Introduction
Hysterectomy is a major surgical procedure in which the uterus is removed along with or without the removal of the cervix, ovaries, fallopian tubes, or other surrounding structures.
- If the ovaries are removed, menopause occurs and one cannot get pregnant.
- Traditionally, it was performed using either vaginal or abdominal approach.
- More recently, laparoscopic techniques have been used. However, vaginal hysterectomy is preferred as it is cheaper and quicker than laparoscopic surgery.
Epidemiology
- Hysterectomy is the second most common surgery among women in the United States after cesarean section with more than 600,000 procedures performed each year.
- Over one-third of American women has had a hysterectomy by the age of 60.
Indications of Hysterectomy
- Dysfunctional uterine bleeding
- Uterine prolapse
- Severe pelvic adhesions
- Uterine fibroids
- Endometriosis and adenomyosis
- Adnexal tumor
- Chronic pelvic pain
- Pelvic inflammatory disease
- Cervical intraepithelial lesion
- Gynecological cancer like cervical cancer, uterine cancer, and ovarian cancer
- Obstetrical indications
- Uncontrollable postpartum hemorrhage (PPH)
- Placenta increta, percreta, accreta
- Atonic uterus
- Ruptured uterus
- Uterine perforation
- Many transgender and gender-diverse adolescents and young adults pursue hysterectomy for gender affirmation.
Risks and Side Effects of Hysterectomy
- Earlier onset of menopause
- Increased chance of osteoporosis and bone fracture
- Reduced libido (sexual dysfunction)
- Vaginal dryness
- Vaginal prolapse
- Vaginal atrophy
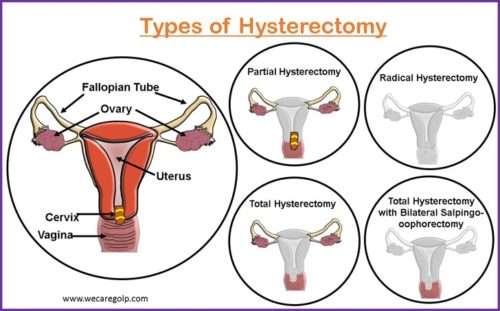
Types of Hysterectomy
It can be done either through the incision of the abdomen or vagina namely abdominal and vaginal hysterectomy respectively.
Hysterectomy according to Part of the Uterus
Total Hysterectomy
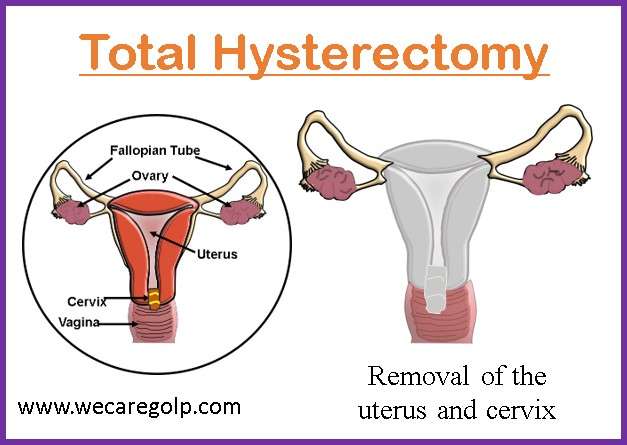
- It refers to the surgical removal of the cervix and uterus.
- It provides the proper drainage of the operation area.
- It is necessary when the cervix needs to be removed for example in cervical cancer.
Partial Hysterectomy
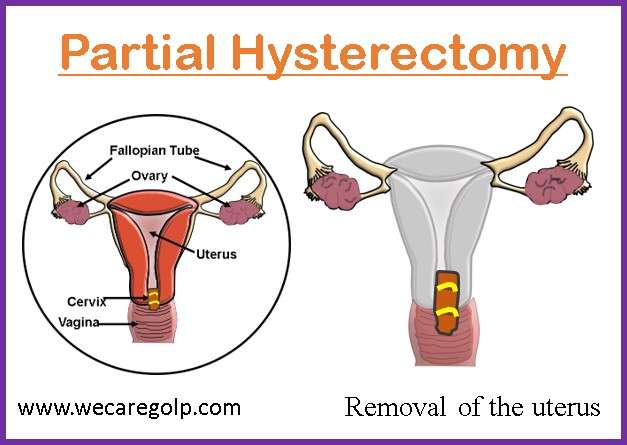
- It is also known as supracervical or subtotal hysterectomy.
