Introduction
Breast cancer is the most common cancer in females worldwide that starts in the cells of the breast. It is found mostly in women, but 1% of breast cancers are also found in the male.
- The breast is composed of three main structures: skin, parenchyma, and stroma.
- The parenchyma is composed of 15 to 20 sections called lobes. Each lobe has many smaller structures called lobules and each lobe is drained by a lactiferous duct.
- The lactiferous ducts converge towards the nipple to open it. Breast cancer arises from the lining of the ducts (85%) or lobules (15%) in the glandular tissues of the breast.
- Initially, the cancerous growth is confined to the ducts or lobules (in situ) and later spreads to the surrounding tissue (invasive breast cancer).
- Breast cancer can spread outside the breast (metastasis) through blood vessels, lymph vessels, or both.
Epidemiology
- Globally, breast cancer is the most common cancer diagnosed in women and is the leading cause of death from cancer among women, with approximately 1.3 million new cases and an estimated 458,000 deaths reported in 2008.
- Breast cancer affects over 1.5 million women annually or 25% of all cancer patients.
- In America, it is estimated that 30% of all new cancer cases among women are breast cancer in 2017.
Anatomy of the Breast
- Breast is derived from the Latin word meaning mammary gland.
- Breast is a modified sweat gland.
- It is located in the superficial fascia of the pectoral region.
- Vertically, it is located from the 2nd to 6th ribs.
- Horizontally, it is located from the lateral border of the sternum to the mid-axillary line.
- Breast is anatomically divided into 4 quadrants:
- Upper inner
- Upper outer
- Lower outer
- Lower inner
- The upper lateral quadrant has a lateral extension known as the axillary tail of Spence.
- Most common site of cancer is the upper outer quadrant.
- Breast can be divided into 3 structures:
- Skin with nipple and areola
- Parenchyma
- Stroma
- The parenchyma comprises 15 to 20 lobes.
- Each lobe is a cluster of alveoli, drained by a lactiferous duct.
- The lactiferous ducts converge towards the nipple and open to it.
- Stroma is partly fibrous and partly fatty. It is the gland’s supporting structure.
- The specialized lymphatic channels collect under the nipple and areola and form Sappey’s plexus.
- About 75% of lymphatic drainage is to the axillary lymph node known as the Sentinel lymph node.
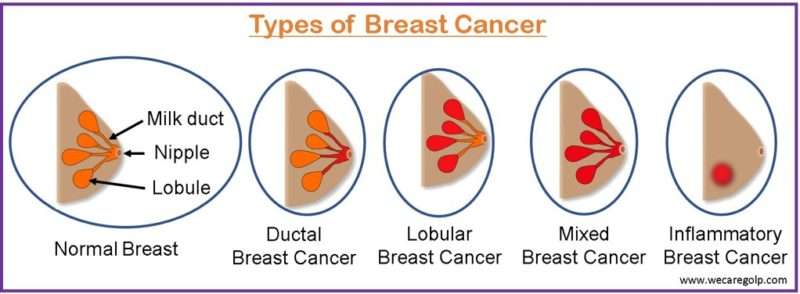
Types of Breast Cancer
Based on Histological Subtypes
Invasive
- Cancerous
- Malignant
- Metastasis may occur.
Non-invasive
- Pre-cancerous
- Cell is limited to the basement membrane.
- Eventually develops into invasive breast cancer.
