Introduction
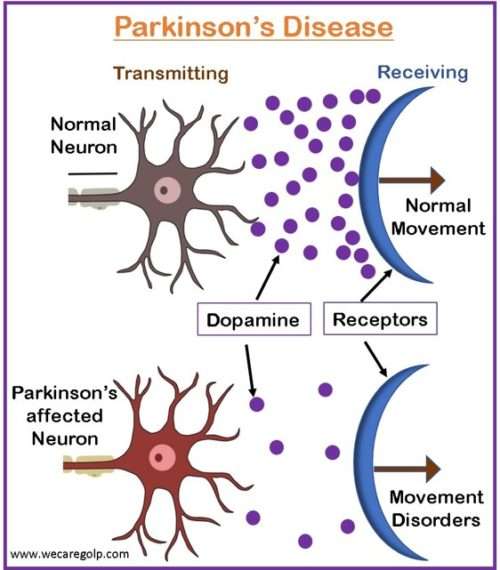
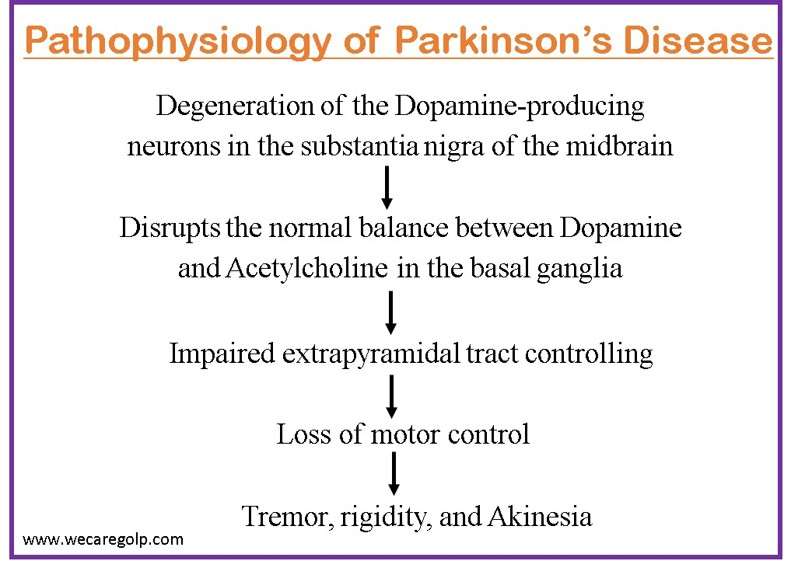
Parkinson’s disease (PD) is a chronic progressive disorder caused by the degeneration of nerve cells in the part of the brain called the substantia nigra, which controls body movement.
- Due to Parkinson’s disease, the nerve cells die or become impaired. Thus, it loses the ability to produce an important chemical called dopamine.
- Dopamine transmits signals between areas in the brain that, when working normally, coordinate smooth and balanced muscle movement.
- The classic motor features of the disease typically start insidiously and emerge slowly over weeks or months.
- The three cardinal signs of Parkinson’s disease are resting tremor, rigidity, and bradykinesia with tremor being the first symptom.
- In 1817, James Parkinson first described the condition, and Jean-Martin Charcot further specified it.
Incidence
- Parkinson’s disease affects 1–2 per 1000 of the population.
- The prevalence is increasing with age and affects 1% of the population above 60 years.
- Some genetic factors can be identified in 5–10% of the patients.
Types of Parkinson’s Disease
The types of Parkinson’s disease are as follows:
- Idiopathic Parkinson’s disease
- Drug-induced parkinsonism
- Progressive supranuclear palsy
- Vascular Parkinsonism
- Early-Onset Parkinson’s
- Normal-pressure hydrocephalus
- Multiple system atrophy
- Dementia with Lewy bodies
Stages of Parkinson’s Disease
Hoehn and Yahr’s scale divides symptoms of Parkinson’s disease into five stages.
Stage 1
- It is the mildest form in which patients may not experience noticeable symptoms or they may be isolated to only one side of the body.
- The symptoms usually do not interfere with daily living.
Stage 2
- The progression from stage 1 to stage 2 can take months or even years varying from person to person.
- This is the moderate stage in which the patient experience symptoms such as muscle stiffness, tremors, changes in facial expressions, trembling, etc.
- Muscle stiffness can complicate daily performance but the patient is unlikely to experience balance problems.
- Noticeable changes may appear on both sides of the body like changes in posture, gait, and facial expressions.
Stage 3
- This is the middle stage in which symptoms reach a turning point.
