Introduction
Mammography is soft tissue roentgenography (use of X-ray) to image the breast to detect breast cancer pathology and cancer. In mammography, low-dose X-rays are used which can show abnormal areas or tissues on the breast. It helps to detect cancer before the clinical manifestations of breast cancer occur.
- A mammogram is an X-ray picture of the breast obtained by mammography.
- A traditional mammogram creates 2D images of the breast.
- A newer, 3D image of the breast can also be created by a 3D mammogram known as breast tomosynthesis.
- Mammography is performed by a radiologist and is 85% to 90% effective.
Epidemiology
- The breast cancer risk death rates decreased by 42% from 1989 to 2019, because of both improvements in treatments and earlier detection.
- According to the National Health Interview Survey Reports 2021, about 70% of women aged 45 to 74 years have had a mammogram within the past 2 years.
- According to the U.S. Preventive Services Task Force (USPSTF), the number of breast cancer deaths decreased by screening and screening 10,000 women aged 60-69 years will result in 21 fewer deaths from breast cancer, 8 fewer deaths in 10,000 women 50-59 years, and 3 fewer deaths in 10,000 women 40-49 years.
Recommendations for Mammography
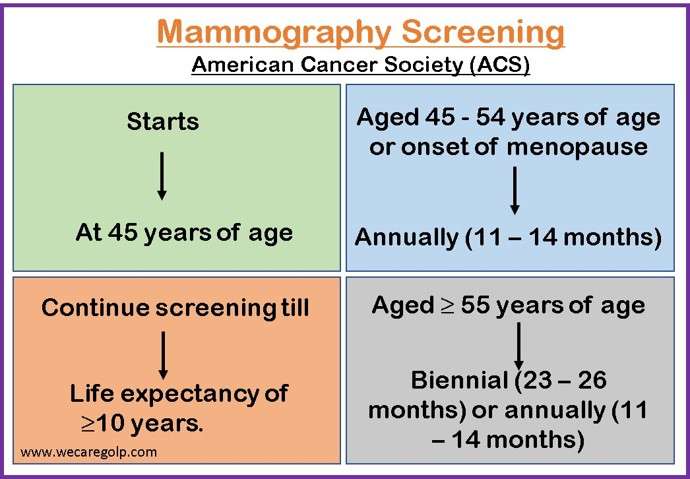
The American Cancer Society (ACS) recommends:
- Regular screening mammography starting at 45 years of age.
- Women aged 45-54 years of age should be screened annually.
- Women aged ≥55 years should transition to biennial screening or can continue screening annually.
- Women should continue screening mammography if their overall health is good and they have a life expectancy of ≥10 years.
- A baseline mammogram should be done at the onset of menopause.
Indications of Mammography
- Breast pain
- Swelling
- Nipple discharge
- Nipple retraction
- Calcification
- Benign or malignant tumor
- Lymph node enlargement
Contraindications of Mammography
- Breast implant
- Severe nipple discharge
- Large palpable mass
- Inflammation
- Women within reproductive age 15 to 40 (benefit over risk).
Risks of Mammography
- As mammography uses X-Rays to produce images of the breast, patients are exposed to a small amount of ionizing radiation, the risk-benefit ratio should be considered prior to mammography.
Types of Mammography
Based on the purpose of mammography, it can be classified as:
Screening
- Screening is done on a healthy population.
- It is a routine procedure done to detect the signs of breast cancer or abnormal tissue before the symptoms are present.
- Usually, it is performed on asymptomatic women with no signs of breast cancer.
Diagnostic
- It is performed when the patient has additional abnormal mammographic study findings or symptoms of breast cancer like
- Changes in breast shape, size, color
- Nipple discharge
- Abnormal mass on breast
- Nipple inversion
- Skin retraction or dimpling
- Peau d’orange (orange skin)
- Breast pain
- Diagnostic mammography is a part of the ‘triple test’, which includes a clinical examination and a needle biopsy of any pathological findings.
