Introduction
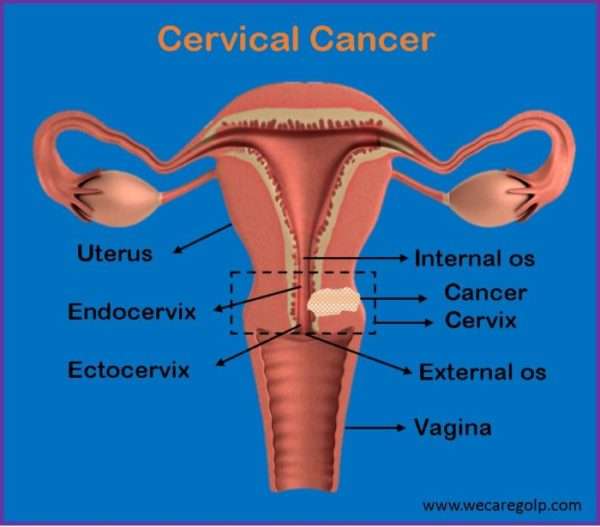
Cervical cancer is the type of cancer that develops in the cells of the woman’s cervix. The cervix, also known as the neck of the uterus, is a part of the female reproductive system that connects the uterus to the vagina. It locates in the lower, narrow end of the uterus. Before the irreversible stages of cancer appear in the cervix, the cells go through changes known as dysplasia, in which abnormal cell begins to appear in the cervical tissue. Over the course of time, the abnormal cells become cancer cells that start to grow and spread more deeply into the cervix and to surrounding areas.
Incidence
According to WHO:
- Cervical cancer is the fourth leading cancer in females worldwide after breast, colorectal, and lung cancer.
- About 90% of the new cases and deaths worldwide in 2020 due to cervical cancer occurred in low and middle-income countries.
- The incidence of cervical cancer is steadily declining in developed countries due to early detection through screening programs.
Types of Cervical Cancer
The cervix lies between the outer vagina and the inner uterus. The interior cavity of the cervix is called the cervical canal which can be divided into the endocervix and ectocervix. The two main types of cervical cancer based on anatomical location are:
Squamous cell carcinoma
- It is the most common type of cervical cancer (90%).
- Cancer develops from ectocervix.
- Ectocervix is the outer part of the cervix continuous to the vagina that is made up of squamous epithelial cells.
Adenocarcinoma
- It develops in the glandular cells of the endocervix.
- Endocervix is the inner part of the cervix that connects the vagina to the uterus.
- The endocervix is made up of columnar cells that secrete mucus.
Stages of Cervical Cancer
Staging classifies the extent of cancer in the body based on the location of cancer when it is first diagnosed. The following stages (I to IV) describe the severity of cervical cancer depending on the cancer extension in the body according to the most common staging system International Federation of Gynecology and Obstetrics (FIGO) 2018.
Stage I
Carcinoma is found in the cervix only.
- Stage IA: Micro invasive, identified only microscopically, with deepest invasion </= 5mm and largest extension </=7mm
- Stage IA1: The deepest point of tumor invasion is 3mm or less.
- Stage IA2: The deepest point of tumor invasion is more than 3 mm but less than 5mm.
- Stage IB: Clinical lesion confined to cervix or preclinical lesion greater than stage IA
- Stage IB1: The tumor is 2 cm or smaller and the deepest point of tumor invasion is more than 5 mm.
- Stage IB2: The tumor is larger than 2 cm but not larger than 4 cm.
- Stage IB3: The tumor is larger than 4 cm.
Stage II
Cervical cancer has spread to the upper two-thirds of the vagina or the tissue around the uterus, but not to pelvic wall & lower third
- Stage IIA: Cancer has spread from the cervix to the upper two-thirds of the vagina but has not spread to the tissue around the uterus.
- Stage IIA1: The tumor is 4 cm or smaller
- Stage IIA2: The tumor is larger than 4 cm.
- Stage IIB: Cancer has spread from the cervix to the tissue around the uterus.
Stage III
Cervical cancer has spread to the lower third of the vagina and/or to the pelvic wall and/or has caused kidney problems and /or involves lymph nodes.
