Introduction
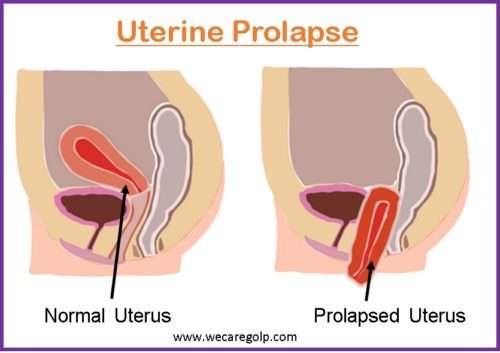
Uterine prolapse is a condition characterized by the descent of the uterus and cervix, within or outside the vaginal canal from the vaginal introitus due to weak or damaged pelvic supporting structures. The uterus is supported by muscles and ligaments which help maintain the normal anteverted and anteflexed position of the uterus.
- Uterine prolapse is one of the forms of female genital prolapse which is also known as pelvic organ prolapse.
- It may also be associated with the prolapse of pelvic organs like the bladder, rectum, bowel, or top of the vagina from the normal anatomic location toward or through the vaginal opening.
- The impact of uterine prolapse on quality of life is enormous as it adversely affects the physiological processes, functions, and quality of life.
- However, uterine prolapse is often underreported due to social stigma related to the reproductive functioning ability of women.
Support of the Uterus
The pelvic support system comprises:
- Muscular support
- Ligamentous support
- Mechanical support
Muscular Support
- The pelvic diaphragm is formed by the levator ani muscles which consist of pubococcygeus and iliococcygeus muscles.
- Other muscles supporting the pelvis beside the levator ani muscles are:
- Bulbospongiosus muscle
- External anal/urethral sphincter
- Superficial transverse perinei
- Deep transverse perinei
- Loss of tonicity of the pelvic diaphragm may lead to uterine prolapse.
- The most common cause of loss of tonicity is damage to the pudendal nerve.
- Uterine prolapse occurs when the muscles and ligaments of the pelvic floor stretch and become weaker. The uterus then slips down into the vagina.
Mechanical Support
- Normally, the uterus is located at an anteverted and anteflexed position.
- The uterus bends towards the urinary bladder which provides mechanical support to the uterus.
- Loss of anteflexion or retroversion of the uterus is the first step of uterine prolapse.
Anteverted uterus
- The normal position of the uterus is an anteverted uterus.
- The uterus tips forward towards the cervix.
- The whole uterus makes the right angle with the longitudinal axis of the vagina.
Retroverted uterus
- The uterus is angled slightly posteriorly.
- The backward displacement of the uterus causes the angles of the version or flexion to look backward.
Anteflexed uterus
- It is the normal position of the uterus in which the fundus of the uterus is tilted forward.
- The longitudinal axis of the body makes an angle of 170˚ with the longitudinal axis of the cervix.
Retroflexed uterus
- The uterus tilts backward rather than forward.
Ligamentous Support
- Ligaments keep the uterus in an anteverted and anteflexed position. Thus, the ligaments prevent the retroversion of the uterus and uterine prolapse.
- Uterus is primarily supported by three ligaments:
- Cardinal/Mackenrodt ligament
- Uterosacral ligament
- Pubocervical ligament
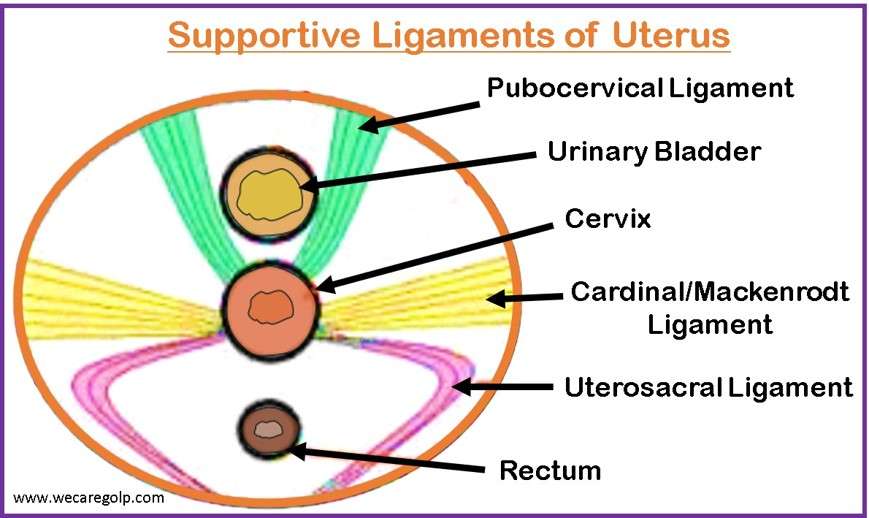
Cardinal ligament/ Mackenrodt ligament
- It is the most important ligament supporting the pelvic organ.
