Introduction
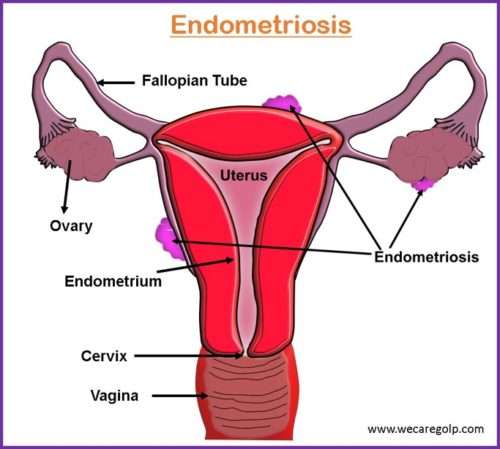
Endometriosis is derived from the Greek words, ‘endo’ meaning inside, ‘metra’ meaning uterus, and ‘osis’ meaning disease. Endometriosis is a chronic estrogen-dependent gynecological disease characterized by the ectopic implantation of the endometrial tissue outside the uterus.
- The localization of endometriotic lesions may vary with the most common site being the ovaries followed by the fallopian tubes and tissues lining the pelvis.
- Rarely, it can also be found in the areas where pelvic organs are located.
- In endometriosis, the extra uterine-like tissue undergoes changes in a menstrual cycle like a normal endometrial tissue in the uterus.
- The extra uterine-like tissue thickens, break down, and bleeds with each menstrual cycle.
- As this tissue has no way to exit the body, it gets trapped.
- Thus, the surrounding tissue can become irritated, eventually developing scar tissue and adhesions.
- The bands of fibrous tissue can cause pelvic tissues and organs to stick to each other leading to various complications.
Epidemiology
- Endometriosis is estimated to affect approximately 10% to 15% of women of reproductive age, whereas this prevalence increases by up to 70% in women with chronic pelvic pain.
- According to the survey of the National Hospital Discharge Survey, in the U.S., 11.2% of all women between 18 and 45 years old hospitalized for genitourinary causes were diagnosed with endometriosis, and approximately 10.3% of the women have undergone gynecologic surgeries due to endometriosis.
- In women with infertility, endometriosis is up to 50%, whereas, in adolescents, the incidence of endometriosis is reported to be 47% of those who have experienced laparoscopy for pelvic pain.
Types of Endometriosis
The three most typical types of endometriosis are:
Superficial peritoneal lesions
- It can occur in the form of intraperitoneal and peritoneal lesions.
- The foci of endometriosis are within the peritoneum.
- It is found in 15-50% of all women diagnosed with endometriosis.
Ovarian endometrioma
- It is also known as pseudocysts.
- They are different from the ovarian cyst by the fact that the endometriotic tissue bleeds inside of the endometriotic cyst.
- It occurs in 2-10% of women of reproductive age and 50% of patients treated with infertility.
Deep Infiltrating Endometrioma (DIE)
- They are the endometriotic lesions that infiltrate the peritoneum more than 5 mm.
- It can involve additionally the bladder, ureter, bowel, more frequently rectovaginal septum, and less commonly sigmoid.
- Neural damage may also occur due to the invasion of endometrial stromal cells and mediators like mast cells, activated macrophages, and leukocytes.
Stages of Endometriosis
- The most widely used and best-known system was developed by the revised American Society for Reproductive Medicine (rASRM).
- The rASRM classification system is divided into 4 stages/grades according to the number of lesions and depth of infiltration: minimal (stage I), mild (stage II), moderate (stage III), and severe (stage IV).
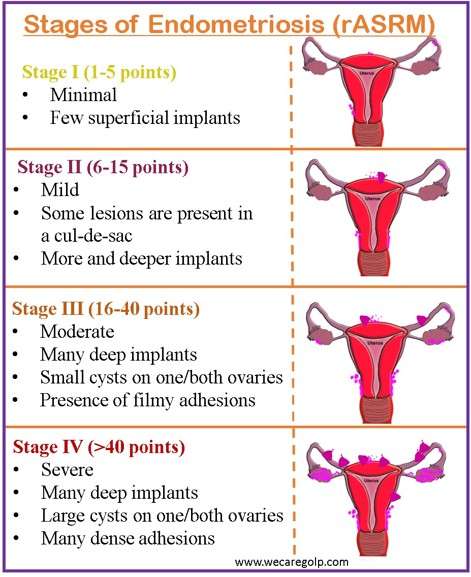
Benefits of rASRM Classification
- Most widely used classification
- Easy to use
- Simple for the patient to understand
Limitations of rASRM Classification
- Arbitrary scoring system
- Wide score ranges between categories
- Can be affected by surgical technique and timing of surgery
- Does not provide a good characterization of the disease
- Does not provide a good characterization of disease severity and pregnancy outcomes.