- Stage IIIA: Cancer has spread to the lower third of the vagina but has not spread by the pelvic wall.
- Stage IIIB: Cancer has spread to the pelvic wall and/or the tumor has become large enough to block one or both ureters or has caused one or both kidneys to get bigger or stop working.
- Stage IIIC
- Stage IIIC1: Cancer has spread to lymph nodes in the pelvis.
- Stage IIIC2: Cancer has spread to the lymph nodes in the abdomen near the aorta.
Stage IV
Cancer has spread beyond the pelvis, has spread to the lining of the bladder or rectum, or has spread to other parts of the body.
- Stage IV is also called metastatic cancer.
- Stage IVA: Cancer has spread to nearby pelvic organs, such as the bladder or rectum.
- Stage IV B: Cancer has spread to other parts of the body, such as the liver, lungs, bones, or distant lymph nodes.
Causes of Cervical Cancer
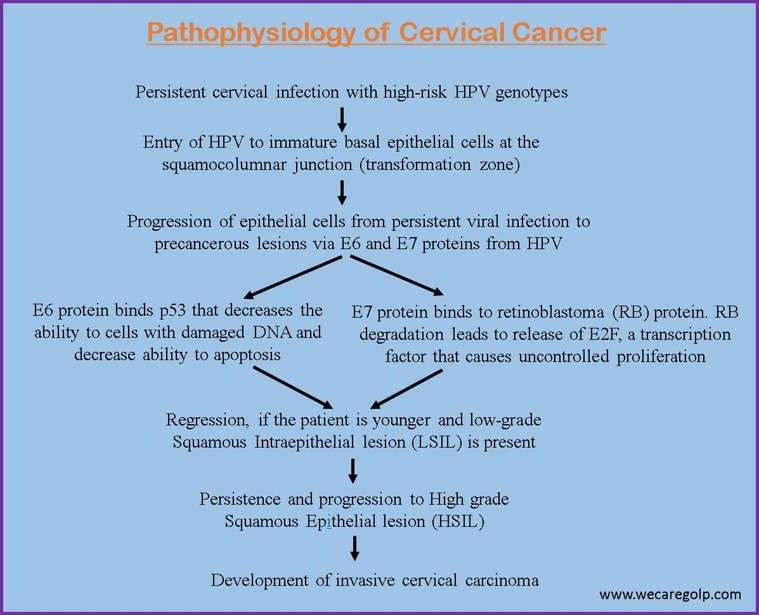
- The WHO 1996 declared HPV as the major cause of cancer of the cervix.
- The most common strain of HPV causing cervical cancer is HPV 16 strain followed by HPV 18 strain.
- HPV has two proteins known as E6 and E7, which turn off the tumor suppressor genes like p53 and Rb.
Risk Factors of Cervical Cancer
- Human Papilloma Virus (HPV) Infection
- Most commonly, HPV infection is due to the strains HPV-16, HPV-18, HPV-45, and HPV-31. Among the HPV family, HPV-16 and HPV-18 infection causes cervical cancer.
- When a high-risk HPV infection lasts for many years, it can lead to changes in the cervical cells that, if untreated, can become cancer.
- Weakened immune system
- This lowers the body’s ability to fight against infection and other diseases.
- Conditions that weaken the immune system are:
- HIV Infection
- Autoimmune diseases
- People under immunosuppression drugs
- Smoking
- Reproductive factors
- Becoming sexually active at an early age
- Multi-parity with poor birth spacing
- Long-term use of hormonal contraception and hormonal therapy (COCs)
- Multiple sex partners Women with a history of pre-invasive lesions
- Family history of cervical cancers
- Multiple sex partners
- Exposure to hormonal drug diethylstilbestrol (DES)
- Lack of regular cervical screening
- Low socio-economic status
Signs and Symptoms of Cervical Cancer
The early stages of cervical cancer are asymptomatic. However, some of the symptoms are:
- Vaginal bleeding after sex
- Dyspareunia (painful sexual intercourse)
- Vaginal bleeding between periods or menorrhagia (periods that are heavier or longer than normal)
- Vaginal discharge that is watery and has a strong odor or that contains blood
- Pelvic pain
The symptoms of advanced cervical cancer may be the following including the symptoms of early-stage cervical cancer.