- The surgery deals with the removal of the uterus but not the cervix.
Radical Hysterectomy
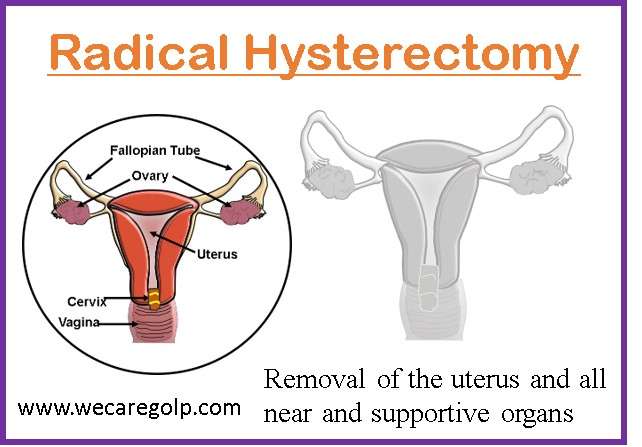
- It is the removal of the uterus, cervix, ovaries, fallopian tubes, and structures that support the uterus and lymph nodes.
Total Hysterectomy with Bilateral Salpingo-oophorectomy
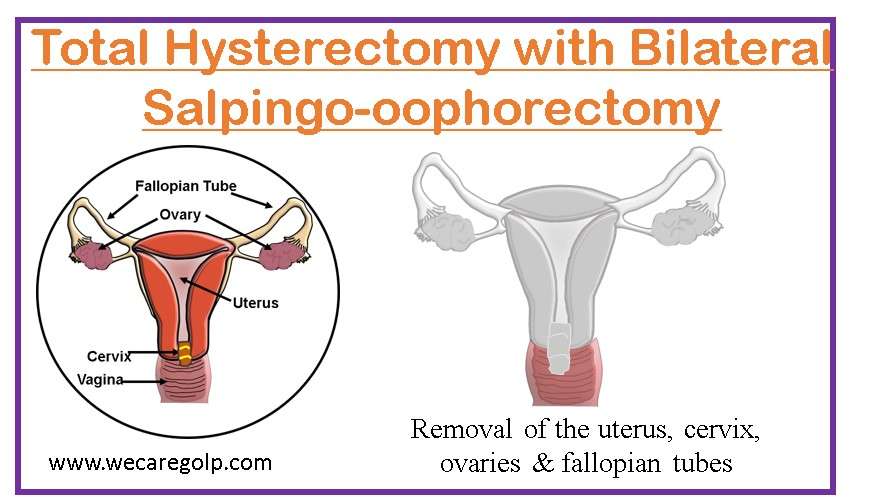
- A total hysterectomy with bilateral salpingo-oophorectomy involves the removal of:
- Fallopian tubes (salpingectomy)
- Ovaries (oophorectomy)
Hysterectomy according to Routes
Minimally Invasive Procedures
It is the most preferred method of hysterectomy. They are:
- Vaginal hysterectomy
- Laparoscopic hysterectomy
- Robotic-assisted hysterectomy
Benefits of minimally invasive procedures
- Typically have a faster return to normal activity.
- Shorter hospital stays
- Less pain after surgery
- Less blood loss during surgery
- Decreased risk for infection
Vaginal Hysterectomy
- It is the surgical removal of the uterus and cervix through an incision made in the top of the vagina.
- The surgical instruments are inserted into the vagina to detach the uterus from ligaments.
