Introduction
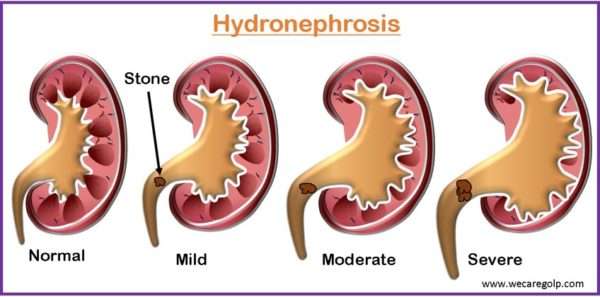
Hydronephrosis is defined as dilatation and distension of one or both kidneys’ renal collecting systems due to blockage of urine outflow distal to the renal pelvis (i.e., ureter, urinary bladder, and urethra).
- Hydronephrosis is described as aseptic dilatation of the kidney’s pelvicalyceal system due to partial or total obstruction of urine outflow.
- The term hydroureter refers to ureter dilation caused by a blockage in urine outflow. It can occur alone or in conjunction with ureter dilation, resulting in hydroureteronephrosis.
- It is a serious concern in patients with abdominal or pelvic disease because increasing dilatation of the upper urinary tract can result in acute kidney damage and, if not treated, irreversible nephron loss.
- The presentation of hydronephrosis might be acute or chronic, physiologic (particularly prevalent in pregnant women) or pathologic, unilateral, or bilateral.
- Prenatally diagnosed hydronephrosis infants have an increased risk of UTIs. It elevates the possibility of underlying kidney dysfunction.
Incidence
- In the general population, the frequency ranges from 0.15% to 0.67%.
- The prenatal ultrasonography frequency is one instance per 100 to 200 fetuses.
- The ratio of men to women is 2:1.
- Bilateral kidney instances account for 10% to 20% of all cases.
- The case fatality rate is 3.1 per 100,000 people.
- It can strike at any age.
- Women have a greater prevalence of hydronephrosis than males in younger patients (aged 20-60 years).
- Men have a greater frequency of hydronephrosis than women in older individuals (>60).
Causes of Hydronephrosis
The causes of hydronephrosis can be classified as intrinsic and extrinsic causes.
| Intrinsic causes | Extrinsic causes |
| Renal stones | Peripelvic cysts |
| Malignancy | Retrocaval ureter |
| Ureteropelvic junction Stenosis | Malignancy |
| Ureteral strictures from prior inflammation | Trauma |
| Renal cysts | Retroperitoneal fibrosis |
| Posterior urethral valves | Prostate Abscess |
| Benign Prostatic Hyperplasia | Renal artery aneurysm |
| Neurogenic bladder | Cervical cancer |
| Endometriosis | Retroperitoneal hemorrhage |
| Ureteral calculus | Inflammatory bowel disease |
| Cystocele | Pregnancy |
The majority of instances of hydronephrosis in children are caused by anatomical defects. Urethral valve stricture, as well as stenosis at the ureterovesical or ureteropelvic junction, are examples of these.
Classification of Hydronephrosis
Unilateral and Bilateral hydronephrosis
Hydronephrosis can be unilateral or bilateral, depending on the location of the blockage to urine flow.
Unilateral hydronephrosis
- When the blockage is above the level of the bladder, it causes unilateral hydronephrosis. The incidence of unilateral hydronephrosis was determined to be 1:100 from birth to 80 years of age.
- The most prevalent cause is ureteric calculus, which affects men more frequently, with a peak incidence in the third to fourth decade of life.
- The major diagnostic modality is the USG abdomen.
- Depending on the cause and severity, either conservative or surgical therapy is used.
Bilateral hydronephrosis
- Bilateral hydronephrosis occurs when both kidneys are affected.
- It is characterized by dilatation of the renal pelvis, calyces, and ureter.
- It arises as a result of urinary tract blockage and results in a build-up of back pressure in the urinary system.
- It may compromise renal function and eventually lead to renal failure.
- Although most instances are clinically quiet, it might be discovered as an accidental discovery during the investigation of an unrelated reason. It causes signs and symptoms in a small percentage of people.
- The most prevalent cause is renal calculus, however, there are other non-calculus etiologies vary depending on age and gender.
