Introduction
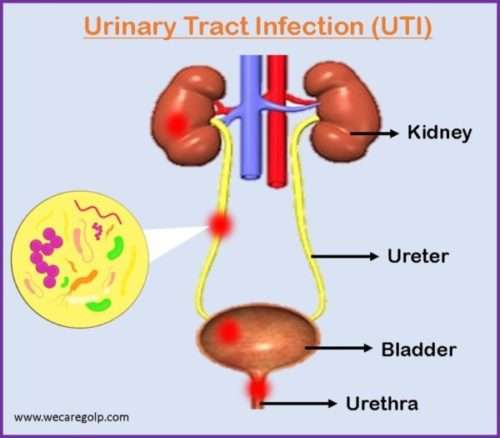
Urinary Tract Infections (UTIs) are infections that affect any part of the urinary system. UTIs are a serious public health issue caused by a variety of organisms like Escherichia coli (E. coli), Klebsiella pneumoniae, Proteus mirabilis, Enterococcus faecalis, and Staphylococcus saprophyticus.
- UTIs are one of the leading causes of morbidity and comorbidity in patients with underlying illnesses, accounting for most hospital visits worldwide.
- Knowledge of the variables related to UTIs may allow for prompt intervention, making it easy to control the condition.
- Urinary tract infection is known to produce short-term morbidity in the form of fever, dysuria, and lower abdominal pain (LAP), including irreversible kidney scarring.
- The term “urinary tract infection” refers to any microbial invasion that causes an inflammatory reaction in the urinary tract epithelium.
- It is characterized as substantial bacteriuria accompanied with cystitis or pyelonephritis caused by pathogenic inflammation of the upper or lower urinary tract.
- UTI is a bacterial invasion-induced inflammatory response of the urothelium, which is generally accompanied with bacteriuria and pyuria.
- UTI is described as bacterial colonization of typically sterile areas of the urinary system (i.e., kidneys, ureters, bladder, proximal urethra).
Classification of Urinary Tract Infection
According to the Level of Complexity
Uncomplicated UTI
- Uncomplicated UTIs have no functional or anatomical abnormalities in the urinary tract, no renal functional impairment, and no concurrent condition that would encourage the UTI.
- Patients with uncomplicated UTI have a normal, unobstructed genitourinary tract, no history of recent instrumentation, and symptoms restricted to the lower urinary tract.
- It is most frequently in young, sexually active women.
Complicated UTI
- Complicated UTIs develop in the presence of pre-existing metabolic, functional, or anatomical urinary tract problems.
- It may impact both the lower and upper gastrointestinal tracts.
- It may increase the risk of therapeutic failure and create harm that leads to recurrence.
According to the Site of Infection
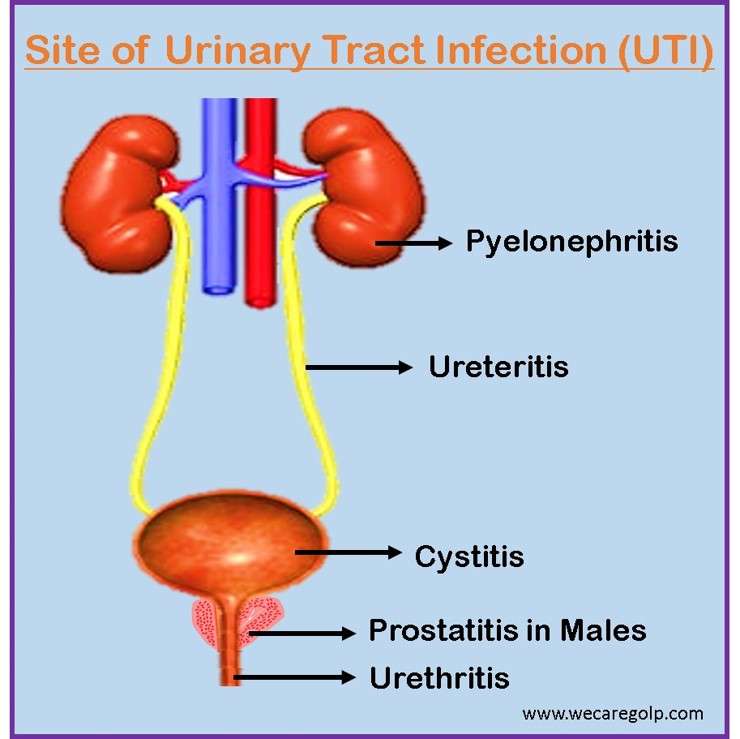
Lower Urinary Tract Infection
Lower urinary tract infection is a UTI that involves the bladder, urethra, and prostate (in a male).
