Introduction
The word pneumonia originated from the Greek word- ‘pneumon’ meaning ‘lung’. So, the word pneumonia is a disease related to the lungs.
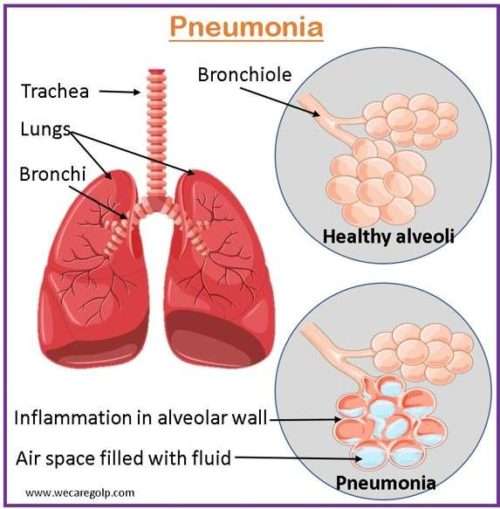
- The lung is a part of the lower respiratory tract which is made up of small sacs called alveoli. When a healthy person breathes, it is filled with air.
- Pneumonia is an inflammatory condition of lung parenchyma typically involving alveolar space which is caused by microbial agents.
- This inflammatory condition in alveolar spaces results in the consolidation of lung tissues. That is why there is an accumulation of a clear to pale yellow watery fluid (serous fluids), mucus, and inflammatory cells in response to infection which leads to difficulty in breathing and reduces in oxygen intake.
Incidence
- The prevalence of pneumonia varies according to a variety of factors, including age, underlying health conditions, and geographic location. It is more common in young children, the elderly, and people with compromised immune systems.
- According to WHO, pneumonia is one of the leading causes of death for children under the age of five, accounting for approximately 15% of all deaths in this age group.
- In 2019, it was estimated that 2.5 million people died from pneumonia worldwide.
- According to data from the CDC, pneumonia was the cause of death for more than 47,000 Americans in 2020.
Types of Pneumonia
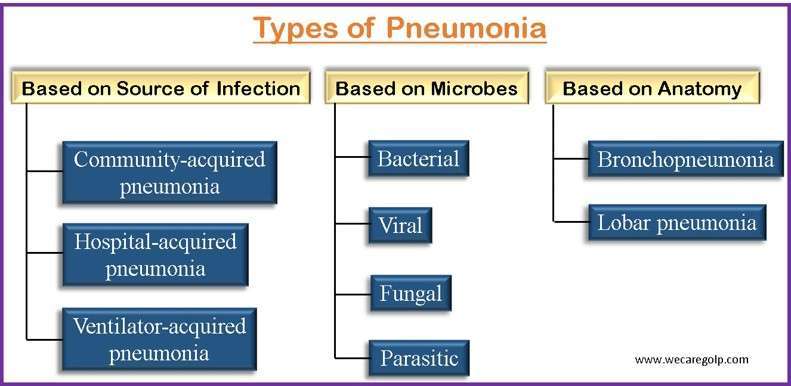
Based on source of infection
- Community-acquired pneumonia: Community-acquired pneumonia (CAP) is an acute infection of pulmonary parenchyma acquired outside of the hospital.
- Hospital-acquired pneumonia: Hospital-acquired pneumonia refers to pneumonia that is acquired ≥48 hours after hospitalization.
- Ventilator-acquired pneumonia: Ventilator-acquired pneumonia refers to pneumonia that is acquired ≥48 hours after endotracheal intubation.
Based on microbes
| Viral | Influenza virus type A Cytomegalovirus |
| Bacterial | Streptococcus pneumoniae (pneumococcal pneumonia) Klebsiella pneumonia Hemophilus influenza Pseudomonas aeruginosa Streptococcus aureus |
| Fungal | Pneumocystis carinii pneumonia is a rare fungal infection seen in patients with impaired immune function |
| Parasitic | Parasitic-necrotizing pneumonia is caused by the uncommon parasitic lung illness known as pulmonary strongyloidiasis. It primarily affects people with compromised immune systems and is typically seen in regions with high parasite infection rates. |
Based on Anatomy
- Bronchopneumonia: It is distributed in a patchy fashion extending from the bronchi to the surrounding lung parenchyma.
- Lobar pneumonia: In these one or more lobes are affected.
Risk Factors of Pneumonia
- Age: Children who are 2 years old or younger and people who are age 65 or older
- Chronic conditions: COPD, Cancer, Diabetes, Chronic liver disease, Renal impairment
- Immunosuppressive disorders: HIV, and Solid organ transplantation
- Factors that increase the risk of aspiration: Placement of endotracheal tube, and neurological disorders like stroke, Parkinson’s disease, dementia, etc.
