Introduction
Trigeminal neuralgia (tic douloureux) is also known as prosopalgia, the Suicide Disease, or Fothergill’s disease.
According to the International Association for the Study of Pain; Trigeminal Neuralgia (Tic Douloureux) is sudden, usually unilateral, severe brief stabbing recurrent pains in the distribution of one or more branches of the fifth cranial nerve.
According to the International Headache Society; Trigeminal Neuralgia is the painful unilateral affliction of the face, characterized by brief electric shock-like pain limited to the distribution of one or more divisions of the trigeminal nerve.
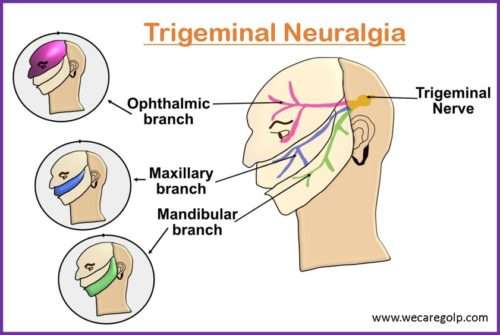
The Trigeminal Nerve
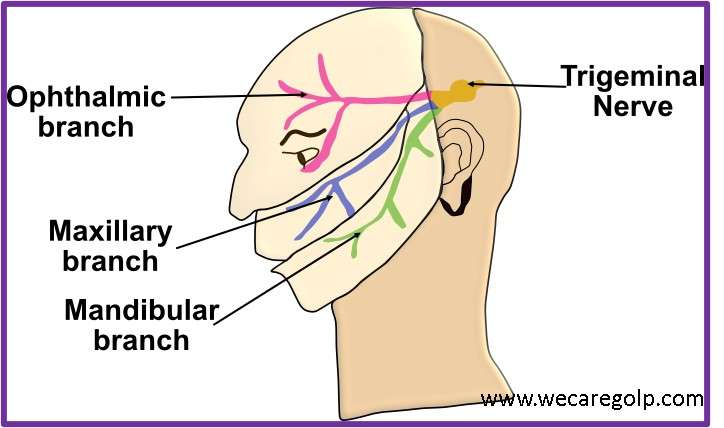
The Trigeminal Nerve is the fifth and the largest among all the cranial nerves. It is also the most complex of all the cranial nerves due to its extensive anatomy. The nerve has ophthalmic, maxillary, and mandibular branches. This is a mixed nerve having both sensory and motor fibers. The sensory fibers supply sensations to the face, mucous membranes, and other structures of the head. The motor fibers of the mandibular branch are for the muscles of mastication and contain proprioceptive fibers.
Classification of Trigeminal Neuralgia
According to the International Classification of Headache Disorders, Trigeminal neuralgia (TN) is divided into three types:
- Classic: TN related to vascular compression
- Secondary: TN due to a tumor along the trigeminal nerve due to an underlying disease
- Idiopathic: TN in which the cause is unknown
Prevalence
- A systematic review by the Journal of the American Dental Association identified a higher prevalence of TN in women, ranging from 0.03% to 0.3%.
- The most affected branches of the trigeminal nerve were themaxillary and mandibular.
- Women were three times more likely than men to have TN, and those between the ages of 37 and 67 were most affected.
Causes of Trigeminal Neuralgia
- No exact cause has been found, but degeneration or viral infection (Herpes virus, syphilis) may be suspected.
- It is often caused by a tortuous blood vessel compressing the trigeminal nerve that damages the nerve (myelin sheath) over time and interferes with its normal functioning.
Risk Factors of Trigeminal Neuralgia
- Advanced age
- Stroke
- Hypertension in women
- Infection of the teeth and jaw, Charcot-Marie-Tooth Disease
- Injury to the trigeminal nerve (facial trauma, sinus and oral surgery)
- Tumors in the trigeminal nerve region
- Arteriovenous malformation
- Multiple sclerosis
- Swelling and irritation
- Autoimmune or metabolic disorders like Diabetes Mellitus
- Chemical irritation
Signs and Symptoms of Trigeminal Neuralgia
- Pain is commonly evoked by trivial stimuli including washing, shaving, smoking, talking, and brushing the teeth, but may also occur spontaneously.
- The pain is abrupt in onset and termination and may remain for varying periods.
- The main symptom of trigeminal neuralgia is sharp, stabbing facial pain, sometimes presenting with facial muscle spasms.