Acute and Chronic hydronephrosis
Acute hydronephrosis
- Acute hydronephrosis is defined as hydronephrosis, which, when addressed, permits the complete return of renal function.
- It can have little anatomic disruption to the renal parenchyma.
Chronic hydronephrosis
- A chronically dilated system, on the other hand, may be accompanied with
- Papillae compression,
- Thinning of the parenchyma around the calyces, and
- Septal coalescence between calyces.
- In contrast to the acute case, even with the repair of the obstructive condition, the loss of function in chronic hydronephrosis is permanent.
- Cortical atrophy eventually advances to the point that just a narrow margin of parenchyma remains.
- Urine flow obstruction occurs gradually over weeks or months in chronic hydronephrosis.
- This is frequently painless and has little or no symptoms.
Partial and complete hydronephrosis
- Partial hydronephrosis can be challenging to diagnose.
- Urinary output can vary in partial hydronephrosis whereas complete obstruction is one of the most common causes of anuria.
Signs and Symptoms of Hydronephrosis
Clinical symptoms differ based on the severity of the illness, the degree, and the location of the blockage. Presentations that might be given include:
- Asymptomatic (developing slowly or partially)
- Pain (due to acute full or partial blockage)
- Suprapubic discomfort with radiation to the labia or testicle (due to lower urinary tract blockage)
- Urine volume changes
- Anuria (due to complete urethral or bilateral ureteral blockages)
- Polyuria
- GFR decreases in partial or total bilateral hydronephrosis.
- Hematuria
- Constant dull pain with intermittent episodes of severe pain.
- Abdominal mass
- Nausea and vomiting
- Urinary tract infections (UTIs)
- Fever
- Painful urination (dysuria)
- Urinary retention
- Palpable bladder
- Increased urinary urgency
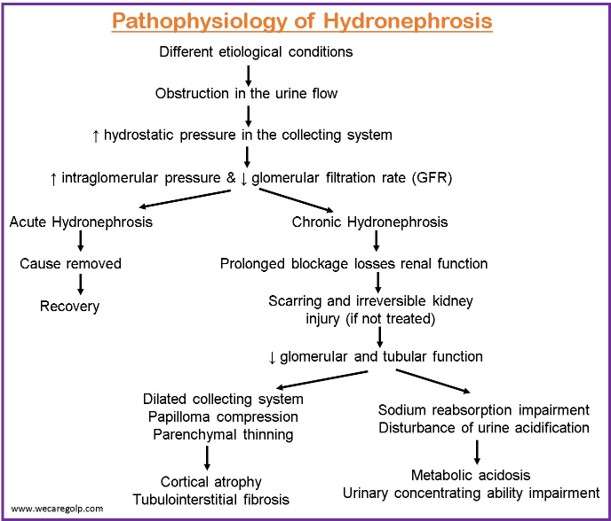
Pathophysiology of Hydronephrosis
- Due to the etiological conditions, there is an obstruction in the flow of urine
- The restriction of the outward flow of urine causes an increase in the collecting system’s hydrostatic pressure.
- This raises intraglomerular pressure, which influences the glomerular filtration rate (GFR).
- The extent of renal function loss is determined by the duration and severity of the blockage. If the blockage is not removed, it can cause scarring and irreversible kidney injury, as well as a reduction in glomerular and tubular function.
- As a result, hydronephrosis might be called acute if kidney function recovers after a blockage is removed.
- Even if the blockage is removed, kidney function does not improve in chronic hydronephrosis.
- Prolonged blockage results in a dilated collecting system, papilloma compression, and parenchymal thinning, eventually leading to cortical atrophy and tubulointerstitial fibrosis.
- Physiologic consequences include sodium reabsorption impairment, disturbance of urine acidification leading to metabolic acidosis, and urinary concentrating ability impairment.
Diagnosis of Hydronephrosis
Urinalysis
- Pyuria indicates the presence of inflammation in the urine.
- Infection is indicated by leukocyte esterase or nitrites.
- Hematuria can be caused by stones, cancer, or an infection.
Blood investigation
- BUN and creatinine levels are elevated in bilateral hydronephrosis, indicating renal impairment.
- Hyperkalemia and acidosis are symptoms of acute renal insufficiency.