- It is also known as the transverse cervical ligament.
- It is attached from the lateral side of the cervix and the vagina to the lateral pelvic wall.
- Ureter and uterine vessels are located near the cardinal ligament and may be injured during surgeries if manipulated.
Uterosacral ligament
- It is also known as the Sacro-cervical or recto-uterine ligament.
- It is extended from the posterior aspect of the cervix and vagina and directed backward to surround the rectum.
Pubocervical ligament
- It is extended from the anterior of the cervix and vagina and directed forward to surround the urethra below the bladder.
Epidemiology
- Evidence suggests that uterine prolapse affected women of all times.
- The global prevalence of uterine prolapse has been reported to be around 9%.
- The prevalence based on the symptoms is 3-6% and up to 50% when defined by vaginal check-ups.
- The incidence of uterine prolapse is about one in 250 pregnancies.
Types of Uterine Prolapse
Uterovaginal prolapse
- It is the prolapse of the uterus including the cervix and upper vagina.
- It is the commonest type of uterine prolapse.
- It is accompanied by cystocele.
Congenital prolapse
- It is commonly seen in young nulliparous. So, it is also known as nulliparous prolapse.
- The most common cause of congenital prolapse is genetic predisposition.
- It can be managed by cervicopexy or sling surgery.
- The slings are synthetic supporting structures that are commonly made of mersilene tape.
- The sling may be used anteriorly or posteriorly to support the uterus.
- However, the complications of the sling surgery may be:
- Injury to the genitofemoral nerve
- Obstruction on the sigmoid colon
- Injury to mesenteric vessels
- Ureteric injury.
Grading of Vaginal Wall Prolapse
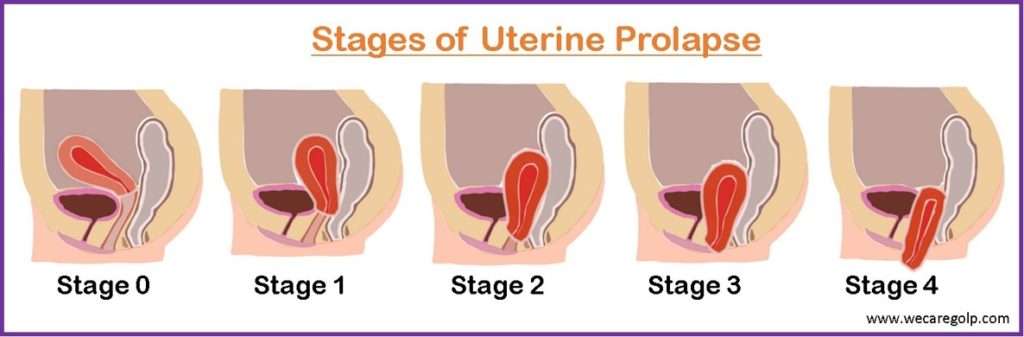
Pelvic Organ Prolapse Quantification System (POP-Q System)
- It is a site-specific, objective method for describing, quantifying, and grading pelvic support.
- It is a reliable and reproducible classification system.
- The fixed point of reference throughout the POPQ system is the hymen.
| Stage | Features |
| Stage 0 | No prolapse |
| Stage I | Most distal prolapse > 1 cm above the hymen |
| Stage II | Most distal prolapse is between > 1 cm above and 1 cm below the hymen |
| Stage III | Most distal prolapse is > 1 cm below the hymen but 2 cm shorter than the total vaginal length |
| Stage IV | Complete eversion |
Baden-Walker Halfway Scoring System
- It is an older classification system that is not reproducible.
- It is based on the level of protrusion.
| Grade | Features |
| Grade 0 | No prolapse |
| Grade 1 | Halfway to the hymen |
| Grade 2 | To the hymen |
| Grade 3 | Halfway past the hymen |
| Garde 4 | Maximum descent |
Causes of Uterine Prolapse
The normal anatomy of the uterus is in an anteverted and anteflexed position. The uterus is held in place within the pelvis by a group of muscles and ligaments (pelvic floor muscles). Several factors may lead to a weakening of the pelvic floor support system that may further lead to uterine prolapse.