Anatomical Classification
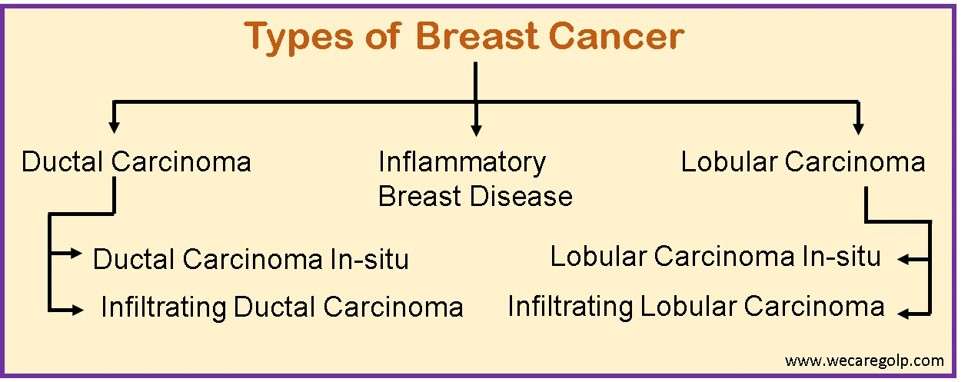
Ductal carcinoma
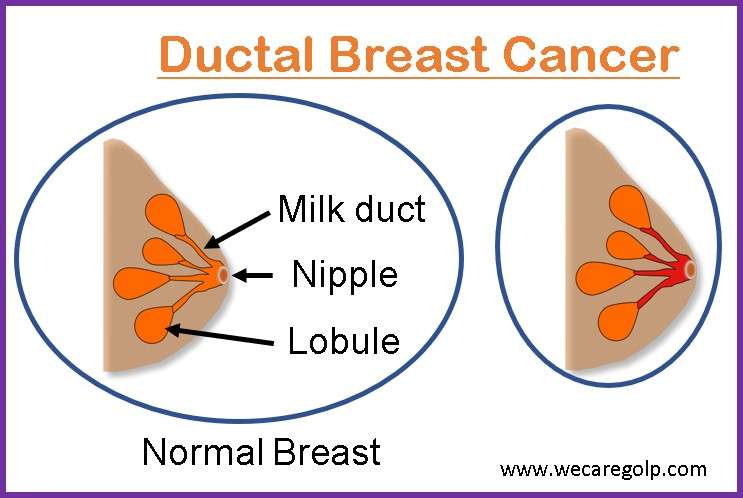
- Cancer in the inner lining of milk ducts.
- May be ductal carcinoma in situ or invasive ductal carcinoma.
- Ductal carcinoma in situ is the most common type of breast cancer.
Ductal carcinoma in situ
- Non-invasive
- Contained within the milk ducts
- ‘In situ’ means ‘in original place’
- May become invasive
Invasive ductal carcinoma
- Also known as infiltrating ductal carcinoma.
- Cancer spreads from a milk duct, where it originates, into nearby tissue and lymph nodes.
- According to the American Cancer Society, about 8 in 10 invasive breast cancers are invasive ductal carcinoma.
Lobular carcinoma
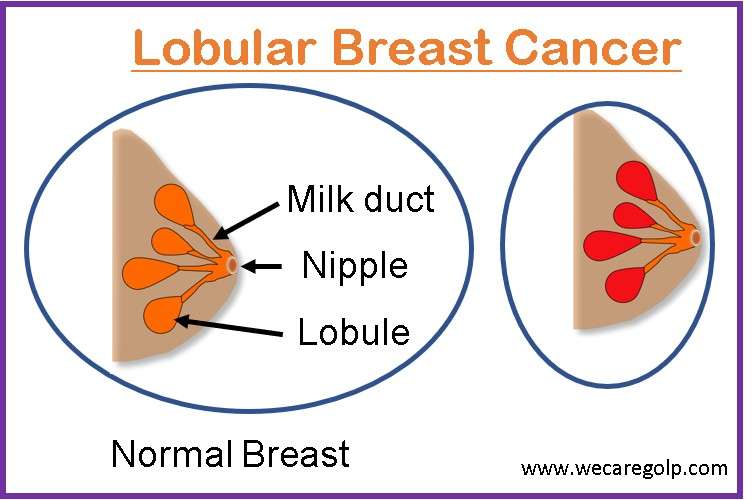
- Cancer in the lobules-milk-producing glands
- May be lobular carcinoma in situ or invasive lobular carcinoma.
Lobular carcinoma in-situ
- It starts in the lobules of the breast and typically does not spread through the wall of the lobules to the surrounding breast tissue or other parts of the body.
Invasive lobular carcinoma
- It starts in the lobules of the breast and may spread to other parts of the body.