- Healthcare setting: People who are in the hospital, hemodialysis center, and a long-term care facility.
- Lifestyle factors: Smoking, high alcohol intake, malnutrition
Causes of Pneumonia
Primary
- Primary pneumonia is caused directly by the virus itself.
- Influenza viruses
- Respiratory syncytial virus (RSV)
- SARS-CoV-2
- It is often associated with conditions that cause an increase in left atrial pressure
Secondary
- Secondary pneumonia results from bacterial superinfection occurring after a period of clinical improvement, typically by
- Streptococcus pneumoniae
- Hemophilus influenzae
- Staphylococcus aureus
- Mycoplasma pneumoniae (especially in children)
- It is also caused by the hematogenous spread of bacteria from a distant focus.
- It is more common in older adults and patients with comorbidities such as
- Chronic respiratory or cardiovascular disease
- Diabetes mellitus
- Chronic hepatic or renal failure
Signs and Symptoms of Pneumonia
- Lassitude (lethargy)
- Dyspnea (painful breathing)
- Stabbing chest pain aggravated by respiration and coughing
- Rapidly rising fever (up to 105F or 40.55C)
- Chills
- Shortness of breath
- Tachypnea (rapid breathing)
- Tachycardia (rapid pulse)
- Cyanosed lips and nail beds
- Rapid shallow breathing
- Cough with purulent, rusty, greenish sputum according to the causative agent
- Pneumococcal infection: Purulent, rusty sputum
- Staphylococcal infection: Yellow, blood-streaked sputum
- Klebsiella infection: Red, gelatinous sputum
- Mycoplasma: Nonproductive sputum
Other symptoms may include
- Muscle pain
- Fatigue
- Headache
- Anorexia (loss of appetite)
- Nausea, vomiting, and diarrhea
- Delirium (confused mental state), particularly in older patients
Pathophysiology of Pneumonia
- Usually, the upper airway protects against infectious pathogens.
- Microorganisms can infiltrate the lower respiratory tract when the host’s defenses weaken as a result of an underlying cause, or they can aspirate the usual flora of the oropharynx into the lungs.
- Blood-borne pathogens can cause pneumonia if they become lodged in the pulmonary capillary beds and enter the bloodstream.
- WBC and neutrophils enter the alveoli and fill the normally air-containing area to start the inflammatory process. Inflammatory reactions cause white blood cells and neutrophils to occupy air-filled spaces within the alveoli, leading to their obstruction and subsequent airlessness.
- This hinders the exchange of oxygen and carbon dioxide, affecting both ventilation and diffusion.
- Obstruction caused by secretions and mucosal edema also compromises adequate ventilation of the lungs.
- Blood low in oxygen is transported to the lungs via the pulmonary artery. Blood that is partially oxygenated goes to the left heart which contributes to hypoxemia.
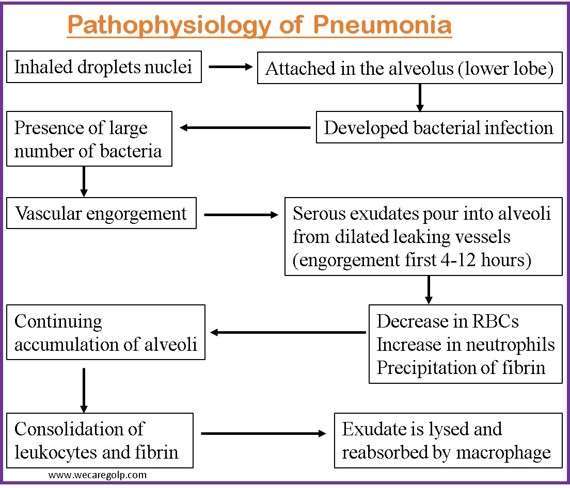
Pneumonia can explain in four phases.
Congestion
- This stage is also called hyperemia.
- It typically takes place within the first 24 hours of pneumonia.
- It is characterized by
- Vascular engorgement,
- Multiple bacteria, and
- Intra-alveolar fluid.
- The lung tissues will be very heavy, boggy, and red.
- There are congested capillaries in the alveolar walls, and the infection spreads to the hilum and pleura.
- During this stage, a person may experience deep breathing and coughing.
- In this stage, red blood cells (RBC) and neutrophils are present in a few amounts.
Red hepatization
- After a few days of the congestion stage, red hepatization begins.
- Characteristics of this phase are
- Red, firm, and airless lungs, resembling liver tissue
- Vascular engorgement and congestion
- The alveoli contain RBCs, neutrophils, fibrin, and desquamated epithelial cells.