- For some people, the pain is constant aching or burning pain. Flare-ups often begin with a tingling or numbness and progress to intense bursts of sharp pain.
- Pain attacks typically last from a few seconds to several minutes, and they can occur repeatedly for up to two hours.
- Trigeminal neuralgia usually affects only one side of the face. In rare cases, it can affect both sides but not at the same time.
- The parts of the face most commonly affected are the upper and lower jaw, teeth, and cheeks, while ears, eyes, forehead, lips, and nose are less common.
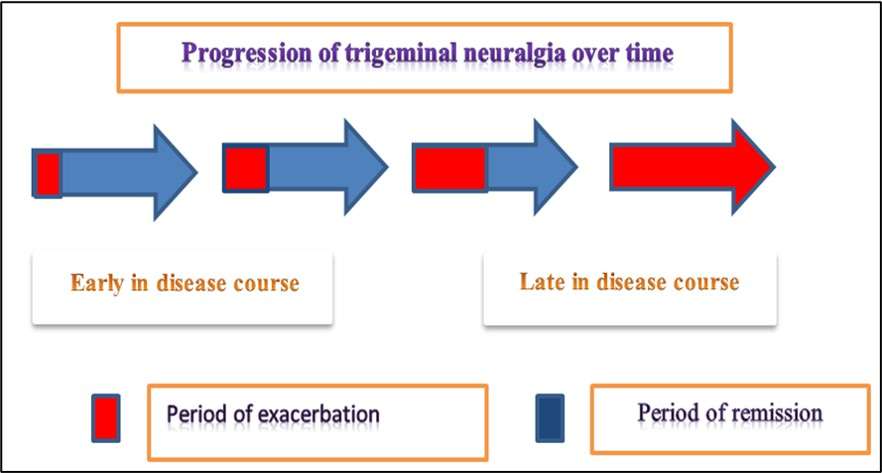
- The pain is progressive. Attacks of pain usually get worse over time, with fewer and shorter pain-free periods every time before they reoccur. Eventually, pain-free intervals disappear.
- Anxiety is common in patients due to the fear of an attack which can also lead to social isolation.
Pathophysiology
- The trigeminal nerve exists in the Pons and merges into the gasserian ganglion before it separates into three branches.
- The Superior cerebellar artery pressing on or grooving the root of the nerve causes pressure.
- This compression results in focal demyelination and hyperexcitability of nerve fibers.
- Nerve fibers fire in response to light touch resulting in brief episodes of intense pain.
Diagnosis
- Identification of characteristic symptoms through detailed history, neurological and clinical evaluation.
- Imaging techniques like Magnetic resonance imaging (MRI), CT scan, and Electromyography can be used to assess for or rule out underlying causes of TN including tumors or multiple sclerosis.
- Lumbar puncture for CSF analysis
- Blood test for sugar and kidney function
Treatment and Management of Trigeminal Neuralgia
The treatment and management options for patients with trigeminal neuralgia depend on a variety of factors like age, general health, disease severity, and the underlying cause.
Pharmacotherapy
First-line treatment for patients with both Classic and Idiopathic TN is pharmacologic therapy. It is recommended to treat the underlying lesion or disease in patients with secondary TN, even it may respond well to pharmacotherapy.
- The most commonly used medication is carbamazepine (an anticonvulsant) starting at a low dose and gradually increasing until the pain is controlled. It controls pain for most people in the early stages of the disease but in some patients, the effectiveness of the drug decreases over time.
- Oxcarbazepine is a newer drug that is used increasingly nowadays as first-line therapy in patients who do not respond to or cannot tolerate carbamazepine.
- Baclofen (a muscle relaxant) can be used.
- Other medications include phenytoin, gabapentin, lamotrigine, clonazepam, and valproic acid.
- Botulinum Toxin injections can be beneficial for the middle-aged and the elderly, who are refractory to medical therapy or who cannot tolerate medical therapy due to its side effects.
Surgical Therapy
Surgery may be an option for patients who are unable to respond to medical treatment.
Microvascular decompression
- Microvascular decompression is one of the most common procedures which involve craniotomy and posterior fossa exploration for identifying and moving the blood vessel that is compressing the trigeminal nerve.
- A soft cushion is then inserted between the nerve and the vessel to allow the nerve to recover, which eventually leads to pain relief. It is the most effective and invasive procedure which results in sustained pain relief for greater than 10 years.