Inflammatory Breast Cancer (IBC)
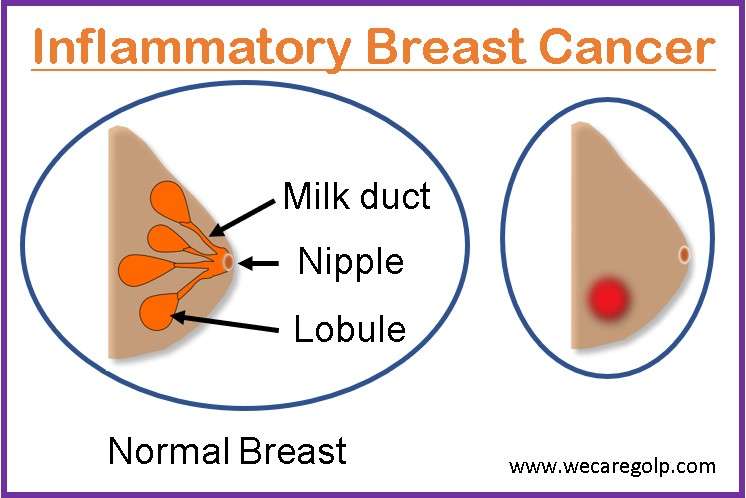
- Least common cancer (1% to 3% of all breast cancers)
- Invasive breast cancer
- No lump or tumor
- Mistaken for infection in its early stage.
- Skin changes:
- Red skin appearance
- Swollen, Warm skin
- Orange peel-like skin
- Inverted nipple
Triple-negative Breast Cancer
- A diagnosis of triple-negative breast cancer means the following three most common types of receptors are not present in cancer.
- Estrogen receptor (ER)
- Progesterone Receptor (PR)
- Human epidermal growth factor receptor 2 (HER2)
- About 10 to 20 % of the diagnosed breast cancer is triple negative.
- It is a high-risk breast cancer that lacks the benefit of specific therapy that targets these proteins.
Genes Related to Breast Cancer
BRCA 1 and 2
- Breast cancer-associated genes 1 and 2 (BRCA1/2) are the most common anti-oncogenes for breast cancer risk.
- BRCA 1 and 2 are located on chromosomes 17q21 and 13q12, respectively.
- Both genes encode tumor suppressor proteins.
- Deficiency of BRCA 1 leads to dysregulation of cell cycle checkpoint, abnormal centromere duplication, genetic instability, and eventually apoptosis.
- BRCA 2 protein regulates recombinational repair in DNA double-strand breaks by interacting with RAD 51 and DMC1.
- The risk increases in case of mutation of either BRCA1 or BRCA2 genes.
HER2
- Human epidermal growth factor receptor 2 (HER2) also known as c-erbB-2 is an important oncogene in breast cancer.
- It is an epidermal growth factor receptor (EGFR).
Cell surface glycoprotein
Causes of Breast Cancer
- Previous history of it
- Significant family history
- History of breast cancer from both maternal and paternal relatives is important.
- BRCA 1 and BRCA2 are abnormal genes that when inherited may increase the lifetime risk between 40 to 88%.
- Genetic cause
- Hormonal causes
- Lifestyle and dietary cause
- Sedentary lifestyle
- High dietary intake of fat
- Obesity
- Use of alcohol
- Environmental cause
- Exposure to UV-rays
Risk Factors of Breast Cancer
The risk increases with age. Estradiol stimulates the mitosis of breast epithelial cells. Early menarche and late menopause increase the risk by extending the relative exposure of the breast to a high concentration of estradiol.
Aging
- The incidence increases with increased age.
- In 2016, approximately 99.3% and 71.2% of all breast cancer-associated deaths in America were reported in women over the age of 40 and 60, respectively.
Early menarche
- The later the age of menarche, the lower the risk of breast cancer.
- For each 1-year delay in menarche, the risk decreases by around 5%.
Childbearing
- Compared with nulliparous women, women who have had at least one full-term pregnancy have on average around a 25% reduction in the risk of breast cancer.
- Increased protection against breast cancer is seen with the increasing number of full-term pregnancies.
Breastfeeding
- The US Cancer and Steroid Hormone Study showed that women who had breastfed for a total of 25 months or more had a 33% lower risk than those who had never breastfed.
Menopause
- Women who go through menopause later in life are more likely to develop breast cancer than those who stop having periods earlier.
- The risk increases by about 3% for each year older at menopause.
Endogenous hormones
- Postmenopausal women with high serum estradiol concentration have a risk of around twice that of women with the lower concentration of this hormone.
Oral contraceptives
- Oral contraceptives suppress the production of estradiol and progesterone, but the endogenous hormones are effectively replaced by the exogenous hormones.
- The risk is increased by around 25% in current users of combined oral contraceptives.
- The later the use of oral contraceptives, the larger the number of resulting excess cases.