Cystitis
- Cystitis (bladder infection) is the most common lower urinary tract infection.
- When bacteria from the vaginal or fecal flora colonize the periurethral mucosa and ascend to the urinary bladder, it frequently results in cystitis.
- It can be classified as either difficult or uncomplicated (simple).
- Uncomplicated cystitis is a lower urinary tract infection in otherwise healthy males or non-pregnant women.
- Complicated cystitis, on the other hand, relates to risk factors that enhance the possibility and hazard of infection or the likelihood of failing antibiotic treatment.
Urethritis
- Urethritis is an inflammation of the urethra (a fibromuscular tube that excretes urine in both males and females and semen in males), a lower urinary tract infection.
- Urethritis is closely linked to sexually transmitted diseases and can be gonococcal or nongonococcal.
- Urethral discharge is the most prevalent sign of urethritis.
Prostatitis
- Prostatitis is a term that refers to a group of infectious disorders of prostate (acute and chronic bacterial prostatitis), chronic pelvic pain syndrome, and silent inflammation.
- Prostatitis is a frequent urinary tract condition that many clinicians find difficult to treat adequately.
- After prostate cancer and benign prostatic hyperplasia, it is the third most frequent urinary tract condition in males.
- Prostatitis may account for 25% of all visits to urology clinics worldwide for complaints regarding the genital and urinary systems.
Upper Urinary Tract Infection
Upper urinary tract infection is a UTI that involves renal parenchyma and ureters.
Pyelonephritis
- Pyelonephritis is an infection of the renal pelvis and kidney caused by pathogenic bacteria ascending from the bladder to the kidneys via the ureters.
- This illness is a potentially fatal infection that can result in kidney scarring.
- During an infection, the invading pathogen may occupy a variety of hydrodynamically and immunologically difficult, linked microenvironments in the renal system.
Ureteritis
- Ureteritis is an inflammation of the ureter that is uncommon and frequently linked with cystitis or pyelonephritis.
- Additionally, a nearby inflammatory disease like appendicitis or salpingitis directly contributes to developing ureteritis.
- By lymphatic spread, the infection may also enter the ureter, notably from the prostate and seminal vesicles.
- Any concomitant ureter abnormalities, such as stricture, megaloureter, ureterocele, and so on, will predispose to infective ureteritis.
According to the Type of Infection
Acute and Chronic UTI
- While chronic infections are polymicrobial and involve more than one type of bacterium or pathogen, acute infections are associated with a single pathogen.
According to Symptoms of Infection
Asymptomatic UTI
- Asymptomatic UTIs affect 2-5% of young, healthy women and are characterized by the absence of any symptoms or signs of infection other than the presence of bacteria in the individual’s urine.
Symptomatic UTI
- A major clinical issue in older people is symptomatic urinary tract infection.
- Higher functionally impaired women and men, such as those with chronic indwelling urethral catheters, are more likely to experience it.
- Numerous symptoms, including dysuria, frequent urination, the need to pee even if the bladder is empty, fever, and flank discomfort, are displayed by individuals with symptomatic lower UTI.
Incidence
- UTIs can affect both sexes, regardless of age. Women are more prone to get UTIs than males, which is probably due to anatomical variations, hormonal impacts, and behavioral factors.
- By the age of 24, nearly one-third of women would have experienced at least one episode of UTI needing antibiotic medication.
- Almost half of all women will get at least one UTI over their lives.
- The risk of UTI is higher in infants, expectant mothers, the elderly, people with spinal cord injuries or catheters, people with diabetes, multiple sclerosis, AIDS, or HIV, and underlying urologic abnormalities.
- Catheter-associated UTI is the most frequent nosocomial infection, accounting for over one million infections in hospitals and nursing homes.
Causes of Urinary Tract Infection
- Urine is typically sterile.
- However bacterial infiltration from the periurethral region can cause illness.
- E. coli, Klebsiella pneumoniae, Staphylococcus aureus, Candida species, and Mycobacterium tuberculosis are the most prevalent pathogens.
Risk Factors of Urinary Tract Infection
- Previous UTIs, sexual activity (especially with new sexual partners), spermicide usage, menopause, pregnancy, restricted mobility (e.g., after surgery or bed rest), urine incontinence, kidney stones, and prostate enlargement.
- Age older persons are at higher risk.
- Female patients are more vulnerable than men due to shorter urethra length and closeness of the urethra to the anus, which increases the likelihood of germs entering the urinary tract.