Causes of Endometriosis
Although the exact cause of endometriosis is unclear, the main theories utilized to explain the pathogenesis of endometriosis are Sampson’s theory, the coelomic metaplastic theory, the stem cell theory, the Müllerian remnant theory, and the vascular and lymphatic theory. The reason why a single theory cannot explain the pathogenesis of endometriosis could be due to the intricate relationship between the expression of endometriosis-related genes, inflammatory responses, and altered hormonal responses to these stimuli.
Sampson’s theory
- The phenomenon of retrograde menstruation in women with endometriosis has been demonstrated in 90% of all women undergoing laparoscopy during menstruation.
- It states that the viable cells existing in the peritoneal fluid with retrograde menstruation can implant, grow, and infiltrate the peritoneal cavity.
- In retrograde menstruation, the menstrual blood containing endometrial cells flows backward from the fallopian tubes to the pelvic cavity during menstruation instead of out of the body.
- The endometrial fragments reach the pelvis via transtubal retrograde blood flow.
- Extrauterine endometrium proliferates and causes chronic inflammation with the formation of adhesions.
- Phenotypic expression of endometriosis (depending on genetics and environmental factors) occurs.
Coelomic metaplastic theory
- This theory states the ability of parietal peritoneum epithelium to differentiate into endometrial tissue under the stimuli of cytokines and growth factors of the endometrial stroma.
- The coelomic metaplastic theory is justified by the occurrence of endometriosis in women without a uterus or a lack of endometria, such as female patients with Mayer-Rokitansky-Küster-Hauser syndrome or the rare cases of males suffering from endometriosis.
Müllerian remnant theory
- This theory explains the occurrence of endometriosis in the cul-de-sac and uterosacral ligaments.
- It suggests that atypical migration or differentiation of the remnants could imitate endometriotic tissue in the poster pelvic floor.
Lymphatic and vascular metastasis theory
- In this theory, endometrial tissue may be able to infiltrate the lymphatics and vasculature, transferring to distant locations like the brain, pleura, or retroperitoneal areas.
Stem cell theory
- The development and progression of endometriosis may be attributed to the endometrial stem cells.
- Endometrial progenitor cells have been recognized in menstrual blood and also in clonogenic cells in endometrial lesions.
- Endometrial stem cells may be retrogradely discarded in the pelvic cavity during either newborn uterine hemorrhage or menstruation following menarche.
Other factors responsible for the pathogenesis of endometriosis are:
Estrogen activity
- The primary hormone that is accountable for the spread and expansion of the endometrium is estrogen.
- The increased action of aromatase leads to the locally increased activity of estrogen and the inability of progesterone to have an antagonistic action with estrogen in the endometrial tissue is the determining factor in the establishment of endometriosis.
Reactive oxygen species (ROS)
- An imbalance between the body’s antioxidant capacity and reactive oxygen species (ROS) is the root cause of oxidative stress.
- ROS has the potential to damage nucleic acids and proteins.
- If the enzymatic and non-enzymatic cellular anti-oxidant capacity is decreased, ROS does not get eliminated from the cells and can be the leading cause of endometriosis.
Inflammatory cytokines
- Research shows that patients with endometriosis have elevated serum levels of pro-inflammatory cytokines like IL-1, IL-6, and IL-8.
- This results in the chemotaxis, recruitment, and activation of peritoneal macrophages and the proliferation of monocytes.
- The production of tumor necrosis factor-alpha (TNF-α) by the peritoneal macrophages increases the inflammatory response in the peritoneal fluid.
Epigenetic changes
- It has been proven that the disease affects not only women of reproductive age but also adolescents and younger women with a family history.
- Specific genetic loci have also been identified for the initiation of the disease making some women more prone to the disease than others.
Surgical scar implantation
- After a surgery, such as a hysterectomy or cesarean section, the endometrial cells may attach to a surgical incision.
Immune system disorder
- Due to immune system disorder, the body may be unable to recognize and destroy endometrial-like tissue that is growing outside the uterus.
Angiogenesis
- Endometrium is unique among adult tissues because it undergoes tissue proliferation, secretion, regression, and regeneration during each menstrual cycle.
- The endometrium of women with endometriosis has an increased capacity to proliferate, and thus, implant and grow in the peritoneal cavity.
- The three separate episodes of angiogenesis are:
- Post-menstrual repair during the early proliferative phase
- Mid-proliferative vessel growth under the influence of estrogen.