Hormonal therapy for menopause
- Current users of hormonal therapy for menopause are at higher risk than women who have never used this preparation.
Use of exogenous hormones
- Studies from the 1940s to 1960s reveal a 30 % increase in the subsequent risk in women who were treated with diethylstilbestrol.
- Use of antifertility drugs like clomiphene citrate, human menopausal gonadotropin, and gonadotropin-releasing hormone increases the risk of breast cancer.
Diet
- The risk increases with the intake of a high-fat diet.
Physical Activity
- A lower risk of breast cancer is linked to moderate physical activity.
Family history and genetics
- Studies on the familial risk of breast cancer have revealed twofold relative risks for first-degree relatives (mothers, sisters, daughters) of the affected patient.
- With affected second-degree relatives (grandmothers, aunts, granddaughters), there is a lesser increase in risk.
Sign and Symptoms of Breast Cancer
- A lump or thickening in the breast that feels different from the surrounding tissue
- Alteration in shape, size, or appearance of the breast
- Fixed, firm mass with irregular borders
- Skin sores
- Dimpling of skin over the breast
- Inverted nipple
- Peeling, scaling, crusting, or flaking of the pigmented area of skin surrounding the nipple or breast skin.
- Redness or pitting of the skin over the skin
- Peau d’ orange (a pitted or dimpled appearance of the skin) due to the plugging of dermal lymphatics
- Nipple retraction
- Abnormal nipple discharge: discharge with blood
- Pain in any area of the breast
- In case of metastasis, the patient may present with the following features:
- Dyspnea due to metastasis to the lungs
- Bone pain and symptoms of hypercalcemia in bone metastasis
- Abdominal distention and jaundice in case of liver and peritoneal metastasis
- Altered cognitive function and local neurological signs of brain metastasis
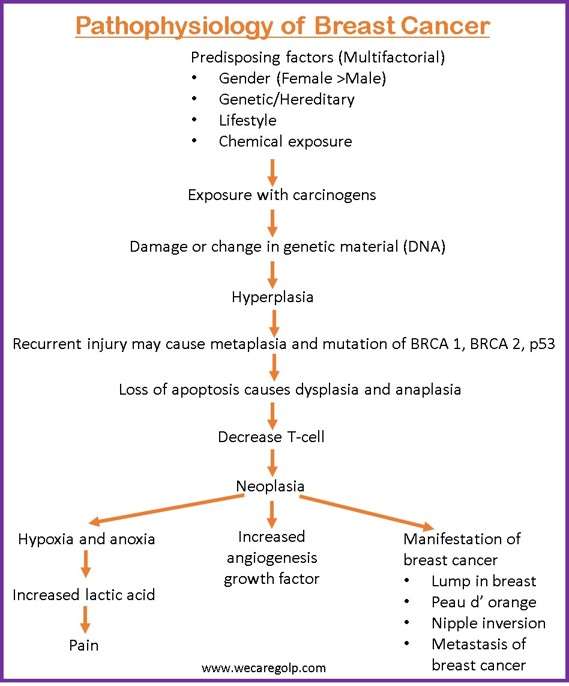
Pathophysiology of Breast Cancer
- Breast cancer can result from genetic mutations and DNA damage.
- The inheritance of defects in the DNA and genes like BRCA1, BRCA2, and P53 and those with a family history of breast cancer are at risk of developing breast cancer.
- The immune system fails to reverse the effects of mutant genes.
- Breast cancer invades locally and spreads through the regional lymph nodes, bloodstreams, or both.
- The lungs, liver, bone, brain, and skin are the most common organs that metastatic breast cancer can affect.
Screening
The American Cancer Society and the National Cancer Institute recommend annual screening mammography for women older than 40 years who have a standard risk of breast cancer. In women from high-risk families, especially those with BRCA 1 or BRCA 2 mutations, screening should start at 25 years of age, or 5 years earlier than the earliest age at which breast cancer was diagnosed in a family member.
Early detection of breast cancer is the cornerstone of breast cancer prevention. Early diagnosis of the disease can lead to a good prognosis and a high survival rate.
Screening of breast cancer is done by:
History and Physical Examination
- Complete medical history followed by clinical breast examination (CBE) procedure.
- For women aged between 20 to 39 years, CBE every 1 to 3 years is recommended.
