Introduction
Colposcopy is a procedure to visualize and assess the uterine cervix, specifically the transformation zone (TZ), for the detection of cervical intraepithelial neoplasia (CIN) and invasive cancer using a specific instrument called a colposcope.
- Colposcopy works on the principle of magnification and illumination, usually in the form of a lens system and a digital imaging system.
- A colposcopist is a doctor who has been specially trained to develop the technique to perform a colposcopy.
- Computer technology helps to capture images directly into a computer, and these images allow enhancement and manipulation according to the physician’s preference.
- About 3% to 5% acetic acid and lugol iodine solution are used to identify potential lesions.
- Because of the subjective nature of visual changes, all the potential lesions are recommended for biopsy along with colposcopy.
Epidemiology
- Nearly 3 million of the approximately 50 million American women who undergo cervical cancer screening each year receive referrals for colposcopy to obtain a positive result.
Elements making up a Colposcope

The head of the colposcope is the essential part and is made up of
Lens
- Optic tubes contain binocular lenses.
- It allows the adjustment of dioptries to correct refraction errors individually.
Focus
- Colposcope is focused by displacing the head of colposcope.
- The focus may be macrometric focus or micrometric focus.
Filters
- Green or blue filters are available.
- It impedes the transmission of red light, highlighting the view of vessels locating the stroma and facilitating evaluation of their characteristics.
Magnification
- The use of low magnification is to evaluate external genitalia.
- The use of medium magnification is to assess the vulva, vagina, and cervix.
- The use of high magnification is to examine the fine specific details like glandular orifices, vascular patterns
Light Source
- It provides good illumination for observation
Adjustable Arm and Stand
- Colposcope can be fixed on an examination table
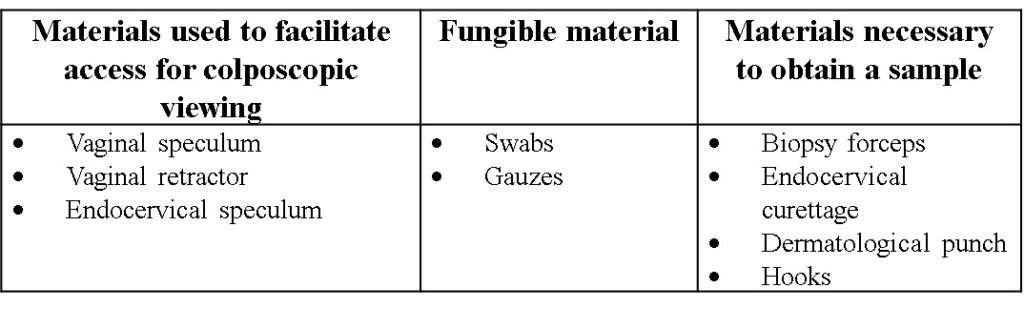
Instruments for Colposcopy

A colposcopist uses a collection of materials and instruments to evaluate the lower genital tract. The following materials can use to perform colposcopy.
Chemicals used in colposcopy
Acetic acid
- 3%-5% acetic acid is used.
- Concentration of 5% produces a more rapid and durable histological response than 3%.
- Exact mechanism of whitening of the lesion area by acetic acid is unknown.
- However, studies show that acetic acid temporarily dehydrates the cells reducing the nucleus/cytoplasm relationship.
- It may also cause precipitation or reversible coagulation of cellular proteins like cytokeratin and nuclear proteins.
- Method of use:
- Use dampened swab or with direct instillation or pulverization of the cervix.
- Acetic acid should act for at least 20 seconds before withdrawal to see acetoreactivity.
Lugol solution

- Composed of potassium iodide 10g, distilled water 100 ml, and iodine crystals 5 gm.
- Mechanism of action of lugol iodine is shown in the figure below.

Indications
Although Human Papilloma Virus (HPV) infection is the cause of virtually every case of cervical cancer and precancer, HPV infection is quite usual and usually transient, especially among young women. Thus, colposcopic evaluation and guided biopsy remain critical tools in distinguishing whether the woman requires the destruction of the cervical transformation zone where persistent HPV infections can lead to cancer.
The main indication for colposcopic examination is the evaluation of women at the increased risk for cervical neoplasia, including those with:
- Abnormal or inconclusive cervical screening tests
- Signs and symptoms of possible cervical cancer like any suspicious cervical abnormality found during a pelvic examination, abnormal genital bleeding, or unexplained cervicovaginal discharge.
- Primary screening for cervical cancer
- Past cytologic and/or pathologic anogenital tract abnormalities
- Abnormal pap smear test or when the cervix looks abnormal during the collection of a pap smear
- Clinically suspicious cervix
- Genital warts
- Precancerous changes in the tissue of the cervix, vagina, and vulva
- Evaluation of sexually assault victims
- Follow up of a patient with intraepithelial lesion before or after treatment.