Imaging modalities
Ultrasonography
- In most cases, ultrasonography (USG) is the best first-line test.
- In identifying ureteral stones, it is not as sensitive as CT.
- USG is mostly used to rule out obstructions and identify aberrant formations.
- It allows for the simultaneous evaluation of nearby parts (e.g., prostate and gynecologic structures)
CT scan
- It is the most effective imaging modality for detecting stones When obstructive stones are detected, this is the first line of defense.
- It is also preferable for pregnant ladies.
IV pyelography
- In IV pyelography, Contrast material is injected into the veins, and X-rays are obtained over about an hour.
- It examines how the contrast substance enters and travels via the urinary system.
- When compared to USG, it has a reduced false positive rate.
- It is frequently used for stone follow-up or anatomical evaluation following stone removal.
Voiding cystourethrography
- A urethral catheter is used to fill the bladder with contrast material, and fluoroscopic pictures are acquired while the contrast material is being filled and voided.
- It is the best imaging study for suspected vesicoureteral reflux (VUR).
Renography with diuretics
- Intravenously, a radionucleotide and diuretic are administered, and a series of pictures are obtained while the marker passes through the kidney and urinary system.
- It is best for distinguishing between obstructive and nonobstructive hydronephrosis.
- It helps determines the function of each kidney (i.e., how much of the “workload” is performed by each kidney).
Urography using magnetic resonance imaging
- It provides a viable alternative to conventional urinary tract imaging, particularly for individuals who are intolerant to ionizing radiation or contrast chemicals.
- It is a promising technique for imaging the urinary system that provides both anatomical and functional information.
- Usually, it is used in surgical planning.
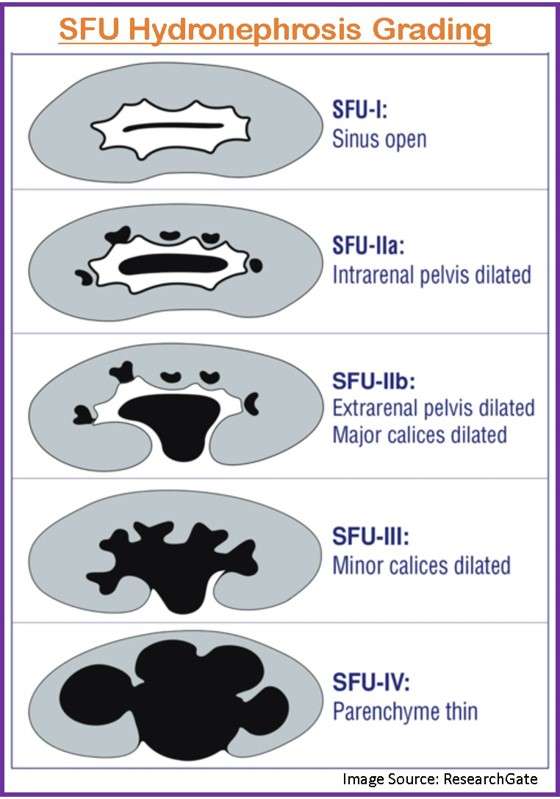
Grading of Hydronephrosis
The Society of Fetal Urology (SFU) developed a hydronephrosis grading system to measure the degree of hydronephrosis. This method is regarded to be the most widely used, and it was initially created to grade newborn and infant pelvicaliectasis:
- Grade 0 (Normal): There is no dilatation, and the calyceal walls are opposed to each other.
- Grade 1 (Mild): There is dilatation of the renal pelvis but not calyces (can also occur in the extrarenal pelvis)
- Grade 2 (Mild): There is no parenchymal atrophy or dilatation of the renal pelvis or calyces (pelvicalyceal pattern is retained)
- Grade 3 (Moderate): There is no parenchymal atrophy, but there is significant dilatation of the renal pelvis and calyces, blunting of fornices, flattening of papillae, and minor cortical thinning.
- Grade 4 (Severe): Gross dilatation of the renal pelvis and calyces, loss of borders between the renal pelvis and calyces, renal atrophy seen as cortical thinning
Management/Treatment of Hydronephrosis
- The objective of hydronephrosis therapy is to restore the free flow of urine from the kidney and to reduce the swelling and pressure that accumulates and impairs kidney function.
- Because the primary issue is the underlying condition, treatment is dependent on it.
