Introduction
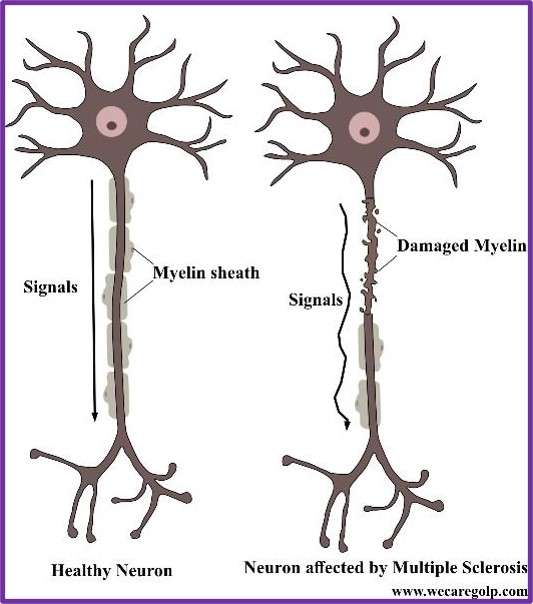
Multiple sclerosis (MS) is a chronic autoimmune, inflammatory demyelinating and neurodegenerative disease of the central nervous system (CNS).
- The disease occurs when the immune system attacks nerve fibers and myelin sheath in the brain and spinal cord causing inflammation, which destroys nerve cell processes and myelin altering electrical messages in the brain.
- The main feature of MS is symptomatic episodes that occur months or years apart and affect different anatomic locations.
- The damage results in different problems including physical, mental, and occasionally psychiatric.
- It is a lifelong condition which may cause serious disability but can be mild occasionally.
Incidence
According to the 3rd edition of the Multiple Sclerosis International Federation (MSIF) Atlas of (MS), the number of people with MS across the globe has increased from 2.3 million in 2013 to 2.8 million in 2020 showing an increase in number (1.5% of cases) of children and young people under 18 living with MS with a high proportion of females.
Classification of Multiple Sclerosis
Classification is based on clinical criteria, frequency of clinical relapses, time to disease progression, and lesion development on MRI.
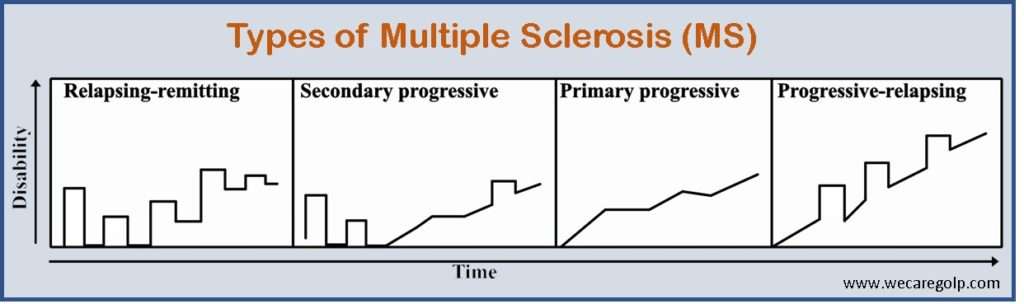
- Relapsing-remitting MS (RRMS): Around 85% of people with MS are initially diagnosed with RRMS, marked by flare-ups (relapses or exacerbations) of new or increasing symptoms followed by periods of remission when symptoms improve or disappear.
- Clinically isolated syndrome (CIS): It is a first single episode with symptoms lasting at least 24 hours and caused by inflammation or demyelination in the central nervous system (CNS). If another episode occurs, diagnosed as relapse-remitting MS.
- Secondary-progressive MS (SPMS): Relapsing-remitting MS (RRMS) patients usually progress into a secondary progressive phase, in which clinical deterioration remains with or without any periods of remission or leveling off symptom severity.
- Primary-progressive MS (PPMS): Symptoms continue to worsen progressively, without early relapses or remissions, but some patients may experience occasional stability (plateaus). Approximately 10% of MS patients are affected with PPMS, which is more resistant to the drugs typically used to treat the disease.
- Progressive-relapsing MS (PRMS): PRMS is a rare form of MS affecting fewer than 5% of patients. It is progressive from the start and continues to cause progressive intermittent flare-ups of worsening symptoms.
Causes of Multiple Sclerosis
The main cause of MS is unknown. It is considered an autoimmune disease that occurs as a result of some combination of genetic and environmental factors such as:
Infectious agents
- Human herpesviruses
- Epstein-Barr virus (EBV)
- Cytomegalovirus
Genetics
- MS is not a hereditary disease, but a number of genetic variations relate to increase the risk.
- Some specific genes that have been linked with MS include differences in the human leukocyte antigen (HLA) system—a group of genes on chromosome 6 that serves as the major histocompatibility complex (MHC).
- The probability of developing the disease is higher in close relatives, identical twins, and siblings of an affected person.
- If both parents are affected the risk in their children is 10 times higher than that of the general population.