- Growth of coiled arterioles under the influence of progesterone in the secretory phase
- The endometriotic lesions are surrounded by peritoneal blood vessels. The peritoneal fluid of women with endometriosis contains more angiogenic factors than most of the women without the disease.
- Endometrium of women with endometriosis is found to secrete increased complement-3, complement receptor, and type-3-positive macrophage production than that of patients without endometriosis.
Risk Factors of Endometriosis
Factors associated with increased risk
- Early age at menarche
- Late menopause
- Shorter menstrual length
- Taller height
- Alcohol use
- Caffeine intake
- Nulliparity
- Reduced parity
- Family history of endometriosis
- Disorders of the reproductive tract that prevent the passage of blood from the body during the menstrual periods e.g., Müllerian anomalies
Factors associated with decreased risk
- Parity
- Higher Body Mass Index (BMI)
- Smoking
- Current contraceptive use
- Regular exercise
- Fish and omega-3 fatty acids
The fact that smoking during pregnancy is linked to a lower risk of endometriosis, whereas passive smoking during childhood is linked to a higher risk, is a controversial finding.
Signs and Symptoms of Endometriosis
- Chronic pelvic pain
- Abnormal bleeding
- Infertility
- Dysmenorrhea
- Dyspareunia
- Irregular uterine bleeding
- Dysuria
- Adnexal tenderness
- Adnexal masses
- The clinical features of endometriosis depend on the location and extent of the extra uterine segment.
Bowel endometriosis causes gastrointestinal symptoms like diarrhea, constipation, abdominal pain, and bloating.
Rectovaginal endometriosis may cause bowel irritation, dyspareunia, dysmenorrhea, dyschezia, and rectal bleeding.
Pathophysiology of Endometriosis
- The pathophysiology of endometriosis is still poorly understood in many ways.
- Sampson’s theory suggests that viable cells and menstrual fragments can migrate through the fallopian tubes, infiltrate into the peritoneal cavity, and then multiply and cause chronic inflammation.
- Additionally, the coelomic metaplastic theory and the vascular and lymphatic metastatic theory are necessary to explain some forms of endometriosis.
- For a more comprehensive understanding of the pathogenesis of endometriosis, it is necessary to integrate the roles of oxidative stress and ROS, as well as genetic, epigenetic, and environmental factors.
- In endometriosis, under the influence of hormones, endometrial tissue that is located outside the uterus, thickens, breaks down, and bleeds each month.
- The blood then becomes strapped as the blood cannot exit from the body.
- The trapped blood forms cysts resulting in scar tissues and adhesion that might cause infertility.
- The trapped blood further irritates the surrounding tissue causing pain, which is the most common clinical manifestation of endometriosis.
Diagnosis
Due to a lack of non-invasive, definitive, and consistent biomarkers, endometriosis diagnosis is frequently delayed despite a variety of symptoms. The clinical presentation of the disease differs in women and may be unexpected in the presentation and duration. However, the following methods can be used for making a diagnosis of endometriosis.
- Detailed history taking
- Positive family history
- Pelvic pain
- Benign ovarian cyst
- Pelvic cyst
- Pelvic surgeries
- Infertility
- Gynecological examination: Depending on the location and size of the endometriotic lesion, clinical features may vary. However, the clinical signs may be seen like:
- Tenderness on vaginal examination
- Palpable nodules in the posterior fornix, adnexal masses
- Immobility of the uterus
- Laparoscopy
- Histological biopsy
- Magnetic Resonance Imaging (MRI)
- Transvaginal Ultrasound (TVS)
Management/Treatment of Endometriosis
- A combination of pharmacological and surgical interventions can also be done.
- However, the final decision about the treatment approach that should be followed should be taken collaboratively with the involvement of the patient, after the detailed explanation of all the possible risks and benefits related to each treatment option.
Pharmacological Management
- Since endometriosis is a chronic disease, the treatment is mainly focused on the alleviation of the symptoms.
- The medical treatment focuses on the hormonal alteration of the menstrual cycle to produce the state of pseudo-pregnancy, pseudomenopause, or chronic anovulation.
The following medications have been proposed as the initial course of treatment for endometriosis.
First-line Medical Management
Non-steroidal anti-inflammatory drugs (NSAIDs)
- They provide pain relief.
- Most commonly used along with other pain medications like opioids, ibuprofen, and naproxen.
Progestins
- Progestins inhibit ovulation and create a hypoestrogenic state.
- By directly to the progesterone receptors in the endometrium, they cause decidualization and atrophy of endometriotic lesions.
- The progesterone may be available in the form of tablets
- Medroxyprogesterone
- Norethisterone
- Levonorgestrel
- Injection
- Medroxyprogesterone
- Under skin implant
- Etonogestrel
Combined hormonal contraceptives
- The combined hormonal contraceptives exert their effect by inhibiting follicular development, lowering the effects of LH and FSH.
