Introduction
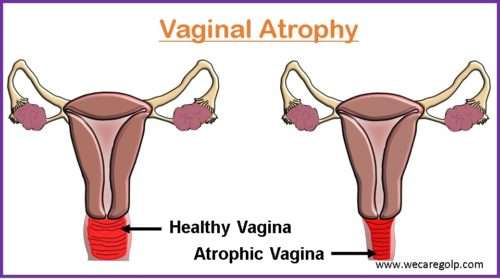
Vaginal atrophy is thinning and inflammation of the vaginal wall as a result of a decrease in estrogen level. Most commonly, it is a consequence of aging which occurs, particularly after menopause when estrogen deprivation accelerates the process of deterioration of urogenital tissues.
- Vaginal atrophy is a component of the genitourinary syndrome of menopause (GSM).
- The involution of the female genital tract is interrelated with the hypothalamic-hypophyseal-ovarian axis.
- The ovaries produce estrogen, which is essential for maintaining the health and lubricity of the vaginal tissues.
- With the increased life expectancy, most women will spend approximately, one-third of their life in the postmenopausal period, a hypoestrogenic state with the major universal change of aging i.e. vaginal atrophy.
Epidemiology
- It is estimated that approximately 64 million postmenopausal women in the United States (US), and as many as 32 million women may suffer from vulvar and vaginal atrophy symptoms including dyspareunia, vaginal dryness, and vaginal irritation.
- The American Association of Family Physicians stated that about 40% of postmenopausal women have the symptoms of vaginal atrophy.
- Studies show the prevalence of vaginal dryness in women from 27% to 55%. and dyspareunia ranging from 32% to 41%.
- The incidence of urinary tract infection (UTI) ranges from 4% to 15%.
- Approximately 40% of women taking oral hormone replacement have persistent vaginal dryness.
- Sternberg et. Al reported that 32% of women complaining of vaginal dryness had lost interest in sexual relations.
Causes of Vaginal Atrophy
- The vaginal epithelium is influenced by estrogen and is thick with abundant glycogen and is well regulated.
- The lactobacilli present in the vagina result in the production of lactic acid and other chemical substances including hydrogen peroxide (H2O2) which controls other micro-organisms in the vaginal ecosystem.
- The hormones and bacteria maintain the normal vaginal pH between 3.5 and 4.5 in healthy mature females, which protects them from vaginitis and UTIs.
- As estrogen levels decrease, the body naturally produces less lubricant in the cervix. Consequently, vaginal epithelium loses its rugae and becomes thin and pale or erythematous with fine petechial hemorrhages.
- The etiology of vaginal atrophy includes but is not limited to:
- Menopause
- Pelvic irradiation or chemotherapy
- Oophorectomy
- Use of anti-estrogen drugs like Tamoxifen, Danazol, Medroxyprogesterone, and Gonadotropin Releasing Hormone (GnRh) agonists
- Immediately after delivery or breastfeeding
- Postpartum loss of placental estrogen
- Immune disorders
- Idiopathic
Risk Factors of Vaginal Atrophy
- Smoking
- No sexual activity
- No vaginal births
Sign and Symptoms of Vaginal Atrophy
The lack of estrogen results in the loss of elasticity and secondary shortening and narrowing of the vagina with manifestations of the following signs and symptoms:
- Shrinkage of labia majora
- Decrease in introital opening
- Shrinkage of the vaginal canal
- Thinning of the vaginal epithelium
- Loss of rugae, pale, dry appearance