Ablative procedures
- Ablative procedures include chemical injection, rhizotomy with thermocoagulation, or mechanical balloon compression.
- These procedures damage the trigeminal nerve root, thus interrupting the pain transmission signals to the brain.
Radiosurgery
- Radiosurgery creates a lesion near the nerve root interrupting the pain signals from transmission to the brain.
- Pain relief is delayed by up to several weeks or months because the formation of the lesion can be slow.
- This is one of the least invasive procedures and can be repeated in patients who have a reoccurrence of pain.
Peripheral neurectomy and nerve block
- Peripheral neurectomy and nerve block are performed on peripheral branches (supraorbital, infraorbital, lingual, and alveolar) of the trigeminal nerve.
- This can be done by incision, alcohol injection, radiofrequency lesioning, or cryotherapy.
- It is safe for elderly patients and in remote areas where neurosurgical facilities are not readily available.
Complications of Trigeminal Neuralgia
- The pain in trigeminal neuralgia is so severe and debilitating that many patients can develop depression if they are not adequately treated.
- Severe pain associated with facial twitches can lead to social withdrawal due to embarrassment and fear of an impending attack.
- Long-term treatment with anticonvulsant drugs can have adverse drug effects.
- There may be risks associated with microvascular decompression and percutaneous neurosurgical procedures. Permanent facial numbness can develop on the affected side.
- Patients can develop corneal anesthesia and jaw weakness occasionally.
- Anesthesia dolorosa (an uncommon differentiation pain that can occur after traumatic or surgical injury to the trigeminal nerve) is seen in a few patients. It can be more disabling than the original TN.
Prevention
- Currently, there are no specific guidelines on the prevention of trigeminal neuralgia but people who already have the condition may prevent attacks and pain by keeping track of potential triggers and avoiding them.
Prognosis
- Trigeminal neuralgia is not usually a life-threatening condition, but it can lead to lifelong pain and disability.
- The course of the disease is variable.
- Some patients have persistent background facial pain simultaneously with TN.
- In some patients, the pain attacks worsen over time, with fewer and shorter pain-free intervals every time before they reoccur.
- The medications might also lose effectiveness over time. Correct diagnosis and proper management lead to a good prognosis.
Summary
- Trigeminal neuralgia is a chronic neuropathic pain disorder characterized by severe, unilateral, paroxysmal facial pain.
- The pain results from mild stimulation in the sensory distribution of the trigeminal nerve.
- The onset of symptoms is usually sudden or spontaneous.
- Pain is triggered by talking, chewing, or brushing teeth.
- The pain is often described as burning, stabbing, or electric shock-like.
- The ability to perform activities of daily living is severely limited.
- Types can be classic, secondary, and idiopathic depending on the cause.
- The first line of treatment is medication.
- Other procedures are surgical intervention, radiosurgery, ablative therapy, etc.
References
- Mandal, G.N. (2012). Textbook of Adult Nursing. Makalu Publication House, Kathmandu
- Sharma, M. et. al. (2020). Comprehensive Textbook of Medical Surgical Nursing. Samikshya Publication, Kathmandu
- Toledo, I.P.D., Reús, J. C., Fernandes, M.. Porporatti, A.L., Peres, M. A., Takaschima, A., Linhares, M. N., Guerra, E., Canto, G.D.L. (2016, July). Prevalence of trigeminal neuralgia: A systematic review. The Journal of the American Dental Association, 147(7):570-576.e2. https://doi.org/10.1016/j.adaj.2016.02.014
- Lee, C. H., Jang, H. Y., Won, H. S., Kim, J. S., & Kim, Y. D. (2021). Epidemiology of trigeminal neuralgia: an electronic population health data study in Korea. The Korean journal of pain, 34(3): 332-338. https://doi.org/10.3344/kjp.2021.34.3.332
- National Institute of Neurological Disorders and Stroke. (June 2013). Trigeminal Neuralgia Fact Sheet, Publication No. 13-5116. https://www.ninds.nih.gov/trigeminal-neuralgia-fact-sheet
- Stanford Health Care (n.d.). Trigeminal Neuralgia. https://stanfordhealthcare.org/medical-conditions/brain-and-nerves/trigeminal-neuralgia.html
- Pilitsis, J. G., Khazen, O. (n.d.). Trigeminal Neuralgia. American Association of Neurological Surgeons. https://www.aans.org/Patients/Neurosurgical-Conditions-and-Treatments/Trigeminal-Neuralgia