- The patient is unlikely to experience new symptoms but the old ones may be more noticeable interfering with all daily tasks.
- Movements and activities slow down. Falls are more common due to significant balance issues.
- However, people with stage 3 Parkinson’s disease usually can maintain their independence and complete activities without much assistance from others.
Stage 4
- Significant changes are noted while progressing from stage 3 to stage 4.
- At this point, the patient will experience great difficulty standing without a walker or any assistive device.
- Muscle movements and reactions also slow down significantly.
- Living alone can be dangerous.
Stage 5
- This is the most advanced stage in which there are severe symptoms.
- Patients need 24-hour assistance.
- It will be difficult to stand and a wheelchair may be required.
- It is possible to experience confusion, delusions, and hallucinations.
Causes of Parkinson’s Disease
- The underlying cause is largely unknown.
- According to scientists, a combination of genetic and environmental factors could be the causing factors.
Risk Factors of Parkinson’s Disease
- Age: People usually develop the disease around the age of 60 or older.
- Heredity: Parkinson’s disease in a close relative increases the chances of developing the disease.
- Sex: Men are more likely to develop Parkinson’s disease than women.
- Pesticide: Exposure to benomyl, paraquat, ziram, maneb, and several types of organophosphate pesticides has an association with Parkinson’s disease.
- Heavy metals and the workplace: Welders may develop symptoms associated with Parkinson’s disease, including slowness of movement in the arms and hands, speech problems, and reduced facial expressions by exposure to heavy manganese metal.
- Head Injuries: It causes the death of dopaminergic neurons which may lead to Parkinson’s disease.
- Air Pollution: It acts on the biological pathways that are involved in Parkinson’s disease causing an accumulation of toxic alpha-synuclein deposits, neuro-inflammation, and an altered brain immune response.
- Diet and Lifestyle: Theseare related to the development and progression of Parkinson’s disease.
- Cooking meat: Heterocyclic amines (HCAs) are chemicals that are produced during high-temperature meat cooking. They are toxic to the dopaminergic neurons which are affected in Parkinson’s disease.
- Vitamin D plays an important role in maintaining good balance and muscle strength as well as regulating the normal function of brain cells. Thus, Vitamin D deficiency is related to Parkinson’s disease.
- Exercise: Regular and higher levels of physical activity improve balance and decreases the risk of Parkinson’s disease.
Signs and Symptoms of Parkinson’s Disease
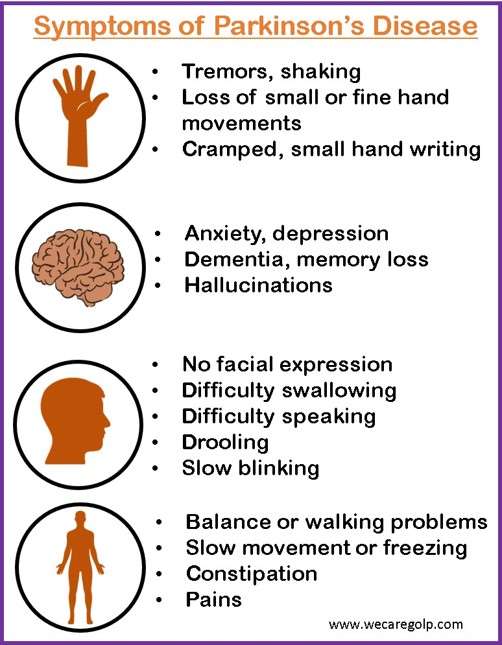
Cardinal signs
- Resting tremors (arms, legs, face, jaw)
- Bradykinesia (impairment of voluntary motor control and slow movements or freezing)
- Rigidity (limbs stiffness)
- Loss of postural reflexes (problems with coordination and balance)
Secondary motor symptoms
- Hypomimia (facial masking or a loss or reduction of facial expressions)
- Dysarthria (speaking difficulty)
- Dysphagia (swallowing difficulty)
- Sialorrhoea (hypersalivation or excessive drooling)
- Micrographia (cramped, small handwriting)
- Shuffling gait
- Festination ( a gait marked by an involuntary hurrying in walking)
- Freezing
- Dystonia (neurological movement disorder)
- Glabellar reflexes
Non-motor symptoms
- Autonomic dysfunction
- Cognitive/neurobehavioral abnormalities
- Sleep disorders and sensory abnormalities such as anosmia, paresthesias, and pain
Non-specific symptoms
- Falling frequently
- Difficulty grooming, dressing, and feeding,
- Blank facial expression
- Sudden freezing spells
- Excessive sweating, etc.