- Vaginal pH greater than 5
- Dryness of the vagina
- Burning and/ or itching of the vagina
- Spotting or bleeding
- Dyspareunia (painful sexual intercourse)
- Vulvar itching
The symptoms in the urinary system may be:
- Stress incontinence
- Increase in urinary frequency
- Dysuria (painful urination)
- Burning micturition
- Hematuria (blood in urine)
- Recurrent infections
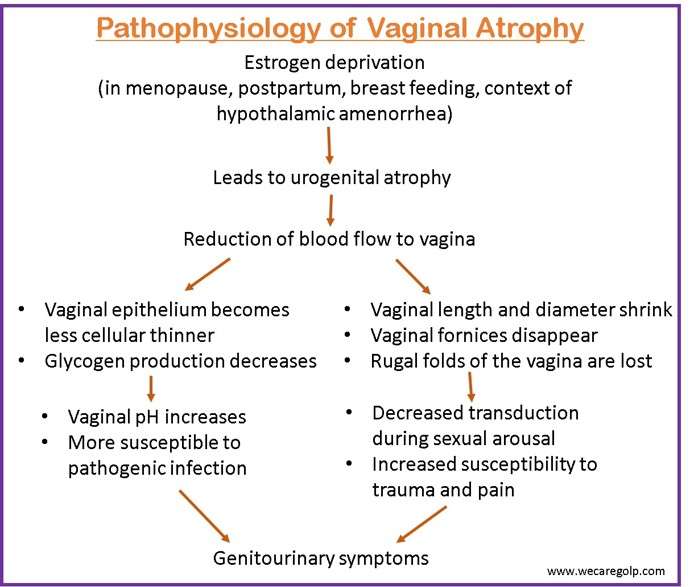
Pathophysiology of Vaginal Atrophy
- Estrogen increases the skin’s collagen content and maintains skin thickness. It also maintains skin and urogenital territory moisture by increasing acid mucopolysaccharides and hyaluronic acid and maintaining the epithelial barrier function.
- Estrogen receptors are found in the vagina, vulva, urethra, and trigone of the bladder, all of which experience atrophy when estrogen levels drop.
- The vaginal walls become thin and lose elasticity resulting in decreased vaginal secretion and susceptibility to trauma and pain.
- The estrogen-deficient vagina develops less pH level ranging from 5.5 to 6.8, which increases the likelihood of urinary tract infections.
- Thus, vaginal atrophy results in a combination of symptoms like vaginal dryness, dyspareunia, urinary frequency, repetitive urinary tract infections, or urinary incontinence.
- Dyspareunia leads to decreased interest in coitus. As the frequency of coitus decreases, vaginal lubrication declines further.
Diagnosis of Vaginal Atrophy
History taking
Take a detailed history of biodemographic data with emphasis on:
- History of frequency of urine, dysuria, nocturia, hematuria and incontinence
- Malodorous thick yellowish vaginal discharge
- Dyspareunia
- Vaginal soreness and itching
Physical examination
- A vaginal examination is done to assess the vaginal depth and general condition of the vagina.
Laboratory testing
- Level of circulating estrogen
- Cytology test
- Acid balance test (vaginal pH)
Management of Vaginal Atrophy
- As vaginal atrophy is a chronic condition, treatment should be continued for as long as symptoms persist and may need to be continued indefinitely.
- About 10% to 40% of women experience discomfort due to vulvar and vaginal atrophy, but it is estimated that only 25% seek medical help.
- The main goals of treatment for vaginal atrophy are to improve symptoms and to restore vaginal and vulvar anatomic changes.
- Manifestations of vaginal atrophy bring discomfort in the daily life of a woman, worsening the quality of life and vaginal health. Timely active detection of the pathological condition and providing adequately selected therapy can prevent the progress of disease and significantly improve the quality of life and sexuality of women.
Lifestyle Modification
Since the decline in estrogen levels is the primary etiology behind vulvovaginal atrophy, lifestyle factors that accelerate the decline of estrogen should be avoided. Some of them are:
Avoid smoking
Smoking results in the increased metabolization of estrogen and is associated with vaginal atrophy.
Regular vaginal coital activity
- Regular vaginal coital activity promotes protection from urogenital atrophy due to increased blood flow to pelvic organs.