Other risk factors
- Certain autoimmune disorders: thyroid disease, pernicious anemia, psoriasis, type 1 diabetes, inflammatory bowel disease, rheumatoid arthritis, etc.
- Race. White people, particularly those of Northern European descent, are at the highest risk of developing MS while Asian, African, or Native American descents have the lowest risk.
- Climate. MS is more common in countries with temperate climates. Areas farthest from the equator have the highest prevalence of MS. On the contrary, MS is rare in populations living near the equator.
- Smoking and alcohol consumption
- Stress, occupational exposures, and toxins
- Obesity during adolescence and young adulthood
- Dietary deficiency of Vitamin D and B12
Signs and Symptoms of Multiple Sclerosis
The symptoms of MS often vary among patients. The symptomatic episodes have variations in time and space that occurs months or years apart and affect different anatomic locations.
The main symptoms include:
- Sensory loss (paresthesia) is usually an early complaint
- Spinal cord symptoms
- motor – Muscle cramping secondary to spasticity
- autonomic – Bladder, bowel, and sexual dysfunction
- Cerebellar symptoms – Charcot triad of dysarthria, nystagmus, and intention tremor
- Optic neuritis
- Bilateral facial weakness or trigeminal neuralgia
- Irregular twitching of the facial muscles which may also be a presenting symptom
- Eye symptoms including diplopia on lateral gaze
- Heat intolerance
- Constitutional symptoms; especially fatigue and dizziness
- Pain
- Subjective cognitive difficulties related to attention span, concentration, memory, and judgment
- Depression
- Euphoria
- Bipolar disorder or frank dementia
- Symptoms associated with partial acute transverse myelitis
- Aphasia or dysphasia may occur very rarely
- Seizures
- Other paroxysmal symptoms like ataxia, akinesia, paresthesia, pruritus
- Significant motor complaints without sensory deficits
Pathophysiology of Multiple Sclerosis
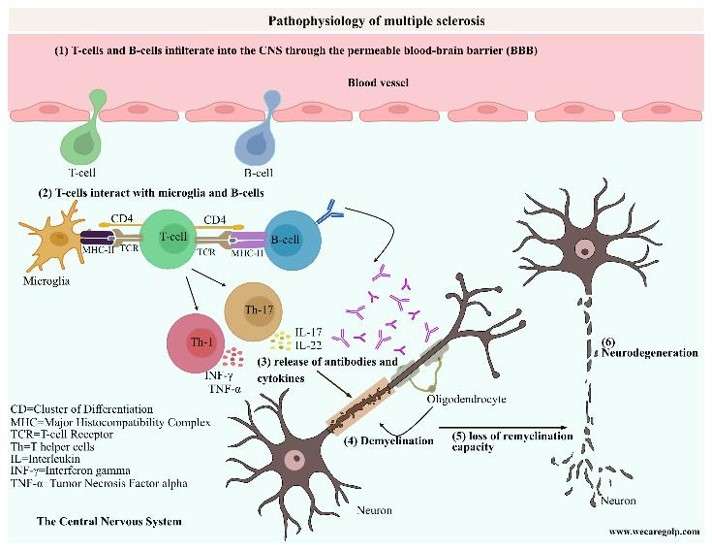
- The immune system triggers T and B cell response to myelin self-antigens and begins the early inflammatory demyelination process.
- Autoimmune response triggers peripheral activation of CD4 + T-cells and CD8 + T-cells, which cross the blood-brain barrier (BBB).
- CD4 + T-cells attach to myelin antigens, presented by antigen-presenting cells in the brain parenchyma.
- CD4 + T-cells activate in the production of cytokines which play a minor role in the inflammatory destruction of myelin by causing persistent activation of microglia and macrophages.
- It causes the activation of IL-17 from T-helper cells. IL-17 is a more potent pro-inflammatory cytokine and is highly expressed, particularly during relapse.
- The inflammatory complement cascade is activated, which releases additional cytokines and chemokines and recruit monocyte and B cells.
- B-cells produce autoantibodies, which further activate T-cells.
- CD8 + T-cells drive direct axonal injury to MHC /antigen-expressing cells such as neurons and oligodendrocytes.
- Loss of myelin causes a loss of nerve conductivity and leads to a loss of brain volume and disruption of sodium, calcium, and potassium ion channels that interfere with neuronal conductivity.
- Demyelination and axonal loss lead to the development of MS lesions or plaques, particularly in the white matter, but they can also occur in the gray matter.
- More diffuse “shadow lesions” occur throughout the CNS causing abnormal Wallerian degeneration.
Diagnosis of Multiple Sclerosis
- Magnetic resonance imaging (MRI) is the best choice for confirming MS and monitoring disease progression in the CNS is
- An evoked potentials or evoked response is used to identify subclinical lesions
- Lumbar puncture is done to evaluate cerebrospinal fluid (CSF) for oligoclonal bands and intrathecal immunoglobulin G (IgG) production
- OCT (Optical coherence tomography) is used to detect changes in the retina related to brain atrophy
- Blood tests to rule out diseases that cause similar symptoms, such as HIV and Lyme disease.