- Birth Injury
- Damage to the supportive tissue and ligaments due to multiple pregnancies and vaginal births
- Giving birth to a large baby
- Peripheral nerve injuries such as pudendal nerve
- Vacuum delivery before the cervix is fully dilated
- Prolonged bearing down in the second stage of labor
- Heavy work just after delivery without any rest or pelvic floor exercises
- Postpartum cough
- Congenital weakness of the uterus and vagina
- Menopausal atrophy
- Atonicity and asthenia after menopause
- A nulliparous woman who has spina bifida, congenital weakness of pelvic floor muscles, etc.
- Raised intra-abdominal pressure due to chronic bronchitis, abdominal tumors, ascites, and obesity.
- Surgeries such as abdominoperineal excision of the rectum, radical vulvectomy, etc.
Risk Factors of Uterine Prolapse
- Being older when having the first baby
- Adolescent pregnancy
- Insufficient rest during and immediately after pregnancy
- Having multiple vaginal births
- Frequent pregnancies close together
- Precipitate labor
- Prolonged labor
- Obstructed labor
- Delivery by unskilled birth attendants
- Ageing (lack of estrogen due to menopause)
- Obesity
- Frequent heavy lifting
- Chronic coughing
- Chronic constipation
- Prior pelvic surgery
- Frequent straining during bowel movements
- Genetic predisposition to weakness in connective tissue
Signs and Symptoms of Uterine Prolapse
The clinical features of uterine prolapse depend on the degree of the prolapse.
- Sensation of something passing through the vagina
- Sensation of vaginal fullness or pressure
- Feeling heaviness or pulling in the pelvis
- Pain in pelvis or abdomen, sacral back pain with standing (due to stretching of uterosacral ligaments)
- Voiding difficulties
- Urgency and frequency of micturition
- Retention of the urine (incomplete bladder emptying)
- Stress incontinence (urine leak while coughing, sneezing, and laughing)
- Urinary infections
- Constipation
- Dyspareunia (Coital difficulty)
- Vaginal spotting from ulceration of the protruding cervix or vagina
- Feeling bulging in the vagina, especially when coughing, sneezing, or physical exertion, after long periods of standing or at the end of the day.
- Decubitus ulcers due to venous congestion
Pathophysiology of Uterine Prolapse
- Uterine prolapse occurs when any of the supportive structures of the uterus are disrupted.
- The levator ani muscles can weaken, causing the uterus to lose support due to: vaginal birth (parts of the levator ani muscle can detach from the bony pelvis) or age-related musculature changes.
- The uterosacral ligaments can also be stretched and weakened during pregnancy, vaginal birth, or an injury. This can cause the uterus to be poorly suspended or positioned so that it is no longer supported by the pelvic floor muscles.
- The uterus can collapse downward due to problems with the vaginal wall, such as trauma or a loss of smooth muscle support in the wall.
- Due to its anatomic relationship with the apical vagina, the uterus drags the upper portion of the vagina, also known as the apical vagina, along with it when it prolapses.
- Moreover, the connective tissues and pelvic musculature are also estrogen-sensitive and respond to changes in estrogen levels.
- Uterine prolapse can be exacerbated by estrogen deficiency, which can occur during menopause and affect the production of collagen, which is necessary for the creation of connective tissue that makes up fascia and ligaments. It is also one reason why connective tissue diseases can lead to uterine prolapse in some people.
Diagnosis of Uterine Prolapse
- History taking
- Physical Examination
- Bimanual pelvic examination
- Stress incontinence test
- Vaginal speculum test
- Rectal examination
- Lab Investigations
- Blood, urea, sugar
- Urine routine examination/microscopic examination (to look for an infection)
- High vaginal swab
- Imaging
- CT scan
- X-Ray
- Ultrasound (to rule out other pelvic problems)
- MRI (suspect more than one prolapsed organ or to plan surgery)
- Cystoscopy (to examine the bladder and urethra)
- Intravenous pyelogram (IVP) or renal sonography (in case of ureteral obstruction due to complete prolapse)
Management of Uterine Prolapse
The management of uterine prolapse can be either a surgical or non-surgical approach and is based on the degree of prolapse, age of the woman, severity, current health status, and her plans regarding children.