- Breast self-examination should be done once every month, usually the week after the menstrual bleeding period stops.
- Women should be made familiar with their breasts and promptly report any changes to their healthcare provider.
- Symptoms or positive findings on physical examination include a palpable mass or lump, asymmetric thickening/ modularity, nipple discharge in the absence of a palpable mass, skin changes like peau d orange, erythema, nipple extraction, and scaling/ eczema.
Risk Assessment
A thorough risk assessment for breast cancer should be done for the women
- Who have undergone previous therapeutic thoracic irradiation or mantle irradiation.
- Aged 35 years or older.
- With a lifetime risk for breast cancer greater than 20% based on family history.
- With strong family history or genetic predisposition.
- With lobular carcinoma in situ or atypical hyperplasia.
- With a prior history of breast cancer.
Mammography
- Mammography is a screening method that uses low-energy X-rays to obtain high-resolution images of the breast.
- A mammography takes 2 radiographic images of each breast craniocaudal (taken from the top of the breast) and mediolateral oblique approach (taken from the other side).
MRI
- Magnetic Resonance Imaging (MRI) is more sensitive than mammography in high-risk women.
- In comparison to mammography, MRI is unaffected by breast density.
- MRI can detect occult primary breast cancer, axillary node metastasis, residual tumors after neoadjuvant chemotherapy, or other small tumors.
Treatment/Management of Breast Cancer
Combination of chemotherapy, radiation therapy or endocrine therapy may be used after surgery to prevent relapse.
Surgery
Breast-conserving surgery
- It is also known as lumpectomy or wide local excision or partial mastectomy.
- It is the surgical removal of only a tumor from the breast.
- It involves the removal of the tumor along with a margin of tissue conserving the cosmetic appearance of the breast.
- It is the most commonly used surgery.
- Most tumors are locally invasive.
- Large tumors can be reduced in size by neoadjuvant chemotherapy prior to conservative surgery.
Total mastectomy
- It is the surgical removal of the whole breast, including the nipple, areola, and most of the overlying skin.
- It is also known as simple mastectomy.
Modified radical mastectomy
- It is the surgical removal of the entire breast and the axillary lymph nodes including the fascia over the pectoralis muscles, but the pectoralis muscles are preserved.
- Indications are:
- Multicentric invasive carcinoma
- Inflammatory carcinoma,
- Extensive intraductal carcinoma
Axillary lymph node dissection
- It is the removal of lymph nodes draining the breast tissue for lymph node metastasis.
- Sentinel nodes are the first node or first group of nodes that drain from the breast to the axilla.
- Sentinel lymph node mapping is a procedure in which a radioactive substance or a blue dye is injected into the area around the tumor. Later, the lower ipsilateral axilla is explored through a small incision and the lymph node that has taken up the dye or radioactive substance is excised.
Radiation Therapy
- The breast can be irradiated entirely or in part in this therapy.
- Adjuvant radiation therapy is applied after breast-conserving surgery or mastectomy to prevent a recurrence.
- Palliative radiation therapy for metastatic disease is also used.
Chemotherapy
- Chemotherapy is a type of treatment to kill cancer cells or prevent them to grow and divide.
- Medical treatment given before surgery is neoadjuvant therapy.
- Medical treatment given after surgery is known as adjuvant therapy.
- Cytotoxic drugs, like cyclophosphamide, methotrexate, and doxorubicin can be given either pre-surgery as a neoadjuvant to shrink the tumor or post-surgery as an adjuvant to prevent relapse.
- Use of a combination of drugs is a more beneficial than single drugs.
Hormonal Therapy
- Breast cancer is hormone-sensitive cancer.
- ER-positive breast cancer will respond to a reduction of circulating estrogens.
- It is mainly used as adjuvant therapy for early-stage hormone-sensitive breast cancer or as first-line therapy for metastatic hormone-sensitive breast cancer.
- Common types:
- Antiestrogens e.g., Tamoxifen
- Aromatase Inhibitors e.g., Aromatase
Targeted Therapy
- It is the use of medicines that are directed at (target) proteins in the breast cancer cells.
- Types of targeted therapy are:
- Targeted therapy for HER2-positive breast cancer
- Targeted therapy for hormone receptor-positive breast cancer
- Targeted therapy for women with BRCA gene mutations
- Targeted therapy for triple-negative breast cancer
- Drugs used: trastuzumab, Pertuzumab, Margetuximab
Prognosis
- The 5- year survival rate tells what percentage of people live at least five years after the cancer is found.