- It is the preferred route when technically possible.
Factors affecting vaginal hysterectomy are:
- Vaginal access to the uterus
- Severe endometriosis
- Uterine fibroid
- Adhesion
Advantages of vaginal hysterectomy
- Absence of abdominal scar
- Lower incidence of intestinal complications
- Quicker recovery time
- An associated genital prolapse can be treated at the same time.
Disadvantages of vaginal hysterectomy
- It is unsafe and difficult in case of pelvic adhesions.
- The ovaries cannot be removed in some cases.
- It cannot be done if the size of the uterus is larger than 14 weeks pregnant uterus.
Laparoscopic Hysterectomy
- It is the most preferred method of hysterectomy.
- It is the process of surgical removal of the uterus and cervix. The operation is performed entirely laparoscopically.
- Under this surgical procedure, 3-4 small incisions (each incision 5 mm -15mm in diameter) are made in the abdomen instead of one large big incision.
- One incision is used to insert an endoscope.
- The laparoscope allows the surgeon to view the pelvic organs on a monitor.
- To create a working space, the abdomen is distended with gas.
- Surgical tools are used in other incisions to remove the uterus. It has the shortest hospitalization and recovery.
Types of laparoscopic hysterectomy
- Laparoscopically assisted vaginal hysterectomy
- Laparoscopic supracervical hysterectomy
- Total laparoscopic hysterectomy
Laparoscopically assisted vaginal hysterectomy
- It is a surgical procedure in which a laparoscope and surgical instruments are inserted through the vaginal and abdominal incisions.
- Indications are:
- Uterine fibroids range in size from moderate to small.
- Uterus is slightly larger than normal.
- Endometriosis
Laparoscopic Supracervical hysterectomy
- It is also known as subtotal or partial hysterectomy.
- This procedure is performed by inserting a laparoscope and surgical instruments through several small abdominal incisions.
- The uterus is removed in small pieces through one of the incisions and the cervix is left intact.
- Indications are:
- Removal of uterine fibroids of any size
- Removal of the uterus of any size
Total Laparoscopic Hysterectomy
- The procedure is performed entirely laparoscopically.
- It is the removal of the uterus and cervix by inserting a laparoscope and surgical instruments through several small incisions in the abdomen.
- Indications are:
- Removal of uterine fibroids, which are small to moderate in size
- No chance of uterine or ovarian cancer is present.
Robotic-assisted Total Hysterectomy
- It is a minimally invasive method of removal of the uterus.
- Robotic devices are used to remove the uterus through 3-5 small abdominal incisions (each incision 8 mm-12 mm in diameter).
- Advantages are:
- It improves surgical precision and accuracy.
- It eliminates hand tremors.
Abdominal Hysterectomy (Open Surgery)
- Laparotomy is yet another name for it.
- It is the surgical removal of the uterus with the incision made in the abdomen which may be done horizontally or vertically.
- It is the most invasive method.
Indications
- Significant uterine enlargement
- Inadequate transvaginal access
- Adnexal pathology and fixation
Disadvantages
- Abdominal hysterectomy has the highest incidence of febrile morbidity.
- It possesses the greatest risk of intraoperative hemorrhage and surgical site infections (SSI).
- It takes the longest hospitalization.
- The recovery rate is slower.
Affecting factors
- Outcome of surgery
- Comparative rate of complications
- History of previous abdominal surgery
- Parity of women
- Size and mobility of the uterus
- Duration of surgery
- Duration of hospital stay
- Overall recovery rate
- Quality of life along with long-term effects including mental health and sexual function
Procedure of Hysterectomy
Preparation before Surgery
- Suggest the patient to
- Stop drinking alcohol 1 week before the surgery as alcohol affects how the human body reacts to medicines.
- Quit smoking one month prior to the surgery if the patient is a smoker. In the case of smokers with COPD, quit smoking two months prior the surgery.
- Keep the blood sugar in the normal range before the surgery, if the patient has diabetes mellitus.