- This leads to the decidualization and atrophy of the human endometrium.
Second-line Medical Management
Gonadotropin-releasing hormone (GnRH) analogs
- It acts by binding to pituitary receptors and down-regulating the pituitary-ovarian axis.
- It leads to Anovulation, hypoestrogenism, endometrial atrophy, pituitary desensitization, and decreased levels of LSH and FSH.
- However, side effects of hypogonadism may occur like: bone loss, hot flushes, vaginal dryness, and headache.
Surgical Management
- Surgical management of endometriosis involves the excision of the endometrium, adhesions, resection of endometriomas, and restoration of normal pelvic anatomy as much as possible.
- Hysterectomy may be done to treat endometriosis in women who do not wish to conceive.
- The goal of surgery is to remove endometrial tissue while keeping the ovaries intact without harming normal tissue.
- Information on In-vitro fertilization (IVF) procedures should be provided prior to surgery.
- The main advantage of surgical treatment in comparison to pharmacological management is the dual benefits of the ability to enhance fertility capability and pain relief.
- In the case of laparoscopic surgery, all the endometriotic lesions and adhesions are excised.
- By the ablation of the endometrial tissue, the local inflammatory milieu decreases in the pelvic cavity, thus increasing the chances for conception.
Prognosis
- Endometriotic lesions can spontaneously regress in approximately one-third of affected women receiving no treatment.
- Patients with endometriosis have fewer chances for childbearing and a higher risk for miscarriages and ectopic pregnancies in comparison to women with no endometriosis.
- The recurrence rates of endometriosis vary from 6% and 67%.
- Although medical treatment is effective, in 5% to 59% of patients, the pain continues to exist even at the end of the therapy.
- Pain recurrence in cases of treatment cessation has been reported to be approximately 17% to 34%.
Complications of Endometriosis
Endometriosis has been the cause of 71% to 87% of women suffering from chronic pelvic pain. Endometriosis can cause a decrease in the quality of life, negatively affect the health-related quality of life, and crucially hinder the social, emotional, and sexual well-being as well as other domains of life like daily routines, family planning, and efficacy, or productivity of patients in the working environment along with various complications like:
- Infertility
- Sub-fertility
- Chronic pain
- Dyspareunia
- Dyschezia
- Poor quality of sleep
- Constipation
- Complications of surgical procedures
- Anatomical abnormalities due to possible adhesions
- Bowel/bladder dysfunction
- Internal scarring
- Adhesions
- Ruptured cysts
Summary
- Endometriosis is a disease condition where tissue like the lining of the uterus i.e., the endometrium grows outside the uterus causing pain and infertility.
- On average, endometriosis affects 10% to 15% of reproductive-age women.
- The three most common types of endometriosis are superficial peritoneal lesions, ovarian endometriomas, and deep infiltrating endometriomas.
- The widely accepted pathogenesis of endometriosis is Sampson’s theory which focuses on the effects of retrograde menstruation.
- Factors that are associated with the increased risk of endometriosis are early age at menarche, late menopause, nulliparity, reduced parity, etc.
- A combination of pharmacological and surgical interventions can manage the symptoms of endometriosis.
References
- Eskenazi, B., Warner, M. L. (1997, June 1). Epidemiology of endometriosis. Obstetrics and Gynecology Clinics of North America, 24 (2), 235-258. https://doi.org/10.1016/S0889-8545(05)70302-8
- Tsamantioti, E. S., Mahdy, H. (2022). (2022, Sep 6). Endometriosis. National Library of Medicine. https://www.ncbi.nlm.nih.gov/books/NBK567777/
- Olive, D.L., Pritts, E. A. (2001, July 26). Treatment of Endometriosis. The New England Journal of Medicine, 345:266-275.
DOI: 10.1056/NEJM200107263450407 - Nap, A. W., Griffioen, A.W., Dunselman, G. A. J., Steege, J. C. A. B., Thissen, V. L. J. L., Evers, J. L. H., Groothuis, P. G. (2004, Mar 1). Angiogenesis Therapy for Endometriosis. The Journal of Clinical Endocrinology & Metabolism, 89(3), 1089-1095. https://doi.org/10.1210/jc.2003-031406
- Cleveland Clinic. (2022, July, 27). Endometriosis. Retrieved 2022, Dec 30 fromhttps://my.clevelandclinic.org/health/diseases/10857-endometriosis
- Revised American Society for Reproductive Medicine classification of endometriosis. (1997). Fertil Steril. 67 (5), 817–21. https://www.fertstert.org/article/S0015-0282(97)81391-X/pdf