- In the United States, women with non-metastatic invasive breast cancer have a 90% 5-year survival rate.
- 84% of women with non-metastatic invasive breast cancer survive for 10 years on average.
- If the breast cancer is located only in the breast, the 5-year survival rate of women with breast cancer is 99%.
- The 5-year survival rate is 86% if cancer has spread to the regional lymph nodes.
- If cancer has spread to a distant part of the body, the survival rate is 29%.
Complication of Breast Cancer
- Infection
- Hematoma
- Lymphedema
- Neuropathy
- Infertility
- Osteoporosis
- Bone pain
- Spinal compression
- Hypercalcemia
- Shortness of breath
Prevention of Breast Cancer
A favorable prognosis and a high rate of survival can result from the early diagnosis of the disease. In North America, there is 5- year survival rate of breast cancer.
Lifestyle modifications
- Prolonged breastfeeding
- Regular physical activity
- Early screening
- Weight control
- Avoidance of harmful use of alcohol
- Avoidance of exposure to tobacco smoke
- Avoidance of prolonged use of hormones
- Avoidance of excessive radiation exposure
Chemoprevention
- According to Sporn, ‘Chemotherapy is the use of pharmacologic or natural agents that inhibit the development of invasive breast cancer either by blocking the DNA damage that initiates carcinogenesis or by arresting or reversing the progression of pre-malignant cells in which such damage has already occurred.’
- More than 70% of breast cancer are estrogen-receptor positive breast cancer.
- Major classes of anti-estrogen drugs are:
- Selective estrogen receptor modulators (SERMs) and aromatase Inhibitors (AIs)SERMs are compounds that act either agonists or antagonists of estrogen receptors, e.g., Tamoxifen, Raloxifene, etc.
- Aromatase Inhibitors (AIs) reduce the plasma levels of estrogen by inhibiting aromatase, an enzyme that catalyzes the biosynthesis of estrogen from androgen, e.g., Exemestane, Anastrozole, Letrozole.
Biological Prevention
- It is also known as monoclonal antibodies for breast cancer.
- The main target of monoclonal antibodies is HER2
- Some examples are Trastuzumab, Pertuzumab.
Summary
- Breast cancer is the most common type of cancer in females in which abnormal and uncontrollable proliferation of tissues occurs in the breast.
- It can spread outside the breast through blood vessels and lymph vessels.
- It may be ductal carcinoma (85%) or lobular carcinoma (15%).
- Previous history of breast cancer, significant family history, and mutation in BRCA1 and BRCA2 genes are the common causes of breast cancer.
- The risk factors are aging, early menarche, late menopause, and contraceptives.
- Abnormal change in shape, size, or appearance of the breast, dimpling of the skin over the breast, nipple retraction, etc. are the signs evident.
- Early screening and diagnosis are the cornerstones of breast cancer prevention.
- Treatment may be a combination of surgery, chemotherapy, radiotherapy, hormonal therapy, and targeted therapy.
References
- Waks, A, G., Winer. E.P. (2019, Jan 22). Breast Cancer Treatment: A review. JAMA, 321(3): 288-300. DOI: 10.1001/jama.2018.19323
- Sun, Y. S., Zhao, Z., Yang, ZN., Xu, F., Lu, HJ., Zhu, ZY., Shi, W., Jiang, J., Yao, PP., Zhu HP. (2017, Nov 1). Risk Factors and Preventions of Breast Cancer. Int J Biol Sci, 13 (11),1387-1397. Doi: 10.7150/ijbs.21635
- Bosch, A., Eroles, P., Zaragoza, R., Vina, J. R. & Lluch, A. (2010, May). Triple -negative breast cancer: Molecular features, pathogenesis, treatment and current lines of research. Cancer Treatment Reviews, 36(3), 206-215. DOI: 10.1016/j.ctrv.2009.12.002
- Key, T.J., Verkasalo, P.K., Banks, E. (2001, Mar). Epidemiology of breast cancer. The Lancet Oncology, 2(3), 133-140. DOI: 10.1016/S1470-2045(00)00254-0
- American Cancer Society. (n.d.). About Breast Cancer. https://www.cancer.org/cancer/breast-cancer/about.html