Treatment and Management of Multiple Sclerosis
Treatment is classified into 3 groups; Abortive, preventive and symptomatic therapy.
Abortive Therapies
- Steroids (glucocorticoids) are prescribed to shorten the duration and severity of the attack in acute exacerbation.
- Intravenous methylprednisolone is given once a day for three-to-five days. Sometimes the intravenous steroid is followed with an oral dose in a tapering dose for an additional 1-2 weeks.
Preventive Therapies
Preventive treatments are given to reduce the frequency and severity of MS exacerbations or to treat the worsening condition. These treatments include:
- Interferon betas (INF- β) inhibit certain immune system cells and processes so that the inflammatory process known to occur in MS is decreased.
- Interferon beta-1a is given once a week by intramuscular (IM) injection or 3 times a week by intradermal (ID) route.
- Interferon beta-1b is another form of beta-interferon which may be given on an alternate day by ID injection. The frequency depends on the specific therapy.
- Glatiramer acetate is given daily by ID injection. It is a synthetic protein structurally similar to a component of myelin which helps immune system produce more anti-inflammation immune cells. This will then help to reduce the inflammation in MS.
- Natalizumab is a monoclonal antibody given intravenous (IV) once every 4 weeks. It works by blocking the ability of immune cells (lymphocytes) entering the central nervous system.
- Mitoxantrone is a chemotherapy drug indicated for worsening forms of relapsing MS and secondary progressive MS. It is given by IV infusion every 3 months. The drug can be very toxic so it can only be given in a limited number of doses over the course of someone’s life. The drug works by suppressing the immune system and reducing the overall numbers of immune cells that could be the cause of inflammation in MS.
Symptomatic Therapies
The inflammation and damage from MS can interrupt normal nerve transmission in CNS, which results in many transient and permanent symptoms. The major goal is to maintain independent function and improve quality of life.
- Physical and occupational therapies are particularly beneficial in maintaining and improving normal function.
- Consultation with urologists, psychiatrists, and pain management specialists may be helpful.
- Physical and occupational therapists and orthotics specialist help in improving mobility.
A coordinated, comprehensive, interdisciplinary approach is necessary for the long-term management of multiple sclerosis.
Prevention of exacerbation
Along with Disease-modifying therapies, lifestyle changes also help to improve relapses and further attacks. These include:
- Healthy diet: Balanced diet that includes lots of fruit and vegetables, whole grains, healthy fats, and lean protein and limiting the intake of added sugars, unhealthy fats, and processed foods.
- No smoking and alcohol: Smoking and alcohol are linked to worsening MS symptoms and could speed the disease’s progression. Quitting smoking will improve the health condition of people with MS.
- Regular exercise: Multiple sclerosis can cause muscle weakness, loss of balance, and difficulty walking. To keep muscles healthy and sustain physical function, it is important to engage in aerobic exercise, flexibility, and strength training.
- Managing stress: Stress can take a physical and emotional exertion interfering with sleep, which may worsen MS-related fatigue. Yoga, meditation, exercise, etc. may help to manage stress.
Complications
- With the loss of function and mobility, patients become more susceptible to several complications, such as problems with coordination, muscle spasms, involuntary movements, muscle paralysis, and rigidity.
- These can make them more prone to infections, pressure ulcers, osteoporosis, aspiration pneumonia, urinary tract infections, depression, and accidents.
Prognosis
- MS is a challenging disease but rarely fatal. Some severe complications such as bladder infections, chest infections, and difficulty swallowing could lead to death.
- MS does not always result in severe paralysis. Although two-thirds of people with MS can walk, many of them will need aids like a cane, wheelchair, crutches, or a scooter.
- A person with MS has a 5-10 years lower average life expectancy than the average person.
Summary
Multiple sclerosis is a chronic condition involving the central nervous system (CNS) in which the immune system attacks myelin; the protective layer around nerve fibers. MS is usually diagnosed between the ages of 20 and 40 and affects more women than men. Symptoms of the disease vary depending on the affected area. The course of the disease varies from person to person.
References
- The Multiple Sclerosis International Federation, Atlas of MS, 3rd Edition (September 2020).
- Browne, P., Chandraratna, D., Angood, C., Tremlett, H., Baker, C., Taylor, B. V., & Thompson, A. J. (2014). Atlas of multiple sclerosis 2013: a growing global problem with widespread inequity. Neurology, 83(11), 1022-1024.
- Sandi, D.; Kokas, Z.; Biernacki, T.; Bencsik, K.; Klivényi, P.; Vécsei, L. Proteomics in Multiple Sclerosis: The Perspective of the Clinician. Int. J. Mol. Sci. 2022, 23, 5162. https://doi.org/10.3390/ ijms23095162
- https://www.nhs.uk/conditions/multiple-sclerosis
- https://www.health.harvard.edu/diseases-and-conditions/multiple-sclerosis
- https://emedicine.medscape.com
- https://www.nationalmssociety.org
- https://www.rarediseaseadvisor.com