- Suppressed immune system (diabetes), menopause, prolonged catheter use
Signs and Symptoms of UTI
- Dysuria (painful urination): most common
- Urgency (sudden onset of the need to urinate)
- Frequency (need to urinate many times)
- Hesitancy (inability to start the urine stream)
- Hematuria (blood in the urine)
According to Areas of the Urinary Tract affected
Kidneys (Acute pyelonephritis)
- High fever
- Nausea, vomiting
- Urinary urgency, frequency
- Chills with trembling
- Back pain
Bladder (Cystitis)
- Hematuria
- Burning micturition
- Pain in the pubic area, lower back, and abdomen
- Pain during sex
Urethra (Urethritis)
- Dysuria
- Discharge from urethral opening/vagina
- Urinary frequency, hesitancy
- Blood in semen or urine
- Itching
Pathophysiology of Urinary Tract Infection
- Adherence is a critical event that initiates each stage in UTI development.
- A UTI often begins with periurethral contamination by a uropathogen living in the gut, followed by urethral colonization and subsequent pathogen migration to the bladder, an event requiring appendages such as flagella and pili.
- At the point where the urethra passes through the urogenital diaphragm, there is a high-pressure zone within the urethra.
- This zone acts as a natural barrier to the ascension of organisms colonized in the distal urethra, and the bladder has inherent defenses against invading invaders.
- The interplay between host defenses and bacteria (the infectious agent) influences whether the germs survive.
- Natural bladder defense systems and regular bladder emptying control a small number of germs and some types of bacteria more efficiently than a large number of bacteria. E. coli, Coliforms, and Enterococci are typical bacterial causes of UTIs and are abundant in the perineum.
- Bacteria colonization in the periurethral allows for ascension via the urethra (Colonization phase).
- Pathogens enter the bladder, and bacteria reproduce, perhaps producing biofilms (Uroepithelium penetration).
- Pathogens can enter the urine bladder beyond the first colonization period, resulting in symptomatic or asymptomatic bacteriuria. Bacterial ascent through the ureters can occur when there is sufficient bacterial colonization.
- Bacterial ascension or the hematogenous spread can infect the renal parenchyma resulting in pyelonephritis.
- The continuous inflammatory response can result in interstitial edema, interstitial nephritis, and ultimately acute kidney injury.
Diagnosis of Urinary Tract Infection
Urinalysis
- The identification of the pathogen in the context of clinical symptoms is the gold standard for diagnosing a urinary tract infection.
- Urine culture detects and identifies the pathogen (using midstream urine). It also enables an estimation of the bacteriuria level.
- Urine dipstick analysis, rather than urinary microscopy, is a viable alternative to urine culture for diagnosing acute uncomplicated cystitis.
- Urine cultures are advised for individuals who have risk factors for complex UTIs, as well as in the following situations:
- Probable acute pyelonephritis
- Symptoms that do not improve or return after 2-4 weeks of therapy completion,
- Women presenting with unusual symptoms
- Pregnant women
- Male patients with suspected UTI.
Midstream Urine
- The gold standard diagnostic test for confirming urinary tract infection is midstream urine (MSU) culture.
- If a urinary tract infection is suspected, the conventional rule is to collect the midstream or middle section of a void.
Catheterized Urine Specimen
- To establish a closed system, indwelling urine catheters connect to a drainage bag.
- Breaking this closed system by detaching the catheter from the drainage device increases the risk of a catheter-associated urinary tract infection in the patient (CAUTI).
- Samples should not be taken from the drainage bag since the specimen might be contaminated.
- Antibiotics should ideally be taken before collecting samples, as they may impact the laboratory outcome.
- A catheter specimen must be retrieved through the catheter bag’s sampling port.
- Without the use of a needle, sampling ports are designed to be accessed directly with a Luer Lock syringe.
Suprapubic Aspiration
- Suprapubic aspiration (SPA) is a method of obtaining a urine sample.
- When a urinary catheter cannot be inserted, this procedure is frequently used.
- It is most usually performed on children, although it may also be conducted on adults.
- SPA is a sterile procedure that allows patients to sample uncontaminated urine.
Blood Test
Interpretation of Lab Results

Intravenous Pyelogram (IVP)
- A contrast dye is injected into the vein during an intravenous pyelogram (IVP), which is a series of X-rays of the kidney, ureters, and bladder.
- The pictures are utilized to detect tumors, abnormalities, kidney stones, and blockages, as well as to evaluate renal blood flow and detect Scarring, either from surgery or a urinary tract infection.