Benefits of Colposcopy
- Colposcopy can detect pre-malignant lesions of the lower genital tract.
- Colposcopy can determine the suitable biopsy site.
- It helps to facilitate and individualize treatments
- Colposcopy allows the follow-up of intraepithelial lesions
- Accurate identification
- Feasible
- More sensitive
- Acceptable.
Potential Risks of Colposcopy
- Severe bleeding
- Pelvic pain
- Infection
- Unpleasant vaginal odor
- Lower abdominal pain
- Anxiety
- Inadequate use of colposcopy
- Colposcopy performed by inexperienced professionals
- Anaphylactic reaction to lugol’s solution
Procedure
Patient Preparation before Colposcopy
- Provide patient teaching on the procedure of colposcopy.
- Ask the patient to void before the procedure.
- Take informed consent
- Review the health history of the patient including:
- Smoking habit
- Date of last period (rule out pregnancy)
- HIV
- Any types of immunosuppression
- Parity
- Current hormonal situation: fertile age/pregnancy/menopause
- Current contraception
- History of hysterectomy or previous treatments for intraepithelial lesions
- History of squamous intraepithelial lesions (cervical, vaginal, vulvar, or anal)
- Date and result of all the previous screening tests and biopsies available
- Vaccination against HPV (including vaccination date and type of vaccine)
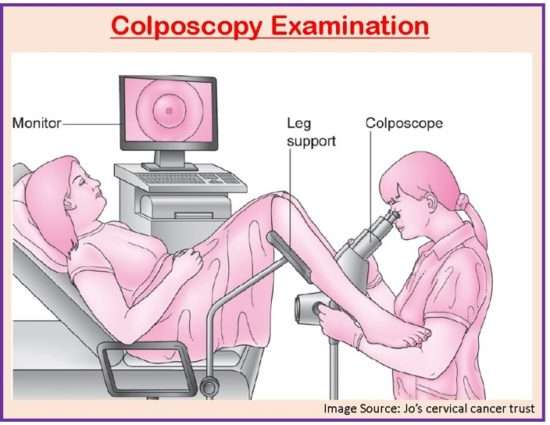
Colposcopy Procedure
- Check the functioning of the instruments.
- Place the patient in the dorsal lithotomy position.
- Turn on the colposcope and focus the lens on the personal characteristics of examiner.
- Visualize the vulva and perianal area
- Insert vaginal speculum of adequate size and length inside the vagina.
- Clean any secretions using a saline solution for adequate visualization.
- Visualize the cervical anatomy, mucosal tropism, and presence or absence of signs of infection.
- Examine the vascular pattern
- Obtain the sample if indicated.
- Apply acetic acid 3.5% to the cervix.
- With white light and low and high magnification, carefully visualize the changes needed.
- Determine if colposcopy is adequate or not.
- Identify the squamocolumnar junction and categorize the transformation zone.
- Identify and evaluate characteristics of colposcopic findings at the level of cervix, endocervix, and vaginal pouch fundus.
- Make digitalized images when possible.
- Apply lugol solution to specify the topography and extension of a suspicious zone.
- Make targeted biopsies in indicated cases and coagulate bleeding zones of the area of biopsies.
- Carefully withdraw the speculum.
- Revise samples to ensure correct identification before sending them for analysis.
- Gage et. al. (2006) recommends that it is worth comparing at least three options: additional biopsy specimen from another part of the worst-looking lesion, additional biopsy specimen from another abnormal area or areas, and random biopsy specimens of quadrants that have no evident abnormalities.
Patient Care after Colposcopy
- Provide patient teaching on not to apply anything inside the vagina for 1 week.
- Do not douche or apply vaginal medication for a week.
- Do not have sexual intercourse for a week.
- Notify the health care provider if a complication arises.
Criteria for Report Findings
- Cervix visibility (Fully visualized/not visualized)
- Squamocolumnar junction visibility
- Acetowhitening(yes/no)
- Lesions present (yes/no)
- Location of the lesion
- Size of the lesion
- Vascular changes
- Other features of lesions (contour/borders/lugol’s uptake, etc.)
Core/Minimum criteria for reporting findings at colposcopic examination
It includes:
- Squamocolumnar junction visibility (fully visualized/not fully visualized)
- Acetowhitening (yes/no)
- Lesions present (acetowhite or other) (yes/no)
- Colposcopic impression (normal/benign; low grade/high grade cancer)
Interpretations of Colposcopic Findings
Colposcopic classification of the International Federation of Cervical Pathology and Colposcopy (IFCPC) 2011
General Evaluation
- Adequate/inadequate for the reason e.g., cervix not clear due to inflammation, bleeding, scarring.