- Treatment may not be necessary for pregnant women or their unborn children.
- In adults, the medical management is confined to pain management and infection treatment or prevention. The majority of illnesses need either minimally invasive or open surgical therapy.
- When a lower urinary tract obstruction at the bladder level is detected, a urinary catheter should be placed.
- Hydronephrosis and severe urinary blockage can harm the kidneys and cause kidney failure. Dialysis or a kidney transplant will be required for treatment in the case of kidney failure. However, with prompt treatment, most patients can recover from hydronephrosis.
Treatment for Infants
- The therapeutic strategy in newborns with prenatal hydronephrosis is determined by
- The persistence of postnatal hydronephrosis,
- Bilateral involvement, and
- The severity of hydronephrosis.
- All therapy options for neonatal hydronephrosis aim to identify all newborns with significant obstructive dilatation during serial follow-ups and conduct surgical correction before permanent deterioration and functional renal impairment occur
- If postnatal USG reveals chronic hydronephrosis, voiding cystourethrography (VCUG) is indicated.
- To detect probable Posterior Urethral Valves (PUVs) in male babies, the posterior urethra should be thoroughly examined.
- USG should be conducted once the child has returned to birth weight
- In babies with severe prenatal unilateral hydronephrosis
- Renal pelvic diameter > 15 mm in the third trimester
- After age 48 h and within the first 2 weeks of life.
- Antibiotic prophylaxis is begun as soon as feasible after delivery
- To rule out VUR or obstructive uropathy and
- To prevent UTIs.
Medical Management
- Mild-moderate hydronephrosis may resolve on its own.
- Antibiotic prophylaxis is advised to reduce the incidence of UTIs.
- Trimethoprim-sulfamethoxazole
- Nitrofurantoin
- Cephalosporins
- Fluoroquinolone
Surgical Management
Surgery is also necessary in some cases of extrinsic compression caused by pelvic, retroperitoneal, and aortic aneurysms, among other things.
Nephrostomy
- A nephrostomy is a procedure that uses a catheter or a nephrostomy tube (soft tube) to remove excess urine from the kidney.
- It is frequently the first step in the treatment of hydronephrosis.
Ureteral stent implantation
- A cystoscopy-guided ureteral stent implantation is a popular technique for a variety of intrinsic and extrinsic causes of ureteral hydronephrosis.
- When ureteral stent placement is contraindicated or cannot be done, interventional radiologists use fluoroscopy to guide percutaneous nephrostomy tube installation.
Shockwave lithotripsy
- To prevent future hydronephrosis and blockage, extracorporeal shockwave lithotripsy is used to treat renal stones in the renal pelvis.
Pyeloplasty
- Pyeloplasty is done to
- Remove the obstruction
- Improve urine flow
- Reduce the risk of kidney damage
- Reattach the ureter to the renal pelvis.
- It is often reserved for strictures that cause an obstruction as well as continuing symptoms such as discomfort, recurring infection, or kidney damage.
Others
Other ureteric stricture therapies that can be utilized with minor strictures but have a significantly lower likelihood of healing the disease include:
- Percutaneous endopyelotomy is a procedure that involves inserting a telescopic device via the flank, into the kidney, and correcting the stricture from inside.
- Trans-ureteric surgery includes inserting a tiny telescopic device through the urethra, bladder, and into the affected ureter without making any exterior incisions.
Complications
- Infection secondary to obstruction
- Electrolyte imbalance
- Hyperkalemia
- Metabolic acidosis
- Distal renal tubular acidosis
- Excessive free water diuresis
- Hypertension
- Renal insufficiency and renal failure
- Renal scarring
- Sepsis
Prevention
Because hydronephrosis is a condition caused by an underlying cause, prevention is dependent on avoiding the underlying cause.
- Individuals with kidney stones that induce ureteral blockage and hydronephrosis, for example, may try to reduce the likelihood of a recurring stone by staying hydrated.
- Patients with kidney stones should be informed about dietary adjustments to assist avoid the production of new stones.
- During pregnancy, an ultrasound might reveal a blockage in the baby’s urinary tract. As a result, the condition can be corrected with early surgery.
- It is critical to pay attention to general urination problems.