- It can also be used to screen for other illnesses or to see whether bladder cancer has spread to other parts of the urinary system.
Cystoscopy
- A cystoscopy (also known as a cystourethroscopy) is a procedure in which a cystoscope (a flexible tube and viewing equipment) is introduced via the urethra.
- Its uses are to check the bladder and urinary system for structural abnormalities or blockages such as tumors or stones and detect any problems such as hematuria, dysuria, frequent UTIs.
- Tissue sample extraction (called biopsies) can be done through the cystoscope and examined under a microscope in the laboratory.
Treatment of Urinary Tract Infection
Medical Management
- Antibiotics are the recommended medicines in all diagnosed cases of UTI.
- Treatment is to be started while awaiting the result of the urine culture.
Goals of antimicrobial therapy
- Elimination of infection
- Relief of acute symptoms
- Prevention of recurrence and long-term complications
Ideal antibiotic
- Adequate coverage
- Concentration in urine
- Duration of therapy
- Low resistance
- Cost, low adverse effects
Uncomplicated cystitis
- First line: Nitrofurantoin for 5 days
- Second line: Trimethoprim/Sulfamethoxazole (TMP/SMX) for 3 days, or oral Cephalexin for 3-7 days, or Fosfomycin for 1 day.
Complicated cystitis
- First line: Nitrofurantoin for 7 days
- Second line: TMP/SMX for 7 days, or oral Cephalexin for 7 days, or Fosfomycin every 48 hours for 3 doses.
Pyelonephritis
Ceftriaxone 1 g IM or IV × 1 dose followed by an oral antibiotic:
- First line: TMP/SMX for 7-14 days,
- Second line: Ciprofloxacin for 7 days, or Levofloxacin for 5 days;
- Third Line: Amoxicillin/Clavulanate for 10-14 days
Asymptomatic bacteriuria
- Do not treat asymptomatic bacteriuria except in pregnancy and before some urologic procedures.
Prostatitis
- The choice of antibiotics for penetrating the prostate are TMP/SMX, ciprofloxacin, or levofloxacin.
Patients with resolved symptoms do not require routine laboratory monitoring.
Patients with recurrent UTIs (two UTIs in six months or three episodes in one year):
- Provide intravaginal estrogen to postmenopausal women.
- Encourage premenopausal women in drinking at least 1.5 L of water every day.
- If behavioral techniques are ineffective, consider antibiotic prophylaxis or self-initiated treatment.
- Examine males and postmenopausal women for urinary retention.
- In individuals with recurrent UTI, cystoscopy and urinary tract imaging are seldom necessary.
Prophylaxis used for UTI
- Single dose of Trimethoprim 100mg/Nitrofurantoin 50mg
- Long-term low-dose prophylaxis beneficial
- For women – a single dose of antibiotic after sexual intercourse
Surgical Treatment
- Surgical removal of renal calculi, bladder calculi
- Ureteroplasty (Ureteral Stricture Surgery)
- Reimplantation of ureters if VUR (Vesicoureteral reflux) present
Complications of Urinary Tract Infection
Urinary tract infection complications include:
- Persistent lower urinary tract problems
- Staghorn urinary calculi
- Pyelonephritis
- Cystitis with emphysematous pyelonephritis
- Incontinence
- Focal renal nephropathy
- Renal Abscess
- Chronic prostatitis
- Abscess of the prostate
- Hypertension
Prevention of Urinary Tract Infection
- Women should urinate after sexual intercourse because germs in the bladder might multiply tenfold.
- Women should wipe from front to back after urinating, not from the anal region forward, which appears to move harmful organisms closer to the urethra. Urine flow is beneficial in the prevention
- Clean the region surrounding the anus carefully after bowel movements, wiping from front to back. Never use the same tissue repeatedly. Any wiping motion that begins at the rectum and progresses to the bladder-opening area brings possibly harmful microorganisms closer to the bladder.
- Shower instead of taking extended baths. Bath water can get polluted fast by the bather’s own skin florae. Bacteria can enter the bladder hole region while sitting in a tub.
- To minimize unwanted infection of the periurethral region with germs or bacteria, the vaginal area should be cleansed first.
- Avoiding large pauses between urinating is quite useful. Even if the desire or urge to urinate is absent, try to empty the bladder at least every 4 hours when awake during the day. When you feel the urge to empty your bladder, don’t try to “hold it” until a more convenient time or place comes around.