Gray hepatization
- In gray hepatization, the lungs turn gray with liver-like consistency due to
- The breakdown of RBCs
- Fibrinopurulent exudate
- Increased number of white blood cells (WBCs) infiltrating the alveoli.
- The macrophages start to appear.
- This phase begins two to three days following red hepatization and lasts four to eight days.
Resolution
- The resolution process involves the substitution of polymorph nuclear leukocytes with highly phagocytic macrophages that effectively eliminate organisms.
- It begins on the eighth day.
- It is characterized by clearing the exudates by resident macrophages with or without residual scar tissue formation.
Diagnosis of Pneumonia
History
- Recent respiratory tract infection
- Any recent travel history
- Occupation
- Exposure to other sick people
Physical examination
- Reduced and abnormal sounds (bubbling, crackling, rumbling) heard in the lung on auscultation
Blood test
- Increased White Blood Cell is a symbol of infection.
- Blood culture shows whether has spread to the blood.
- Arterial blood gas (ABG) measures blood oxygen level.
Pulse oximetry
- Measures oxygen level in the blood.
Imaging
- Chest X-ray: It shows pulmonary infiltration. It helps figure out the location and extent of inflammation in the lungs.
- Chest CT scan: It shows the affected part of the lungs by the infection.
Sputum culture
- It helps find out pathogens.
- There are other methods available for gathering specimens, some of which are more intrusive.
- For example, sputum can be collected through nasotracheal or orotracheal suctioning using a sputum trap.
Bronchoscopy
- This is another option obtaining sputum through fiberoptic bronchoscopy.
- When a diagnosis cannot be determined through expectorated or induced specimens, bronchoscopy is typically utilized for individuals experiencing
- Acute severe infections
- Refractory infections, or chronic cases, and
- For those with compromised immune systems
- Purposes:
- To examine the bronchi (the main airways of the lungs) directly
- To evaluate and diagnose lung problems
- To assess blockages
- To collect a sample of the lung tissues and fluid from the lungs to find the cause of pneumonia.
Thoracocentesis
- A small needle is inserted to take a fluid sample from pleural space (space between lungs and chest wall).
- The collected sample is sent to the lab to find out the causative bacteria.
Management of Pneumonia
Medical Management
Bacterial pneumonia
- Culture and sensitivity tests will be done on blood and sputum to determine appropriate antibiotic therapy.
Viral pneumonia
- The treatment for viral pneumonia is mostly supportive.
- Sometimes, antiviral medicines can be used for long-term and severe infections.
- Antibiotics are ineffective against viral upper respiratory infections and pneumonia, and they may cause side effects.
- Antibiotics are only prescribed for a viral respiratory infection if there is secondary bacterial pneumonia, bronchitis, or sinusitis.
Fungal pneumonia
- Antifungal medications can treat pneumonia if the infection is due to fungus.
Supportive Management
Supportive treatment includes hydration, bed rest, antipyretics, antihistamine, nasal decongestants, and oxygen therapy.
- Because fever and tachypnea can cause insensible fluid losses, hydration is an essential component of treatment. Warm and moist inhalation helps soothe irritation in the bronchi.
- Bed rest is recommended until the infection is subsided.
- Antipyretics may be used to treat headaches and fever.
- Antihistamines may provide benefits with reduced sneezing and rhinorrhea.
- The associated cough may be treated with antitussive medications.
- Respiratory support includes endotracheal intubations, high oxygen concentration (fraction of inspired oxygen [FiO2]), and mechanical ventilation.
- If hypoxemia develops, oxygen is administered. Pulse oximetry and arterial blood gas analysis are used to determine the requirement for oxygen and to evaluate the effectiveness of the therapy.
- In COPD patients, a high concentration of oxygen is contraindicated because there is a risk of worsening alveolar ventilation by reducing ventilatory drive, promoting further respiratory decompensation.
Complications of Pneumonia
Patients with other underlying chronic conditions are more likely than others to experience complications from it.
- Pleurisy
- Pleural effusion
- Emphysema
- Abscess
- Atelectasis (collapsed alveoli)
- Acute respiratory distress syndrome (ARDS)
- Sepsis (bacteria in the bloodstream)
- Meningitis
- Pericarditis
- Endocarditis
Prevention of Pneumonia
Vaccination
- To avoid seasonal influenza, we should be vaccinated against it every year. As pneumonia frequently results from the flu, avoiding the virus is an effective strategy to avoid pneumonia.
- Pneumococcal pneumonia is a prevalent type of bacterial pneumonia, certain people should get vaccinated against it including:
- Children under the age of 2.
- Children aged 2 to 5 who suffer from illnesses like diabetes, heart disease, or chronic lung disease.