- Dysuria (difficult or painful urination) or hematuria (blood in urine)
- Difficult or painful bowel movements
- Dull backache
- Swelling of the legs
- Abdominal pain
- Urinary retention
- Constipation
- Anemia
Pathophysiology of Cervical Cancer
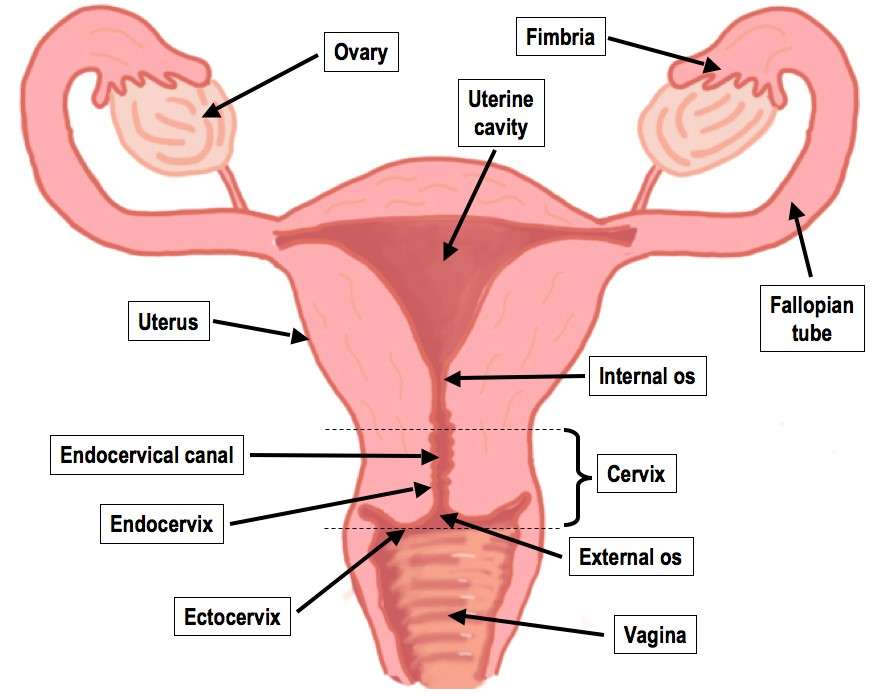
- The cervix consists of the internal os, endocervical canal, ectocervix, and external os.
- The place where the endocervical canal overlaps with the ectocervix is called the transformation zone (TZ).
- The transformation zone is the most common site for abnormal cells to grow in the cervix.
- The precursor to cervical cancer is cervical intraepithelial neoplasia (CIN).
- CIN, if untreated, later leads to the development of invasive cervical cancer.
Diagnosis
Bimanual pelvic examination
- Under this gynecological examination, a vaginal speculum is inserted into the vagina to visualize the cervix.
- A pap test is done at the same time.
Pap smear
- Pap smear is a test that is used to detect the presence of pre-cancerous or cancerous cells in the cervix. Under this examination, the inside and outside cells of the cervix area taken with the help of a smear sampling device.
Human Papilloma Virus (HPV) typing test
- This test examines the presence of strains of HPV like HPV 16 and HPV 18, also called high-risk HPV.
- However, HPV testing alone does not confirm the presence of cervical cancer.
Colposcopy
- Colposcopy is a diagnostic method in which a special instrument colposcope is used to check the cervix for abnormal areas. The colposcope magnifies the cells of the vagina and cervix.
Cervical biopsy
- Cervical biopsy is a procedure to remove a small amount of tissue for examination under a microscope.
- It is the definitive test to diagnose cervical cancer.
Treatment/Management
The treatment and management of cervical cancer depend on the stage of cancer, overall health status, fertility status, and patient preferences.
Surgery
Conization
- It is a surgical procedure in which a scalpel is used to remove cone-shaped tissue from the cervix and cervical canal.
- This method is usually preferred by people who wish to have children in the future.