- Studies reveal that masturbation increases genital blood flow in menopausal women and helps to maintain urogenital health
- Use of vaginal lubricants to decrease irritation during coital activity.
Medical Management
Treatment of vaginal atrophy depends on the severity of symptoms of the disease and the preferences and expectations of women.
Lubricants and moisturizers
- It is the first-line recommendation for the treatment of mild and moderate manifestations of vaginal atrophy.
- Vaginal lubricants should be used before intercourse.
- They provide short-term relief from vaginal dryness and discomfort during sexual intercourse.
- Vaginal moisturizers with a long-term effect are used regularly.
- Vaginal moisturizers enhance the moisturizing of the vaginal mucosa, reducing the pH.
- Lubricants and moisturizers are recommended for women for whom the use of vaginal estrogen preparation is unacceptable.
- When choosing lubricants and moisturizers, it is important to choose a product that is similar to vaginal secretions in terms of osmolality, pH, and composition.
Hormone therapy
- Hormone therapy is the second line of treatment after moisturizers and lubricants.
- It can be both systemic and local action.
- Vaginal creams are the most common type of local estrogen therapy.
- Systemic or topical application of pharmacological estrogen improves the index of maturation and thickness of vaginal mucosa, reduces the pH of the vagina, and increases vaginal maturation index.
- Estrogen-containing preparations for topical use are available in the form of a cream, tablets, and a vaginal estrogen-releasing ring which may contain estriol, conjugated estrogens, estradiol, or estrone.
- Vaginal ring is preferred to women for whom daily use of the drug is unacceptable.
- Vaginal ring is inserted for up to 90 days and can be independently inserted and removed by the patient.
- Vaginal ring is not recommended in women with prolapse of genitals.
- Systemic hormone replacement therapy includes all preparation containing estradiol or conjugated estrogens.
- Studies show that systemic hormone replacement therapy eliminates the symptoms of vaginal atrophy in 75% of cases, while local therapy does so in 80% to 90% of cases.
- Low doses of estrogen are preferred for use since the use of high doses of estrogen in menopausal age is associated with a high risk of hyperproliferative endometrial and adenocarcinoma.
- Local estrogen therapy may be low, intermediate, or high.
- The choice of form of administration of the drug is determined by the patient’s preference.
- Side effects to monitor:
- Excess estrogen levels in postmenopausal women are associated with an increased risk of heart disease, breast cancer, thromboembolic complication, and cerebrovascular disease.
Selective Estrogen Receptor Modulators (SERMs)
- It is used in women in whom estrogen preparations are contraindicated.
- SERMs interact with intracellular estrogen receptors in the target organs as agonists or antagonists of estrogens.
- E.g.: Ospemifene, Lasofoxifene, Bazedoxifene
Vaginal Dehydroepiandrosterone (DHEA)
- Dehydroepiandrosterone (DHEA) is a steroid prohormone.
- The vaginal metabolism of DHEA leads to the activation of the estrogen and androgen receptors in the vaginal wall.
Laser therapies
- It improves the vascularization of vaginal mucosa and thickens the vaginal epithelium
- Additionally, it stimulates the synthesis of new collagen and matrix basic substances in the connective tissue.
- Salvatire et al noted a significant improvement in the quality of life and sexual activity when laser therapies are used with vaginal atrophy.
Non-hormonal
- Use of non-hormonal water-soluble vaginal lubricants and moisturizers.
Complications of Vaginal Atrophy
- Vaginal infections
- An alteration in the pH balance may increase infections caused by yeast, bacteria, and other organisms.
- Additionally, this may increase the likelihood of UTIs.
- Genitourinary atrophy
- Dysuria
- Urinary urgency
Prevention of Vaginal Atrophy
Vaginal atrophy complicates the course of the postmenopausal period in more than half of women. Manifestations of vaginal atrophy bring discomfort i daily life, worsening the quality of life. Thus, timely active detection and providing adequate treatment prevent the progress of disease and significantly improve the quality of life and sexuality of women.