Mechanism of Mammography
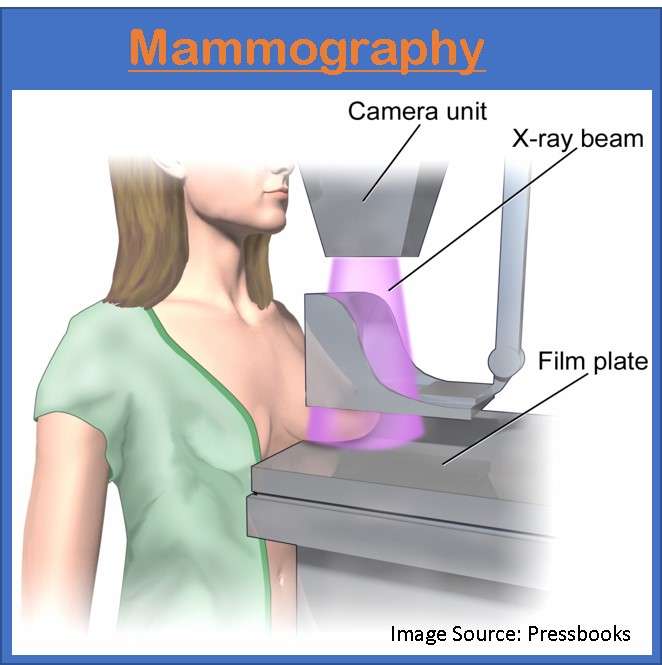
- Mammography uses an X-ray machine that produces lower doses of X-rays to look at the breast tissues.
- Breast is placed on a support plate attached to the X-ray machine.
- Breast is squeezed with a parallel plate called a paddle for 5 to 10 seconds.
- Compression holds the breast in place and minimizes blurring of the X-Ray image that can be caused by the movement of the patient.
- It evens out the shape of the breast so that x-rays can travel a shorter path to reach a detector. This allows for a lower radiation dose.
- It allows all the tissues to be visualized in a single plane.
- The X-rays pass through the breast to a detector located on the opposite side.
- Then, the detector transmits electronic signals to a computer to form a digital image.
- These images are called mammograms.
- The upper aspect of the image represents the outer portion of the breast.
- The lower aspect of the image represents the inner portion of the breast.
- The name of imaging comes from the location and the direction of X-ray beams.
Standard views on Mammography
Four standard views performed in every mammography with two views (left and right) of each breast: Craniocaudal (CC) view and Medial Lateral Oblique (MLO) view.
CC view
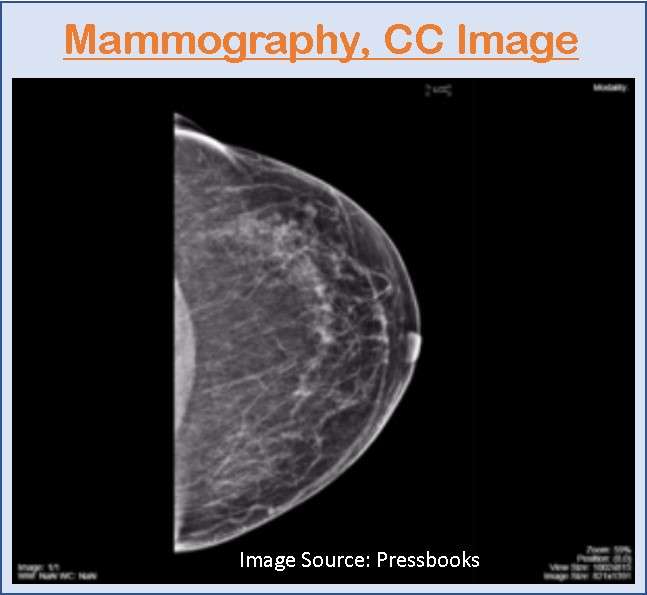
- CC view means the X-ray extends from the cranial or the superior aspect of the breast and extends through the breast to the patient’s feet.
- In CC View, the breast is placed on compression and the X-ray beam extends from above the breast through the breast to hit the image receptor below.