- Wearing tight-fitting undergarments composed of nonbreathing fabrics are not recommended. Accumulating moisture accumulates in such textiles. It causes maceration of the skin and bacterial overgrowth at the bladder entrance. Cotton underwear is recommended for everyday usage.
- Drink plenty of water. When engaged in physical activity or exercise, drink lots of water and other fluids and empty your bladder periodically.
- Low-dose antibiotic regimens used daily, three times weekly, or post coitally help avoid recurrences in most women who are prone to infection.
- Estrogen replacement treatment, particularly vaginally administered estriol creams, may also considerably lower the risk of recurrent UTI in postmenopausal women.
Prognosis of Urinary Tract Infection
Most UTI symptoms may linger for several days even after receiving antibiotic treatment. While UTIs have a low fatality rate, they have high morbidity. The quality of life in women who have recurrent UTIs might be low. Within six months, around 25% of women have such recurrences. The following factors suggest the adverse effect on UTI recovery.
- Inadequate overall health
- Advanced age
- Detection of renal calculi
- Diabetes (particularly if poorly managed)
- Sickle cell disease
- The presence of malignancy
- Urethral catheterization
- Ongoing chemotherapy
- Incontinence
- Chronic diarrhea
Summary
- Urinary tract infection (UTI) is a common bacterial illness that affects various areas of the urinary system and affects both men and women.
- Although both genders are susceptible to the illness, women are more sensitive owing to their anatomy and reproductive system.
- In most cases, bacterial invasion is the prime cause of lower and upper urinary tracts.
- E. coli is the most common pathogen for UTIs.
- Urinary infection risk factors include frequent sexual intercourse, a new sex partner, diaphragm usage, particularly with a spermicide, a lack of urine after intercourse, and a history of prior infection.
- UTIs can be classified as asymptomatic, symptomatic, complicated, uncomplicated, acute, chronic, lower UTI, and upper UTI.
- Most common clinical presentations of UTIs are urinary frequency, urgency, suprapubic discomfort, and dysuria.
- Non-pharmacological as well as good hygienic habits are the cornerstones for the reduction of recurrent UTIs.
- Urinalysis (urine culture) is gold standard test for diagnosing UTIs. Antibiotic therapy choices and duration depend on the type of UTI.
References
- Akhtar, A., Ahmad Hassali, M. A., Zainal, H., Ali, I., & Khan, A. H. (2021). A Cross-Sectional Assessment of Urinary Tract Infections Among Geriatric Patients: Prevalence, Medication Regimen Complexity, and Factors Associated With Treatment Outcomes. Frontiers in public health, 1458.
- Bennett, J. E., Dolin, R., & Blaser, M. J. (2019). Mandell, douglas, and bennett’s principles and practice of infectious diseases E-book. Elsevier Health Sciences.
- Bono, M. J., & Reygaert, W. C. (2021). Urinary tract infection. In StatPearls [Internet]. StatPearls Publishing.
- Byron, J. K. (2019). Urinary tract infection. Veterinary Clinics: Small Animal Practice, 49(2), 211-221.
- Chu, C. M., & Lowder, J. L. (2018). Diagnosis and treatment of urinary tract infections across age groups. American journal of obstetrics and gynecology, 219(1), 40-51.
- Cyran, O., Jagodzińska, M., & Nowicki, M. (2019). Knowledge and usage of prevention measures against urinary tract infections among young women. Family Medicine & Primary Care Review, 21(4).
- Flores-Mireles, A. L., Walker, J. N., Caparon, M., & Hultgren, S. J. (2015). Urinary tract infections: epidemiology, mechanisms of infection and treatment options. Nature reviews microbiology, 13(5), 269-284.
- Grigoryan, L., Trautner, B. W., & Gupta, K. (2014). Diagnosis and management of urinary tract infections in the outpatient setting: a review. Jama, 312(16), 1677-1684.
- Kaur, R., & Kaur, R. (2021). Symptoms, risk factors, diagnosis and treatment of urinary tract infections. Postgraduate medical journal, 97(1154), 803-812.
- Sabih, A., & Leslie, S. W. (2022). Complicated urinary tract infections. In StatPearls [internet]. StatPearls Publishing.
- Simerville, J. A., Maxted, W. C., & Pahira, J. J. (2005). Urinalysis: a comprehensive review. American family physician, 71(6), 1153-1162.
- Tan, C. W., & Chlebicki, M. P. (2016). Urinary tract infections in adults. Singapore medical journal, 57(9), 485.
- Vasudevan, R. (2014). Urinary tract infection: an overview of the infection and the associated risk factors. J Microbiol Exp, 1(2), 00008.