Pathophysiology of Parkinson’s Disease
Diagnosis of Parkinson’s Disease
Imaging tests
- MRI: An MRI can reveal a brain tumor, normal pressure hydrocephalus, or vascular parkinsonism.
- Dopamine transporter (DAT): A DAT scan is a type of imaging used to measure the quantity of dopamine in the brain. An abnormally low level of dopamine can diagnose Parkinson’s disease.
- Neuroimaging: It is necessary when patients have atypical features like early cognitive impairment, early falls, ideomotor apraxia (a neurological disorder characterized by the inability to correctly imitate hand gestures and voluntarily mime tool use, e.g., pretend to brush one’s hair or hammer a nail), hyperreflexia, etc.
- Positron emission tomography (PET)
- Near-infrared spectroscopy (NIRS)
- Magnetoencephalogram (MEG)
- Electroencephalography (EEG)
- Functional magnetic resonance imaging (fMRI)
- Genetic test: Genetic test may assist the doctor in determining the primary cause if the patient has a family history of parkinsonism.
- Other lab tests are done to rule out other conditions that may be causing the symptoms.
Treatment/Management of Parkinson’s Disease
- A combination of lifestyle changes, medications, and surgical treatments is required for the treatment of Parkinson’s disease.
- Management requires careful consideration of the patient’s signs and symptoms, stage of disease, age, degree of functional disability, level of physical activity, and productivity.
- Adequate rest, exercise, and a balanced diet are important.
- Speech therapy, occupational therapy, diversional therapy, and physical therapy can also help improve communication and self-care.
Medical Management
Medication is necessary for managing various physical and mental health symptoms in almost all patients. Medications relieve the symptoms by stimulating the remaining cells in the substantia nigra to produce more dopamine or by inhibiting the acetylcholine that is produced therefore restoring the balance between the chemicals in the brain.
Levodopa
- Levodopa is regarded as the gold standard of Parkinson’s therapy which works by crossing the blood-brain barrier where it is converted into dopamine.
- Levodopa reduces the symptoms of slowness, stiffness, and tremor but does not slow the disease progression.
- The addition of the drug Carbidopa prevents levodopa from being metabolized in the gastrointestinal tract, liver, and other tissues, thus allowing it to reach the brain more effectively.
- Therefore, a smaller dose of levodopa is needed to treat symptoms and reduce severe side effects like nausea and vomiting.
Dopamine Agonists
- Dopamine agonists are medications that mimic the role of chemical messengers in the brain, causing the neurons to react in the same way as with dopamine.
- Bromocriptine
- Pergolide
- Pramipexole
- They are given alone or combined with levodopa.
- The drugs may be used in the early stages of the disease or to lengthen the effective duration of levodopa.
Catechol-O-methyl transferase (COMT) Inhibitors
- In the bloodstream, an enzyme COMT metabolizes levodopa.
- By blocking COMT, more levodopa can penetrate the brain and increase the effectiveness of treatment.
- Entacapone and tolcapone are drugs that are used to treat fluctuations in the response to levodopa.
- Tolcapone is given only to those patients whose symptoms are not properly controlled by other medications because it has potentially serious toxic effects on the liver.
Selegiline
- This medication slows down the activity of the enzyme monoamine oxidase B (MAO-B).
- MAO-B metabolizes dopamine in the brain, delaying the breakdown of naturally occurring dopamine and dopamine formed from levodopa.
- Thus, selegiline enhances and prolongs the effectiveness of levodopa.
Anticholinergic medications
- Anticholinergic medicines block the action of acetylcholine.
- Trihexyphenidyl
- Biperiden HCL
- Procyclidine
- Acetylcholine is a chemical found in the brain whose effects become more pronounced when the dopamine level is dropped.
- These medications are very useful in the treatment of muscle rigidity, tremors, and medication-induced Parkinsonism.
Amantadine
- Amantadine is an antiviral medication that is often used in the early stages of the disease which helps reduce symptoms of Parkinson’s disease.
- It is also effective in treating the jerky motions associated with the disease.
Surgical Management
Lesion surgery
Involuntary movements of Parkinson’s are relieved by operating on the deep brain structures involved in motion control – the thalamus, globus pallidus, and subthalamic nucleus.
Pallidotomy
- Pallidotomy is performed by inserting a wire probe into the globus pallidus (a very small region that is hyperactive in Parkinson’s disease due to the loss of dopamine).
- Creating lesions in the region helps restore the balance required for normal movement.