MLO view
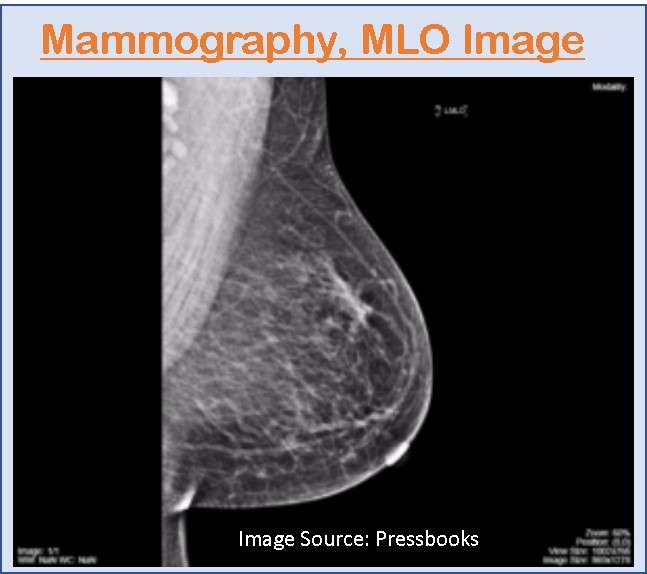
- MLO view is the direction that the X-Ray beam travels when the imaging is acquired.
- In MLO view, the breast is placed in compression at a 45˚ angle and the X-Ray beam travels from the medial aspect of the breast through to the lateral aspect.
Procedure of Mammography
During mammography, a patient’s breast is placed on a flat support plate and compressed with a parallel plate called a paddle.
Patient positioning
- The breast should be pulled out far enough from the chest wall so that all the breast is imaged,
- The distance from the nipple to the chest wall should not differ in the CC view and MLO view by more than 1 cm.
- The nipple should be in profile in at least one of the images from the view.
- The nipple is angled slightly up on the MLL view so that the entire breast is being lifted and the lower inferior portion of the breast is also evaluated.
- Each MLO view must capture the inframammary fold so that the inferior and posterior aspect of the breast is captured.
- An X-ray machine produces a small burst of X-rays that pass through a breast to a detector located on the opposite side.
- The detector can be either a photographic film plate, which captures the X-ray image on film or a solid-state detector, which transmits electronic signals to form a digital image.
- The images produced are called mammograms.
Patient preparation
- Take a detailed history of the patient including:
- Personal history of breast cancer
- Family history of breast or ovarian cancer
- Inherited genetic mutations like BRCA1 and BRCA2.
- Dense breast
- Ask the patient to bring the previous mammogram reports if available.
- Schedule mammography between day 7 to day 12 after the beginning of the woman’s last menstruation.
- Remove any clothing and jewelry above the waist.
- Maintain patient privacy.
- Position the breast on a breast support plate.
Interpretation of the Imaging Findings
The American College of Radiology’s (ACR) Breast Imaging Reporting and Data System (BIRADS) lexicon is the most widely used method to interpret the findings of mammography.
BIRADS
- The Breast Imaging Report and Data System (BIRADS) is a communication tool used in mammography.
- It provides a system of quality assurance intended to homogenize the data collected and the quality of mammographic reports.
- The mammographic features are described in the BIRADS as BIRADS’S lexicon which is as follows:
- Densities and masses
- Micro/macrocalcifications
- Architectural distortions
- Special cases including ducal ectasia, intramammary lymph node, or focal asymmetric density
- Associated findings: skin or nipple retraction, skin thickening, cutaneous lesions, axillary lymph nodes
Masses
- Masses are space-occupying lesions.
- It is described according to its shape, margin, and density.
- If the mass is found on two views but without discreet borders, it is known as focal asymmetry.
- When the mass finding is present in only one of the views, it is known as asymmetry.
Shape
- The shape can be irregular, round, oval, or lobular.
Margin
- It may be circumscribed, microlobulated, obscured, indistinct (Ill-defined), or speculated.
Density
- Tissue density refers to the percentage of glandular tissue related to breast fat within the breast.
- It looks white on a mammogram.
- It may be:
- Fatty (<25% dense),
- Fibroglandular (25%-50% dense),
- Heterogeneously dense (50% -75% dense), or
- Dense (>75% dense)
- As a woman’s breast has increasing fiber glandular densities, there is an increased chance of missing an underlying breast cancer because the fiber glandular tissue can mask the underlying malignancy.
Microcalcification
- Calcifications are the calcium deposits that lie within the breast.
- It may be benign or malignant calcification.
Architectural distortion
- It describes the rupture of the normal architecture with no apparent mass.
