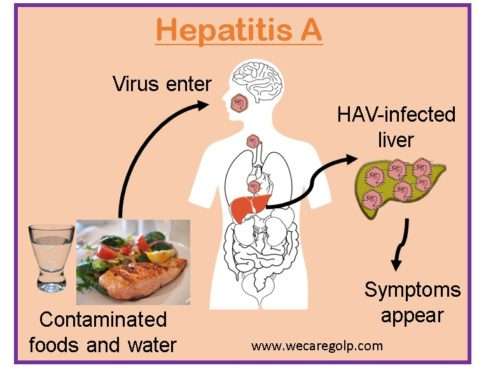
- HAV is an acute, self-limiting infection of the liver that is typically spread through the oral-fecal route.
- The two main ways that the virus is disseminated are through consuming contaminated food or drink or getting into close contact with an infected person.
- The HAV virus can cause acute, extremely contagious hepatitis, which can result in jaundice and elevated liver transaminases, along with hazy prodromal symptoms such as fever, chills, and fatigue.
- Most people have a full recovery within a few months, providing them immunity for life.
- In several nations, including the United States, it is recommended for everyone at increased risk of exposure to have the prophylactic HAV vaccine, as well as for all children older than 12 months.
Incidence
- The WHO estimates that approximately 1.4 million people worldwide contract HAV each year, with endemic rates being highest in poorer nations with low socioeconomic standards and poor sanitation and hygiene practices.
- Developed nations like the United States, Canada, and Western Europe have low infection rates.
Causes
- The Hepatitis A virus (HAV), causes hepatitis A and can be contracted by consuming minute fecal fragments from an infected person, causing disease.
Risk factors
Anyone who is not immune to hepatitis A can contract it, but some groups of people are at higher risk than others.
- People who visit high-endemicity regions without getting vaccinated.
- Members of the armed forces
- Sexually active individuals
- Individuals abusing illegal intravenous narcotics
- Employees of daycare centers
- Institutional daycare facilities
- Having sex with men
- Living with an infected individual
- Having clotting factor disorders like hemophilia
- People with HIV
- People consuming raw or undercooked seafood
- Those who are homeless
- People with chronic liver disease, including hepatitis B and hepatitis C
Mode of transmission
There are three possible routes by which the disease can be spread:
Fecal-oral route
- This is the main transmission pathway.
- It can happen directly (from person to person) or inadvertently (via tainted milk, food, or water).
- Hepatitis Epidemic breakouts have been linked to eating raw or undercooked shellfish that has been picked from sewage-contaminated water or salads.
- The virus spreads more easily in unsanitary environments.
Parenteral route
- Hepatitis A is rarely transmitted through the parenteral route (by blood and blood product or by skin penetration through contaminated needles).
Sexual transmission
- Sexual transmission may occur among homosexuals because of oral-anal contact.
Incubation Period
Hepatitis A typically requires 14 to 28 days to incubate. The duration of the incubation phase depends on how much virus is ingested.
Signs and Symptoms
Most hepatitis A-infected individuals do not exhibit any symptoms. If symptoms do appear, they are often modest and usually appear two to seven weeks after the infection.
Children under the age of six typically do not exhibit symptoms.
Hepatitis A symptoms can include
- Unusual fatigue and weakness
- Sudden nausea, vomiting, and diarrhea
- Sppetite loss
- Abdominal pain or discomfort, particularly on the upper right side beneath your lower ribs, above the liver.
- Stool that is grey or clay-colored
- Dark urine
- Jaundice, which is a yellowing of the skin or eyes
- Low-grade fever
- Severe itching
Pathophysiology
- When contaminated food is consumed, it replicates in the oropharynx and intestines before entering the bloodstream and causing viremia.
- Hepatotropic tissue tropism causes the virus to enter the liver, where it is then taken up by hepatocytes via a receptor on the plasma membrane.
- Hepatocytes and Kupffer cells (hepatic macrophages) are the sites of replication; upon viral RNA entrance, the host ribosomes bind to create polysomes.
- There is no obvious viral cytotoxicity; hepatic damage is an immunologic response to infection, accompanied by a portal and periportal lymphocyte infiltration and different degrees of necrosis; viral proteins are generated; and the viral genome is copied by a viral RNA polymerase.
Diagnosis
Hepatitis A can be diagnosed using a variety of tests.
Medical history–
- Immunization status and travel history
Physical examination
- To rule out the symptoms
Blood tests
- Elevation of the liver enzymes SGPT and SGOT to hundreds of the normal levels, which may last for 1 to 3 weeks.
- Blood result shows relative lymphocytosis.
Hepatitis A immunoglobulin M (IgM anti-HAV) antibody test
- Macroglobulin (IgM) denotes acute infection. It is the first antibody produced in response to initial antigen exposure.
- It manifests in the blood 3–4 weeks following HAV viral exposure.
- In most patients, the IgM titer remains high for approximately a month and then gradually falls to zero over about six months.
Hepatitis A immunoglobulin G (IgG anti-HAV) antibody test
- The IgG anti-HAV antibody detects IgG antibodies that appear later in the disease progression, usually shortly after the IgM antibody has disappeared.
- The IgG anti-HAV test is used to identify previous HAV infections and whether a person has acquired immunity through previous infection and immunization.
PCR test
- While early-stage antibodies cannot be found, PCR for RNA can be found in the blood and feces.
Treatment
Short-term viral infections like hepatitis A resolve on their own.Hepatitis A infection does not have a specific treatment. Treatment aims to diminish symptom intensity and reduce the risk of consequences. Options may include:
- Adequate rest
- Good nutrition and
- Plenty of fluids are recommended.
- Avoid alcohol
- Review any types of medication that can harm the liver.