- Adults aged 19 and 64 who smoke or who have certain risk factors for heart disease, diabetes, COPD, or asthma.
- Pneumococcal pneumonia vaccinations should be administered to all people aged 65 and over.
- Depending on their health, additional pneumococcal immunizations may be advised for children and adults who are at higher risk for pneumococcal illness.
- Other vaccines
- Measles
- Hib (Hemophilus influenza type b)
- Covid 19
- Chickenpox
- Whooping cough (Pertussis)
Other Preventive Measures
Hand hygiene
- Hands should be washed regularly, especially after using the restroom, changing diapers, coughing or blowing nose, and before consuming or preparing food.
Quit smoking and avoid alcohol
- Smokers are reported to have an increased risk of developing pneumonia because tobacco harms the lungs’ ability to fight against infection.
- Current tobacco smokers are more than twice as adults who have never smoked to develop CAP, whereas people who consume alcohol (or in larger amounts) have an 83% increased risk of CAP compared to those who consume no (or less) alcohol (Simou et al., 2018).
- Every 10-20 g more alcohol consumed per day increases the risk of CAP by 8%.
- The pneumococcal pneumonia vaccine is recommended for high-risk populations, including tobacco smokers to help prevent pneumococcal pneumonia.
Adopting healthy lifestyle
- Healthy eating, adequate rest, regular exercise, and other good health practices all work to prevent viral and respiratory diseases.
Maintaining pre-existing respiratory disease
- Existing medical issues including asthma, COPD, diabetes, and heart disease should be maintained under control.
Prognosis
- Age of the patient, overall health (existence of comorbidities), and the environment in which antibiotic treatment is administered play a significant role in determining prognosis.
- In general, the mortality rate for outpatients is less than 1%, although it ranges from 5% to 15% for hospitalized patients.
- Nevertheless, it rises to between 20% and 50% for patients who need admission to an intensive care unit.
- Patients with CAP have readmission rates that vary from 7% to 12%.
- Readmission occurs most frequently as a result of comorbidities (mostly cardiovascular, pulmonary, or neurological disease) worsening.
Summary
- Pneumonia is a lung inflammatory condition caused by viruses, bacteria, or other microorganisms.
- It is a common illness that can affect people of all ages, but it is more common in young children, the elderly, and people with compromised immune systems.
- Coughing, fever, chest pain, and difficulty breathing are all symptoms of pneumonia.
- The treatment is determined by the source of the infection. Antibiotics can be used to treat bacterial pneumonia, but viral pneumonia usually resolves on its own.
- Hospitalization may be required in severe cases to provide supportive care such as oxygen therapy.
- Vaccination against certain types of bacteria and viruses, good hygiene practices such as hand washing, avoiding close contact with sick people, and quitting smoking are all preventive measures for pneumonia.
- Early detection and treatment are critical for avoiding complications and lowering the risk of severe illness. If symptoms appear, it is critical to seek medical attention, especially in high-risk individuals.
References
- Mandal, G.N. (2019). A Textbook of Medical Surgical Nursing. Makalu Publication House
- Lim, W. S. (2022). Pneumonia—Overview. Encyclopedia of Respiratory Medicine, 185–197. https://doi.org/10.1016/b978-0-12-801238-3.11636-8
- Aston S.J. (2017, Oct). Pneumonia in the developing world: Characteristic features and approach to management. Respirology,22(7),1276–1287. DOI: 10.1111/resp.13112
- Htun, T. P., Sun, Y., Chua, H. T., & Pang, J. (2019). Clinical features for diagnosis of pneumonia among adults in primary care setting: A systematic and meta-review. Scientific Reports, 9, 7600. https://doi.org/10.1038/s41598-019-44145-y
- Torres, A., Niederman, M. S., Menéndez, R., Chalmers, J. D., Wunderink, R. G., & Van Der Poll, T. (2021). Pneumonia. Nature Reviews Disease Primers, 7, 25. https://doi.org/10.1038/s41572-021-00259-0
- Jones, B., Dean, N. C., Wunderink, R., & Sockrider, M. (2016). What is Pneumonia? American Journal of Respiratory and Critical Care Medicine, 193(1), 1-2. https://doi.org/10.1164/rccm.1931p1
- Rabbat, A., & Huchon, G. (2008). Nonbacterial Pneumonia. Clinical Respiratory Medicine, 351–364. https://doi.org/10.1016/b978-032304825-5.10028-5
- American Lung Association. (2022, Nov 17). Pneumonia Symptoms and Diagnosis. Retrieved on 2023, Apr 23 from https://www.lung.org/lung-health-diseases/lung-disease-lookup/pneumonia/symptoms-and-diagnosis