Sentinel lymph node biopsy
- Sentinel lymph node biopsy removes the sentinel lymph node during surgery. The sentinel lymph node is the first lymph node to receive lymphatic drainage from the primary tumor.
Hysterectomy
It is the complete or partial removal of the uterus. Types of hysterectomy done to treat cervical cancer are:
- Total hysterectomy: It is the surgical removal of the uterus and cervix. Depending on the site of the incision and surgical procedures involved, it may be a total vaginal hysterectomy, total abdominal hysterectomy, or total laparoscopic hysterectomy.
- Radical hysterectomy: It is the surgical removal of the uterus, cervix, part of the vagina, and a wide area of ligaments and tissues around these organs. The ovaries, fallopian tubes, or nearby lymph nodes may also be removed.
- Modified Radical Hysterectomy: It is the surgical removal of the uterus, cervix, upper part of the vagina, and ligaments and tissues that closely surround these organs.
Radical Trachelectomy
- It is also known as radical cervicectomy.
- It is the surgical removal of the cervix, nearby tissues, and the upper part of the vagina. Lymph nodes may also be removed.
Bilateral pelvic exenteration
- It is the removal of the lower colon, rectum, and bladder.
- The cervix, vagina, ovaries, and nearby lymph nodes are also removed.
The complications of surgery may be acute or chronic. They are as listed below here:
Acute Complications
- Blood loss
- Fistula formation
- Pulmonary embolus
- Small bowel obstruction
Chronic Complications
- Bladder formation
- Lymphocyst formation
- Lymphedema
Radiation Therapy
- It is the use of high-energy x-rays or other radiation to kill cancer cells.
- Radiation therapy may be given alone, before surgery, or instead of surgery to shrink the tumor.
- The two main types of radiation therapy are external radiation therapy and internal radiation therapy.
Chemotherapy
- Chemotherapy uses drugs to stop the growth of cancer cells.
- It may be given before or after radiation therapy.
- Combination of drugs may be used to treat cervical cancer. Some of them are:
- Cisplatin
- Carboplatin
- Fluorouracil
- Paclitaxel
- Topotecan
- Docetaxel
- Ifosfamide
- Fluorouracil
- Irinotecan
- Mitomycin
Prognosis
The prognosis of cervical cancer depends on many factors.
- Stage of cancer (size of the tumor and whether cancer has spread beyond the cervix).
- Type of cervical cancer (Adenocarcinoma or squamous cell carcinoma)
- Pre-morbid disease conditions
- Recurrent or recently diagnosed cancer
The 5 -year relative survival rate represents the percentage of people with the same type and stage of cervical cancer who are alive 5 years after their cancer was diagnosed, compared with people in the overall population.
- The 5-year survival rate for cervical cancer diagnosed at an early stage is 92%.
- When it is diagnosed after it has spread to nearby tissues, organs, or regional lymph nodes, the 5-year survival rate is 58%.
- When it is diagnosed after it has spread to a distant part of the body, the 5-year survival rate is 18%.
- The 5-year survival rate for all people with cervical cancer is 66%.
Thus, early screening and treatment help to prevent and manage cervical cancer.
Screening for cervical cancer
- Human papilloma virus (HPV) test
- It checks cells for infection with high-risk types of Human Papilloma Virus that can cause cell changes on the cervix.
- Visual Inspection with Acetic Acid (VIA) test
- Under this screening, detection of acetowhite lesions on the cervix 1 minute after application of 3%-5% freshly prepared acetic acid is done.
- Pap smear test
- Pap smear test is obtaining a sample of a cervical cell.
- The specimen should be obtained two weeks after the first day of the last menstrual period.
- The purposes of a pap smear test are:
- To detect early cancer of the cervix.
- To determine estrogen activity related to menopause or endocrine abnormalities.