- In case of fulminant liver failure- consider liver transplantation.
Complications
People who are over 50 years old are more likely to experience complications.
- Prolonged cholestasis: The gallbladder is blocked from receiving bile from the liver. It alters the blood, leading to jaundice, fever, and weight loss.
- Relapsing hepatitis- Periodically, liver inflammation symptoms like jaundice reoccur
- Autoimmune hepatitis – As a result, the liver is attacked by the body. Chronic liver disease, cirrhosis, and liver failure develop if it is not addressed.
- Liver failure
Prevention
Improved sanitation
- To inhibit the transmission of the HAV and reduce infection rates, environmental surfaces should be disinfected with a newly produced solution of household bleach diluted 1:100.
- This is because the HAV can survive on surfaces for a lengthy period of time.
- Washing hands after using the restroom, changing diapers, and before cooking or eating meals regularly.
Clean water sources
- It is recommended to boil water for at least one minute at a temperature of at least 185 degrees Fahrenheit (or 85 degrees Celsius).
- Adding chlorine or iodine to the water will also eliminate the virus.
Food safety
- Food that has been prepared in contaminated water should not be consumed.
Immunization
- The best way to avoid contracting hepatitis A is to receive immunization.
- The vaccine works by assisting the body in producing its own defenses against the disease.
- The vaccination is administered in two injections, with the second shot being administered six months after the first.
- Combinations of the hepatitis A and hepatitis B vaccines can be administered over six months.
- Immunoglobulin or the vaccine should be given to people who have recently been exposed to HAV (as post-exposure prophylaxis) as soon as feasible but no later than two weeks following the exposure.
- The hepatitis A vaccine is not recommended to anyone who has experienced hypersensitivity after receiving a dose previously.
- Hepatitis A vaccinations are often not advised for expectant mothers and nursing mothers.
The hepatitis A vaccine is recommended by the Centers for Disease Control and Prevention for the following individuals:
- All children at age of 1 year, or older children who did not receive the childhood vaccine.
- Anyone aged 1 year or older who is homeless.
- Infants ages 6 to 11 months traveling to the parts of the world where hepatitis A is prevalent.
- Family and caregivers of adoptees from countries where hepatitis A is common.
- People who are in close contact with hepatitis A infected person
- Laboratory workers who come in contact with hepatitis A
- Men having sex with men
- People traveling in parts of the world where hepatitis A is common.
- People with chronic liver disease, including hepatitis B or hepatitis C.
- People using recreational drugs.
Doses of Hepatitis A Vaccine
- The deltoid muscle is used to inject a vaccination. For kids and adults, two separate doses of 0.5 ml up to age 18 years or 1 ml for adults > 19 years.
- Typically, children receive their first dosage around 12 to 23 months old, followed by their second dose 6 to 18 months later.
- Adults receive the vaccination in a 2-dose series at 0 and 6 to 12 months (Havrix) or 0 and 6 to 18 months (Vaqta) depending on the manufacturer.
- The combined HepA and HepB vaccines can be administered to adults in three doses at 0, 1, and 6 months.
- The interval between the first and second dosages should be four weeks, and the interval between the second and third doses should be five months. As an alternative, the vaccination can be administered in four doses more quickly, on days 0, 7, 21, and 30, and then a booster shot can be given 12 months after the initial dosage.
Prognosis
- The majority of patients with hepatitis A have a great prognosis.
- The majority of hepatitis A patients recover in 3 months or less. And almost everyone recovers completely within six months.
- Some patients get brief illnesses with only minor symptoms that last a few weeks.
- Long-term immunity is common after an infection, and recurrence of symptoms is uncommon.
- Although hepatitis A rarely results in mortality, elderly people or those with underlying illnesses are at increased risk.
- The infection has no long-term negative impact on health.
- Rarely, patients with liver conditions or elderly people infected with hepatitis A can develop liver failure.
Summary
- A viral liver disease called hepatitis A can have mild to severe symptoms.
- The HAV is spread via direct contact with an infected person or by consuming tainted food and water.
- Some people may not experience any symptoms, and the symptoms can be moderate or severe.
- Consequences of infection rarely occur but can include liver failure, especially in older adults and people with underlying liver disease.
- Improved sanitation and the Hepatitis A vaccine are the most efficient approaches to controlling the virus.
- Hepatitis A infection is linked to a lack of clean water and proper sanitation.
References
- Migueres, M., Lhomme, S., Izopet, J. (2021, Sep 22). Hepatitis A: Epidemiology, High-Risk Groups, Prevention and Research on Antiviral Treatment. Viruses, 13(10):1900. https://doi.org/10.3390/v13101900
- Bhandari, P., Brett, C., Batool, A., Sapra, A.. Hepatitis A Vaccine. (Updated 2022, Sep 9). StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK554604/
- Shin, EC., & Jeong, SH. (2018, Sep). Natural History, Clinical Manifestations, and Pathogenesis of Hepatitis A. Cold Spring Harbor perspectives in medicine, 8(9), a031708. https://doi.org/10.1101/cshperspect.a031708
- Abutaleb, A., & Kottilil, S. (2020, Jun). Hepatitis A: Epidemiology, Natural History, Unusual Clinical Manifestations, and Prevention. Gastroenterology clinics of North America, 49(2), 191–199. https://doi.org/10.1016/j.gtc.2020.01.002
- Savoy, M. L. (2022, October). Hepatitis a (HepA) Vaccine. MSD Manual professional version. Retrieved 2022, Jan 13 from https://www.msdmanuals.com/professional/infectious-diseases/immunization/hepatitis-a-hepa-vaccine
- Park, K. (2017, Jan). PREVENTIVE AND SOCIAL MEDICINE (24th ed., pp. 225–227). Banarsidas Bhanot Publishers.