Conservative Management
- Pelvic floor muscles exercise
- Losing the excessive weight
- Treatment of chronic cough and constipation
- Avoiding heavy weight lifting
- Estrogen therapy for post-menopausal women
- Avoid future pregnancy too soon
Kegel exercise
- It is the exercise that is done to strengthen and tighten the pelvic floor muscles that support the urinary and reproductive systems of the human body.
- Identification of the right muscle and repeated controlled contraction and release of the pelvic muscles is done during the Kegel exercise.
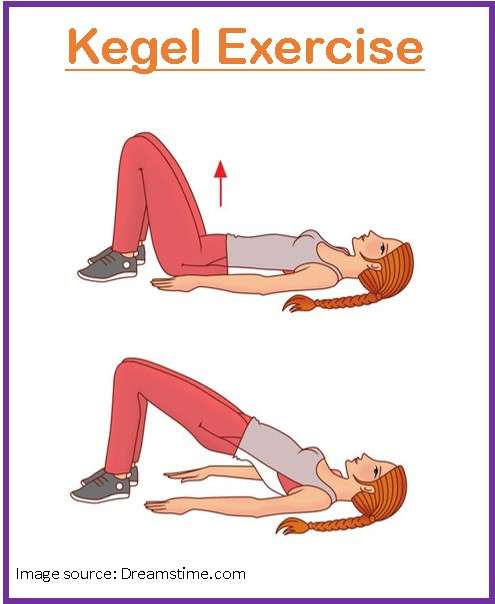
Benefits of Kegel exercise
- Increased pelvic support
- Protection from the physical stresses of childbirth
- Prevention of urinary incontinence
- Restoration of sexual function
Steps of Kegel exercise
- Sit or stand in a relaxed, comfortable position.
- Locate the perineal muscles and contract them.
- Hold the contraction for 5 – 10 seconds.
- Keep breathing normally.
- Keep the muscles of the stomach and buttocks relaxed.
- Release the contraction for about 10 seconds.
- Repeat the contraction hold release sequence 12-20 times.
- Repeat the exercise three or four times a day.
Mechanical Management
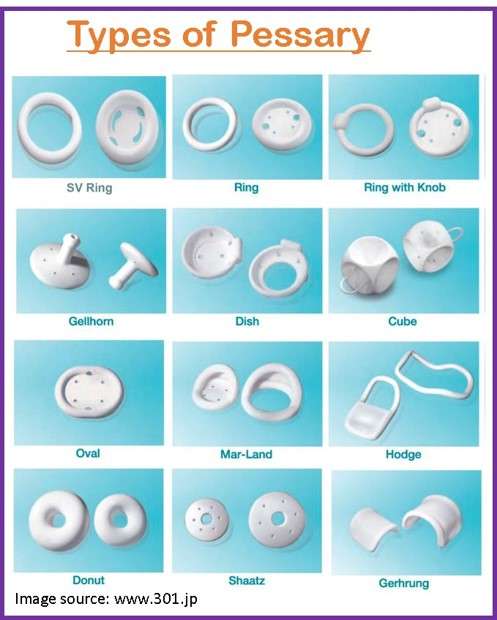
Pessary
- A pessary is a flexible mechanical device that is inserted into the upper part of the vagina to provide support to the pelvic structures.
- The use of pessary can be dated back to the era of Hippocrates who used pomegranate soaked in vinegar as a vaginal pessary.
- Ambrose Pare in the late 16th century first developed a ring type of pessary.
- Initially, pessaries were made up of wood, cork, silver, or gold.
- Now, pessaries are commonly made up of silicon and are available in different sizes.
- The most common type of pessary in use is ring pessary followed by Gellhorn and cube or donut pessaries.
- The two basic forms and working mechanisms for pessaries are: supportive and space-filling.
- The support pessary is kept on the posterior fornix and generally rests above the pubic bone/pelvic floor, e.g., Ring pessary, Shaatz pessary, etc.
- A space-occupying pessary is most often used for severe prolapse, e.g., Cube, Inflatoball, Donut pessary, etc.
- A pessary does not cure uterine prolapse but only holds the genital tract in position.
Qualities of pessary
- Made of incorruptible material that resists decomposition
- Maintains the normal uterine position
- Allows for natural movement
- Should be worn without pain
- Should not excite leucorrhea or menorrhagia.
Indications of pessary
Pessaries are indicated for diagnostic or therapeutic purposes for uterine prolapse with the following conditions.