- Visibility of the squamocolumnar junction completely, partially, or not visible.
- Types of transformation zone 1,2,3
Normal Colposcopic Findings
- Original squamous epithelium
- Mature
- Atrophic
- Columnar epithelium
- Ectopy
- Metaplastic squamous epithelium
- Naboth cysts
- Glandular openings and/or glandular crypts
- Deciduous in pregnancy
Abnormal Colposcopic Findings
- General principles
- Location of the lesion: Inside or outside the transformation zone, clockwise location of the lesion
- Lesion size: Number of quadrants of the cervix covering the lesion, size of the lesion as a percentage of cervix
- Grade 1 (Minor)
- Fine mosaic
- Fine punctation
- Thin acetowhite epithelium
- Irregular, geographic border
- Grade 2 (Major)
- Sharp border
- Inner border sign
- Ridge sign
- Dense acetowhite epithelium
- Coarse mosaic
- Coarse punctuation
- Rapid appearance of acetowhitening
- Cuffed crypt (gland) openings
- Nonspecific
- Leukoplakia (keratosis, hyperkeratosis), erosion
- Lugol solution (Schiller test): positive/negative
Suspicion of Invasion
- Atypical vessels
- Additional signs: thin vessels, irregular surface, exophytic lesion, necrosis, ulceration(necrotic), nodular tumoration
Miscellaneous Findings
- Congenital transformation zone, condyloma, polyp (ectocervical/endocervical), inflammation, Stenosis, Congenital abnormality, Posttreatment abnormality, Endometriosis
Contraindications
- No absolute contraindications exist. However, special precautions may be required in circumstances like pregnancy with placenta previa.
- Acute cervicitis and vulvovaginitis should be treated before the examination as inflamed tissues can alter the accurate assessment.
Summary
- Colposcopy is the process of visualizing the vagina with the help of a colposcope.
- Colposcopy works on the principle of magnification and illumination.
- About 3% to 5% acetic acid and lugol iodine solution is used to identify potential lesions.
- Colposcopy is indicated in abnormal or inconclusive cervical screening tests, primary screening for cervical cancer, genital warts, evaluation of sexually assault victims, and follow-up of the patient with intraepithelial lesion before or after treatment.
- Colposcopy can treat pre-malignant lesions of the lower genital tract and facilitates individualized treatment.
- However, the risks of severe bleeding and infection may occur after colposcopy.
- Proper patient care should be done before, during, and after colposcopy.
- Colposcopy findings should be evaluated as per the protocol.
References
- Gage, J. C., Hanson, W., Abbey, K., Dippery, S., Gardner ,S., Kubota, J., Schiffman, M., Solomon, D., Jeronimo, J.ASCUS LSIL Triage Study (ALTS) Group . (2006, Aug). Number of cervical biopsies and sensitivity of colposcopy. Obstetrics & Gynecology,108(2):264-72. DOI: 10.1097/01.AOG.0000220505.18525.85
- Bornstein, J., Bentley, J., Bösze, P., Girardi, F., Haefner, H., Menton, M., Perrotta, M., Prendiville, W., Russell, P., Sideri, M., Strander, B., Tatti, S., Torne, A., Walker, P. (2012, July). 2011 Colposcopic Terminology of the International Federation for Cervical Pathology and Colposcopy. Obstetrics & Gynecology, 120:166–72. DOI: 10.1097/AOG.0b013e318254f90c
- Khan, M. J., Werner, C. L., Darragh, T. M., Guido, R. S., Mathews, C., Moscicki, A., Mitchell, M. M., Schiffman, M., Wentzensen, N., Massad, L. S., Mayeaux, E.J., Waxman, A., Conageski, C., Einstein, M., Huh, W. K. (2017, Oct). ASCCP Colposcopy Standards: Role of colposcopy, Benefits, Potential Harms, and Terminology for Colposcopic Practice. Journal of Lower Genital Tract Disease, 21 (4): p-223-229. DOI: 10.1097/LGT.0000000000000338
- Dexus, S., Cararach, M., Dexeus, D. (2002). The role of colposcopy in modern gynaecology. Eur. J. Gynaecol.Oncol, 23(4), 269-277
- AEPCC guidelines. Colposcopy guidelines standards of quality
- https://journals.lww.com/jlgtd/Fulltext/2017/10000/ASCCP_Colposcopy_Standards__Risk_Based_Colposcopy.4.aspx
- https://www.nhs.uk.com
- https://www.hopkinsmedicine.org
- https://www.acog.org
- https://www.cancerresearchuk.org