- Previous history of prior surgery or trauma to the breast in the location should be excluded.
Associated findings
- It can be described alone or associated with masses or microcalcification
- Findings to be noted:
- Skin retraction
- Axillary lymph node
- Nipple retraction
Location of lesion
- Location of lesion according to a clock, the location from the nipple area (subareolar, central, or axillary) and depth (anterior, middle, or posterior)
Reporting
The composition of the breast according to the breast density is reported as:
- Type 1 fatty breast (less than 10% of dense tissue)
- Type 2 fibroglandular (10 to 49% of dense tissue)
- Type 3 heterogeneously dense (49% to 90% of dense tissue)
- Type 4 Dense and homogenous (Greater than 90 % of dense tissue)
BIRADS Coding System
| BIRADS | Characteristics |
| BIRADS 0 | Incomplete AssessmentNeed for additional imaging evaluation |
| BIRADS 1 | Negative/ NormalNormal interval follow-up |
| BIRADS 2 | BenignNormal interval follow-up |
| BIRADS 3 | Probably benignA short interval follow-up is recommended |
| BIRADS 4 | Suspicious abnormalityA biopsy should be considered |
| BIRADS 5 | Highly suggestive of malignancyBiopsy or surgery should be performed |
| BIRADS 6 | Proved malignancyImaging is done for cancer staging or assessment after chemotherapy |
Limitations of Mammography
- Denser breast is difficult to image and assess for tumor diagnosis.
- X-Ray mammography may not be sufficiently sensitive and accurate in detecting cancer.
- Missed cancer may occur due to errors in technique, errors in detection, or errors in interpretation.
- Mammography causes overdiagnosis of breast cancer.
- Mammograms can detect cancer, but they cannot diagnose cancer.
- Not all cancers found by mammography can be cured.
Summary
- Mammography is the process of using low-dose X-ray to image the breast to detect breast cancer pathology and cancer.
- The American Cancer Society (ACS) recommends regular mammography screening starting at the age of 45 years.
- Mammography can be done for either screening or diagnostic purposes.
- In mammography, the patient’s breast is placed on a flat support plate and is compressed with a parallel plate called a paddle.
- The interpretations of mammography findings are widely done according to The Breast Imaging Report and Data System (BIRADS).
- Further, the early detection and screening of breast cancer can be done by mammography and it is 85% to 90% effective.
References
- Balleyguier, C., Ayadi, S., Nguyen, K. V., Vanel, D., Dromain, C., & Sigal, R. (2007, Feb). BIRADS classification in mammography. European Journal of Radiology, 61 (2), 192-194. DOI: 10.1016/j.ejrad.2006.08.033
- Egan, R.L. (1996, Jan). Mammography. The American Journal of Nursing, 66 (1), 108-111. https://doi.org/10.2307/3419514
- Loberg, M., Lousadal, M. L., Bretthauer, M., Kalager, M. (2015, May 1). Benefits and harms of mammography screening. Breast Cancer Res, 17(1), 63. doi: 10.1186/s13058-015-0525-z
- Sardanelli, F., Fallenberg, E. M., Clauser, P., Trimboli, R. M., Camps-Herrero, J., Helbich, T. H., Forrai, G., and EUSOBI. (2017, Feb). Mammograhy: an update of the EUSOBI recommendations on information for women. Insights Imaging, 8(1), 11-18. doi: 10.1007/s13244-016-0531-4
- Centers for Disease Control ND Prevention, CDC. (2022, Sep 26). What Is a Mammogram?. https://www.cdc.gov/cancer/breast/basic_info/mammograms.htm
- American Cancer Society. (2022, Jan 14). Mammogram Basics. Retrieved 2022, Dec 24 from https://www.cancer.org/cancer/breast-cancer/screening-tests-and-early-detection/mammograms/mammogram-basics.html
- Mayo Clinic. (2022, April 12). Mammogram. Retrieved 2022, Dec 24 fromhttps://www.mayoclinic.org/tests-procedures/mammogram/about/pac-20384806
- Niknejad, M. (2022. Aug 21). Breast imaging-reporting and data system (BI-RADS). Retrieved 2022, Dec 24 from https://radiopaedia.org/articles/breast-imaging-reporting-and-data-system-bi-rads