- Symptomatic when the surgery is not, or yet possible.
- Unfit for surgery, e.g., during pregnancy, high-risk case for surgery
- Who has recently given birth
- Who is awaiting surgeries
- Elderly women with many co-morbidities
- Patient’s choice
- The choice of pessary depends on the degree of prolapse and the choice of women.
- The size of the pessary also depends on the size of the vagina.
- Before insertion, the pessary is kept in hot water for a few minutes so that the pessary becomes soft and easy to insert.
- Pessary should be removed, cleaned, and re-inserted at regular intervals of 6-12 months.
- If left in place for longer periods, it may lead to the formation of a vesicovaginal fistula.
Complications of pessary
- Irritation of vaginal mucosa with discharge, odor, ulceration, and bleeding.
- Perforation of bowel or bladder
- Cervical entrapment
- Small bowel prolapses
- Bowel and ureteral obstruction
- Infection
- Latex allergy
Surgical Management
The type of surgery to be done for the uterine prolapse depends on
- The age of the patient,
- Degree of uterine prolapse, and
- Woman’s desire to retain the uterus.
Purposes of surgery
- To relieve symptoms
- To restore anatomy
- To restore sexual functions
Types of Surgery
Hysterectomy
- Hysterectomy is the surgical procedure in which the uterus is removed.
- It may be done either through a vaginal or an abdominal approach.
- Indications:
- Post-menopausal prolapse
- Uterine pathologies like small fibroids or adenomyosis
- Menstrual disorders like dysfunctional uterine bleeding
Colporrhaphy
- Colporrhaphy is a minimally invasive surgical procedure that strengthens the supporting pelvic muscles and tissues.
- It is a less invasive type of reconstructive surgery.
- Under this surgery, a surgeon makes an opening in the vagina and reinforces the tissue layer under the vaginal skin with strong sutures.
- Indications
- Symptoms not relieved by conservative management like Kegel exercise, pelvic floor therapy, or pessary insertion.
- Advantages
- Incision is small
- Faster post-operative recovery
- No inpatient hospitalization is required
- Complications
- Bleeding
- Infection
- Pain with intercourse
- Difficult bowel movements
- Failure of the surgery
Types of colporrhaphy
Anterior colporrhaphy
- It is performed to repair anterior vaginal wall prolapse.
- It is also known as cystocele repair.
Posterior colporrhaphy
- It is done to repair the posterior vaginal wall and perineum.
- It is also known as rectocele repair.
- It is commonly performed along with an anterior colporrhaphy or vaginal hysterectomy requiring pelvic floor repair and as a part of Fothergill’s repair.
Fothergill’s repair (Manchester Operation)
- Manchester-Fothergill procedure is a type of surgery in which normal support of the uterus is restored without removing the uterus.
- Under this surgery, an incision is made in the top or bottom of the vaginal wall.
- The stronger tissues that are underneath the soft skin that lines the inside of the vagina are stitched together.
- It preserves the normal menstrual function of women. However, childbearing ability is lost after the surgery.
Cervical amputation
- Under this procedure, cervical amputation (supra vaginal part) is done.
- The amputation may lead to cervical stenosis that may lead to recurrent 2nd-trimester abortions.
- The suture used on the posterior lip of the cervix covered with cervical flap after the amputation is known as the Sturmdorf suture.
Plication of cardinal ligament
- Normally, the anterior support to the uterus by the pubocervical ligament is weaker compared to the lateral support by the cardinal ligament.
- In Fothergill’s repair surgery, the cardinal ligament is plicated anteriorly after the cervical amputation.
- Shirodkar modification of Fothergill’s repair can be performed under which only plication of cervical ligaments is done.
- This allows the female to have her normal pregnancy.
Complications of Manchester Surgery
- Bleeding
- Damage to the bladder, ureter
- Nerve damage
- Bowel obstruction
- Infection
- Urinary symptoms
- Anterior prolapse
- Posterior vaginal prolapse
Prevention of Uterine Prolapse
Uterine prolapse cannot be prevented completely. However, the following preventive measures may help to prevent uterine prolapse.
During Labor and Pregnancy
- Multiple childbirths with short intervals cause uterine prolapse. So, women should be advised to avoid pregnancies in quick succession.
- Effective management of different stages of labor is essential.
First stage:
- Avoid bearing down
- Breech, forceps, or vacuum delivery should not be attempted before full dilatation of the cervix.