- Patients should be taught to seek the medical attention if they experience the first signs like
- Inability to void,
- Urinary infection (fever, burning, painful urination),
- Cloudy, rusty, or smoky urine,
- Flank pain.
Prognosis
- Chronic hydronephrosis produces ischemia damage, which leads to cortical and medullary atrophy and irreversible renal function loss.
- Hydronephrosis is reversible if the obstruction is removed as soon as possible.
- Prolonged hydronephrosis can cause irreparable kidney injury due to tubular atrophy and interstitial fibrosis.
- The overall prognosis of renal recovery following obstruction relief is determined by the duration and severity of the blockage.
Summary
- Hydronephrosis is a kidney condition characterized by increasing dilatation of the renal pelvis and atrophy of the renal parenchyma.
- It causes can be categorized into two types: intrinsic and extrinsic compression. Renal stones and cancer are two causes of intrinsic blockage. Pregnancy, peripelvic cysts, prostate abscesses, and other medical conditions can all cause extrinsic compression.
- It can be classified as, acute or chronic, unilateral or bilateral, and partial or complete.
- Common signs and symptoms of hydronephrosis include dysuria, urgency, hematuria, flank pain, azotemia, etc.
- It is usually diagnosed by urinalysis, blood test, and USG. CT is commonly regarded as the gold standard imaging modality for the identification of renal calculi and hydronephrosis.
- Treatment includes analgesics, antibiotics, and treating the underlying cause of hydronephrosis.
References
- Mevorach, R. A., Hulbert, W. C., & Rabinowitz, R. (2007). Hydronephrosis. Pediatric Clinical Advisor (pp. 283-284). Mosby.
- Mesrobian, HG. O., & Mirza, S. P. (2012, Aug). Hydronephrosis: a view from the inside. Pediatric Clinics of North America, 59(4), 839-851. DOI: 10.1016/j.pcl.2012.05.008
- Thotakura, R., & Anjum, F. (2022, Jan). Hydronephrosis And Hydroureter. StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK563217/
- Patel, K., & Batura, D. (2020, Jan 2). An overview of hydronephrosis in adults. British Journal of Hospital Medicine, 81(1), 1-8. DOI: 10.12968/hmed.2019.0274
- Alshoabi, S. A., Alhamodi, D. S., Alhammadi, M. A., & Alshamrani, A. F. (2021, Sep-Oct). Etiology of Hydronephrosis in adults and children: Ultrasonographic Assessment in 233 patients. Pakistan Journal of Medical Sciences, 37(5), 1326-1330. DOI: 10.12669/pjms.37.5.3951
- Onen, A. (2020, Aug 27). Grading of hydronephrosis: an ongoing challenge. Frontiers in pediatrics, 8, 458. https://doi.org/10.3389/fped.2020.00458
- Laquerre, J. (2020, Nov). Hydronephrosis: diagnosis, grading, and treatment. Radiologic Technology, 92(2), 135-151. https://pubmed.ncbi.nlm.nih.gov/33203770/
- Rasmussen, P. E., & Nielsen, F. R. (1988, Mar). Hydronephrosis during pregnancy: a literature survey. European Journal of Obstetrics & Gynecology and Reproductive Biology, 27(3), 249-259. DOI: 10.1016/0028-2243(88)90130-x
- Belarmino, J. M., & Kogan, B. A. (2006, Jan). Management of neonatal hydronephrosis. Early human development, 82(1), 9-14. https://doi.org/10.1016/j.earlhumdev.2005.11.004
- Ilgi Sr, M., Bayar, G., Abdullayev, E., Cakmak, S., Acinikli, H., Kirecci, S. L., & Horasanli, K. (2020, may). Rare Causes of Hydronephrosis in Adults and Diagnosis Algorithm: Analysis of 100 Cases During 15 Years. Cureus, 12(5), e8226. doi: 10.7759/cureus.8226
- Lusaya, D.G. (2022, Oct 3). Hydronephrosis and hydroureter. Medscape. Retrieved 2023, Jan 1 from https://emedicine.medscape.com/article/436259-overview
- Zeidel, M. L., & O’Neill, W. C. (2022, Aug 18). Clinical manifestations and diagnosis of urinary tract obstruction and hydronephrosis. UpToDate. Retrieved 2023, Jan 1 from https://www.medilib.ir/uptodate/show/7174