- Keep the patient in NPO for 6-8 hours.
- Review of the patient’s medical, surgical, and family history.
- Gather information on:
- Patient allergies to food, medications, or environment
- Current medications with dosages
- Pre-morbid disease conditions
- Review the laboratory findings prior to the surgery.
- Get the imaging reports like ultrasound, MRI, and chest X-Ray.
- Promote patient understanding of the surgical procedure.
- Prepare the patient psychologically.
- Support and teach the patient deep breathing, spirometry, early ambulation, and splinting while coughing.
- Administer pre-operative medications including antibiotic prophylaxis.
- Remove the pieces of jewelry and oral dentures.
- Insert the urinary catheter to empty the bladder.
- Prepare the abdominal or vaginal area for surgery.
Patient Care during Surgery
- Re-check the arrangements with the pre-operative checklists.
- Ensure patient safety, monitor the implementation of sterile techniques
- Clean the vagina and/or abdomen with a sterile solution.
- Check the amount of blood loss during the surgery.
- Perform blood transfusion if necessary.
- Maintain fluid and electrolyte balance.
- Send the sample specimen to the laboratory as needed.
Patient Care after Surgery
- Manage the pain.
- Monitor vital signs frequently.
- Help for early ambulation to promote pulmonary ventilation.
- Help to perform deep breathing and coughing exercises and spirometry.
- Splint or support the site of the incision while coughing.
- Support to perform leg exercises to prevent deep vein thrombosis.
- Provide psychological support.
- Teach the patient not to lift anything heavier than 5-10 lbs for six weeks or more post-operatively.
- Provide discharge teachings on medications, follow-up, diet, exercises, etc.
Complications of Hysterectomy
- Hemorrhage
- Shock
- Pneumonia
- Surgical site infections/Sepsis
- Pulmonary complications: bronchitis, pneumonia, pulmonary collapse
- Venous thrombosis
- Cystitis
- Vaginal wall prolapse
- Vaginal fistula formation
- Trauma to adjacent organs like bladder or bowel, ureter
- Post-operative anesthetic complications like cyanosis, vomiting
- Menopausal symptoms
- Incisional hernia
Summary
- A hysterectomy involves removing all or part of the uterus.
- This procedure aims to relieve discomfort caused by disease or injury to the uterus.
- It is a major operation that can have risks and side effects.
- It is usually only an option when other treatments do not help enough.
- In the case of cancer, it can be unavoidable to remove the tumor.
References
- Clayton, R. D. (2006, Feb). Hysterectomy. Best Practice & Research Clinical Obstetrics & Gynaecology, 20(1), 73-87. https://doi.org/10.1016/j.bpobgyn.2005.09.007
- Kovac, S. R. (1995, Jan). Guidelines to determine the 3route of hysterectomy. Obstetrics & Gynecology, 85(1), 18-23. DOI: 10.1016/0029-7844(94)00318-8
- Carlson, Karen J. (1997, Dec) Outcomes of hysterectomy. Clinical Obstetrics and Gynaecology, 40(4),939-946. DOI: 10.1097/00003081-199712000-00029
- Kjerulff, K. H., Langenberg, P.W., Rhodes, J.C., Harvey, L.A., Guzinski, G.M., Strolly, P. D. (2000, Mar 1). Effectiveness of hysterectomy. Obstetrics & Gynecology, 95 (3), 319-326. DOI: 10.1016/s0029-7844(99)00544-x
- Hoffmann, M. (2021, Feb 4). Hysterectomy. WebMD. https://www.webmd.com/women/guide/hysterectomy
- Mayo Clinic (2021, April 27). Abdominal hysterectomy. https://www.mayoclinic.org/tests-procedures/abdominal-hysterectomy/about/pac-20384559
- Office on Women’s Health. (2022, Dec 29). Hysterectomy. https://www.womenshealth.gov/a-z-topics/hysterectomy
- ACOG. (2021, Jan). Hysterectomy. https://www.acog.org/womens-health/faqs/hysterectomy