Second Stage:
- Avoid the prolongation of the second stage of labor.
- Perform episiotomy if needed or if tears or overstretching of the perineum may be present.
Third Stage:
- The episiotomy or tears should be stitched carefully.
During Puerperium
- Treat chronic cough and constipation.
- Avoid exerting physical exercises and prolonged standing.
General
- Prevent constipation
- Get regular exercise and a healthy weight.
- Avoid heavy lifting
- Control and manage chronic cough
- Avoid weight gain
- Quit smoking
- Perform Kegel exercise
- Follow a diet rich in fiber and fluids to prevent constipation and straining
Complications of Uterine Prolapse
- Cystocele- Descent of bladder into the vagina
- Rectocele- Descent of rectum into the vagina
- Enterocele- Descent of small intestine into the vagina
- Urinary and fecal incontinence
- Long-term morbidity
Prognosis
- The prognosis of uterine prolapse is usually good with early detection and treatment.
- However, a prolapse may recur on occasion. It happens more often if a woman has a severe prolapse and obesity and is younger than 60.
- A good lifestyle and treatment plan can prevent the recurrence of uterine prolapse.
- Whether temporary or permanent, pessaries can be very effective.
- A prolapsed uterus can be supported or removed by surgery.
Summary
- Uterine prolapse, also known as the prolapse of pelvic organs is the descent of the uterus within or outside the vagina.
- The approximate global prevalence of uterine prolapse is reported to be 9%.
- Uterine prolapse occurs due to weakening of the muscular, ligamentous, and mechanical support of the pelvic floor, which may be due to birth injury, congenital weakness of the uterus and vagina, and atonicity after menopause.
- The clinical features associated with uterine prolapse are the sensation of vaginal fullness/ pressure, coital difficulty, lower abdominal discomfort, etc.
- Uterine prolapse can be managed by conservative, mechanical, or surgical management.
References
- Badacho, A. S., Lelu, M. A., Gelan, Z., & Woltamo, D. D. (2022, Jan 21). Uterine prolapse and associated factors among reproductive-age women in south-west Ethiopia: A community-based cross-sectional study. PloS ONE, 17(1), e0262077. https://doi.org/10.1731/journal.pone.0262077
- Maher, C. F., Carey, M. P., & Murray, C. J. (2001, Jun). Laparoscopic suture hysteropexy for uterine prolapse. Obstetrics & Gynecology, 97(6), 1010-1014. https://doi.org/10.1016/S0029-7844(01)01376-X.
- Ayhan, A., Esin, S., Guven, S., Salman, C., & Ozynuncu, O. (2006, Jan 20). The Manchester operation for uterine prolapse. International Journal of Gynaecology & Obstetrics. 92(3), 228-233. https://doi.org/10.1016/j.ijgo.2005.12.002
- Downing, K. T. (2011, Nov 14). Uterine Prolapse: From Anttiquity to Today. Obstetrics and Gynaecology International, 2012, https://doi.org/10.1155/2012/649459
- Burgio, K. L., Robinson, J.C., & Engel, B. T. (1986, Jan). The role of biofeedback in kegel exercise training for stress urinary incontinence. American Journal of Obstetrics and Gynaecology, 154(1), 58-64. doi:10.1016/0002-9378(86)90393-5
- Robert, M., Schulz, J. A., & Harvey, MA. (2013, Jul). Technical Update on Pessary Use. Journal of Obstetrical and Gynaecology Canada, 35(7), 664-674. doi:10.1016/s1701-2163(15)30888-4
- Stetson, D. (2019, Mar). Manchester-Fothergill Procedure and Vaginal Wall Prolapse Repair. Michigan Medicine. Retrieved on 2023. Feb 1 from https://www.med.umich.edu/1libr/Gyn/Manchester-Fothergill.pdf
- Cleveland clinic. (2022, July 9). Uterine Prolapse. Retrieved on 2023. Feb 1 from https://my.clevelandclinic.org/health/diseases/16030-uterine-prolapse

Good day — how long is the recovery period after a pessarie operation. Please
Hi!
A pessary is a flexible mechanical device that is inserted into the upper part of the vagina to provide support to the pelvic structures. It is not an operation and does not cure uterine prolapse but only holds the genital tract in position. It can be used to ease the symptoms of moderate or severe prolapses and is a good option if you cannot or would prefer not to have surgery
Hope it helps you.