When and how often should cervical cancer screening be done?
| Age | Pap smear frequency |
| Age Less than 21 years old | None needed |
| Age 21-39 years | First screening should begin at the age of 21 years old. After the first screening, pap testing should be done every 3 years. |
| Age 30-65 years | Every 3 years or HPV every 5 years or a pap test and HPV test together every 5 years |
| Older than 65 years | No longer screening is needed, if the regular pap smear results are normal |
Contraindications to Cervical Cancer Screening
- HIV positive
- Weakened immune system
- Had a recent abnormal cervical screening test or biopsy result
- Have had cervical cancer
- Has been exposed to diethylstilbestrol (DES)
- Have had a total hysterectomy for reasons not related to cervical cancer or pre-cancer.
Complications
- Cystitis
- Proctitis
- Uterine perforation
- Vaginal stenosis
- Bone fracture
- Hormone deficiency
- Secondary malignancy
Prevention
The WHO has called for a global initiative for the elimination of cervical cancer as a public health problem by implementing a 90%-70%-90% triple pillar intervention strategy before the year 2030, which includes:
- 90% of girls fully vaccinated with two doses of HPV vaccine by the age of 15 years.
- 70% of women screened using a high-performance screening test at the age of 35 and 45 years.
- 90% of women detected with cervical lesions receive treatment and care.
Primary prevention
HPV vaccination
HPV vaccination was launched in 2006. American Cancer Society (ACS) recommends:
- HPV vaccination of children between the ages of 9 and 12.
- A two-dose schedule (0.5 ml at 0 and 6-12 months) is given. The second dose ought to tend 6-12 months once the primary dose. Children and young adults aged 13 through 26 who have not been vaccinated, or got their doses, should get vaccinated as soon as possible.
- The ACS does not advocate HPV vaccination for persons older than twenty-six years.
Health education on safe sexual practices
- The commonest reason for cervical cancer is HPV infection. So, exposure to HPV should be limited.
- HPV can be spread from one person to another during skin-to-skin contact with an infected area of the body. So, other than sexual contact may also cause cervical cancer.
- Use condoms during sex.
- Limit the number of sex partners.
- Avoid having sex with people who have had many other sex partners.
- Warnings on tobacco use and smoking
- Emphasis on the use of condoms
- Male circumcision
Secondary Prevention
- Screening tests like HPV test, Pap smear test
- Early identification and treatment
- Finding cervical pre-cancers
Tertiary Prevention
Treatment of invasive cancer at any stage includes:
- Surgery
- Radiotherapy
- Chemotherapy
- Palliative care
Summary
- Cervical cancer, the fourth leading cancer in females worldwide is the abnormal proliferation of cervical cells most commonly at the squamocolumnar junction.
- The FIGO classification is the most commonly used method for staging the cervical cancer.
- The most cause of cervical cancer is Human Papilloma Virus (HPV) infection by strain 16.
- Repeated and untreated HPV infections lead to the production of E6 and E7 decreasing the ability of tumor suppression eventually causing cervical cancer.
- Symptoms like unusual vaginal bleeding during sex, painful sexual intercourse, unusual vaginal discharge, and painful bowel movement may be seen in the later stages.
- Diagnosis of cervical cancer can be done by Pap smear test, HPV typing test, colposcopy, and cervical biopsy.
- Surgical procedures like conization, hysterectomy, and bilateral pelvic exenteration along with chemotherapy and radiation therapy can be done for the management of cervical cancer.
- The 5-year survival rate for cervical cancer diagnosed at an early stage is 92%. So, early diagnosis improves the survival rate.
- The most widely used screening method for cervical cancer is a Pap smear test in which the cervical cells are taken and examined for abnormal cells.
- HPV vaccination and early screening helps to prevent the cancer to develop into advanced stages.
References
- https://www.who.int/health-topics/cervical-cancer (Retrieved on 19 December, 2022)
- https://www.cancernet.com (Retrieved on 19 December, 2022)
- https://www.cdc.gov (Retrieved on 19 December 2022)
- https://www.americancancersociety.com (Retrieved on 19 December 2022)
- https://www.cancer.gov (Retrieved on 19 December, 2022)
- https://www.webmd.com (Retrieved on 19 December, 2022)
- World Cancer Research Fund International. https://www.wcrf.org/diet-activity-and-cancer/cancer-types/cervical-cancer/
- Fowler J R, Maani E V, Dunton C J, Jack B W. Cervical Cancer. NIH. November 2022