- Regular sexual activity if desired and acceptable, for all women and menopausal women.
- Regular sexual intercourse improves blood circulation to the vagina.
- Seminal fluid contains sexual steroids, prostaglandins, and essential fatty acids, which help to maintain vaginal tissue.
- Perineal pads, panty liners, and clothing that is too tight should be avoided.
- Water-soluble vaginal lubricant can also be used to moisten the tissues and prevent painful sexual intercourse.
Summary
- Vagina atrophy is thinning and inflammation of the vaginal wall as a result of the decrease in estrogen level.
- The most common cause of vaginal atrophy is aging while other causes may be oophorectomy, post-delivery, breastfeeding, pelvic irradiation, or chemotherapy.
- Studies reveal the prevalence of vaginal dryness in women from 27% to 55% and dyspareunia ranging from 32% to 41%.
- Estrogen produced by the ovaries helps to maintain skin thickness and increases skin collagen content.
- As estrogen level decreases, the body naturally produces less lubricant in the cervix, and blood flow to vagina is reduced, thus leading to manifestations of genitourinary symptoms.
- Vaginal atrophy leads to dryness of the vagina, vaginal itching, painful sexual intercourse, spotting or bleeding, and loss of rugae.
- Vaginal atrophy can be managed by avoiding smoking, regular coital activity, use of hormone therapy, selective estrogen receptor modalities, and laser therapies.
References
- Naumova, I. & Castelo-Branco, C. (2018, July 31). Current treatment options for postmenopausal vaginal atrophy International Journal of Women’s Health, 2018(10), 387-395. DOI:https://doi.org/10.2147/IJWH.S158913
- Lynch, C. (2009, Oct 26). Vaginal Estrogen Therapy for the Treatment of Atrophic Vaginitis. Journal of Women’s Health, 18(10), 1595-1606. http://doi.org/10.1089/jwh.2008.1281
- Kasikrishnaraja, P., Sainathan, S., Indira, M. (2017, July). Patterns and Correlates of Post-menopausal Symptoms in a Cohort of Gynecological Patients Attending Outpatient Department. International Journal of Scientific Study, 5(4), 40-46. https://docplayer.net/101058916-Patterns-and-correlates-of-post-menopausal-symptoms-in-a-cohort-of-gynecological-patients-attending-outpatient-department.html
- Lethaby, A., Ayeleke, R.O., Roberts, H., and Cochrane Gynaecology and Fertility Group. (2016, Aug 31). Local estrogen for vaginal atrophy in postmenopausal women. Cochrane Database Systc Rev, CD001500. doi: 10.1002/14651858.CD001500.pub3
- Johnston, S.L. & Farell, S.A. (2004, May). The detection and management of vaginal atrophy. J Obstet Gynaecol Can, 26(5), 503-508. https://www.jogc.com/article/S1701-2163(16)30662-4/pdf
- Leiblum, S., Bachmann, G., Kemmann, E., Colburn, D., Swartzman, L. (1983, April 22). Vaginal Atrophy in the Postmenopausal Woman: The Importance of Sexual Activity and Hormones. JAMA, 249 (16), 2195-2198. doi:10.1001/jama.1983.03330400041022
- Nelson, A. (2022, Jan 16). What’s Vaginal Atrophy. WebMd. Retrieved 2022, Dec 23 from https://www.webmd.com/menopause/vaginal-atrophy
- Women’s Healthcare of Princeton. (n.d.). 5 Signs of Vaginal Atrophy. Retrieved 2022, Dec 23 from https://www.princetongyn.com/blog/5-signs-of-vaginal-atrophy
- Healthline. (2017, June 22). Postmenopausal Atrophic Vaginitis. Retrieved 2022, Dec 23 from https://www.healthline.com/health/atrophic-vaginitis