Thalamotomy
- Radiofrequency energy currents are used to destroy a small, but specific, portion of the thalamus in thalamotomy.
- A small number of patients who have disabling tremors in the arm or hand may get benefit from this procedure.
Deep Brain Stimulation (DBS)
- In comparison to pallidotomy and thalamotomy, DBS is a safer alternative.
- Small electrodes are inserted into the brain to deliver an electrical impulse to the globus pallidus or the subthalamic nucleus of the thalamus, which are deep regions of the brain involved in motor function.
- The electrode is connected to wires that lead to an impulse generator that is placed under the collarbone and beneath the skin.
- The electrodes are usually placed on one side of the brain and patients have a controller to turn the device on or off.
- The procedure ultimately suppresses the tremor.
Complications
- Cognitive problems (dementia) and thinking difficulties usually occur in the later stages of Parkinson’s disease and are not usually improved by medications.
- Depression and emotional changes: Depression sometimes is seen in the very early stages before starting the treatment. Emotional changes such as anxiety, fear, or loss of motivation may also be seen.
- Swallowing problems occur when the disease condition progresses. Slow swallowing causes saliva accumulation in the mouth resulting in drooling.
- Chewing and eating problems are seen in the late stage due to effects on the muscles of the mouth, making chewing difficult. This may lead to choking and poor nutrition.
- People with Parkinson’s disease often have sleep problems like waking up early or falling asleep during the day or waking up frequently throughout the night. Sleep behavior disorder with rapid eye movement is another possibility for patients.
- Bladder problems including being unable to control urine or having difficulty in urinating may occur.
- Constipation develops mainly due to a slower digestive tract.
- Orthostatic hypotension: It is a sudden condition of low blood pressure when you stand up from a seated or lying down position.
- Smell dysfunction: Difficulty identifying certain odors or the difference between odors.
- Experience Fatigue and loss of energy occur especially later in the day.
- Patients may experience pain, either in specific areas of their bodies or throughout their bodies.
- Some patients may notice a decrease in sexual desire or performance.
Prevention
- Because the cause of Parkinson’s disease is unknown in about 95% of the case, there are no effective ways to prevent the disease.
- However, some research proved the following measures to reduce the risk of PD.
- Regular aerobic exercise (reduce sadness and anxiety improving physical strength and balance)
- Caffeine and Vitamin D consumption
- Protection from toxins like pesticides
- Healthy diet (eating a high-fiber diet, fruits, vegetables, grains, drinking enough water to avoid constipation)
Prognosis
- With advances in treatment and management, most people with the disease nowadays have a normal or near-normal life expectancy.
- If left untreated, motor symptoms advance aggressively in the early stages of the disease and slowly later whereas untreated, cases may lose independent ambulation and be bedridden after a period of 8 to 10 years.
- Parkinson’s disease does not directly lead to death but the condition can place great stress on the body making people more vulnerable to serious and life-threatening infections.
Summary
- Parkinson’s disease is a chronic, progressive neurological disorder that occurs due to damage or death of dopamine-producing cells in the brain, leading to a decrease in the neurotransmitter called Dopamine.
- The cardinal signs are resting tremors, rigidity, and bradykinesia with tremor being the first sign.
- Management includes supportive treatments, such as physiotherapy and occupational therapy as well as medication and brain surgery.
- With advances in treatment, most people with Parkinson’s disease nowadays have a normal or near-normal life expectancy.
References
- Mandal, G.N. (2012), Textbook of Adult Nursing. Makalu Publication House. Kathmandu
- Sharma, M. et. al., (2020). Comprehensive Textbook of Medical-Surgical Nursing. Samikshya Publication, Kathmandu
- Cherney, K. and Lia Tabackman, L. (2021). Parkinson’s disease. https://www.healthline.com/health/parkinsons#treatment
- American Association of Neurological Surgeons (n.d). Parkinson’s Disease. https://www.aans.org/en/Patients/Neurosurgical-Conditions-and-Treatments/Parkinsons-Disease
- Tysnes, OB., Storstein, A. (2017, Feb 1). Epidemiology of Parkinson’s disease. Journal of Neural Transmission, 124, 901–905. https://doi.org/10.1007/s00702-017-1686-y
- Beitz, J. M. (2014, Jan 1). Parkinson’s disease: a review. Frontiers in Bioscience (Schol ED), 6(1), 65-74. DOI: 10.2741/s415
- Parkinson’s Foundation. (n.d.) What is Parkinson’s? Retrieved 2023, Feb 6 from https://www.parkinson.org/understanding-parkinsons/what-is-parkinsons