Introduction
Whooping cough is a potentially fatal bacterial infection of the respiratory tract caused by the gram-negative bacterium, Bordetella pertussis. Whooping cough (pertussis) is a highly contagious infection of the lungs and breathing tubes. In many people, it is marked by a severe hacking cough followed by a high-pitched intake of breath that sounds like “whoop.” Other names for whooping cough include pertussis and the “hundred-day cough.”

- Whooping cough can start like a common cold, but unlike a cold, it can last for weeks or months.
- It usually causes prolonged and repeated coughing fits. Coughing fits can last for weeks or even months after noticing the first symptoms of the illness.
- It is an endemic, highly infectious disease that can be prevented with a vaccine. The disease is a leading cause of morbidity and mortality in children.
- The disease has 3 clinical stages, the second and third of which are characterized by an intense paroxysmal cough, an inspiratory whoop, and post-tussive vomiting.
- Pertussis can be prevented by a vaccine that is administered as part of most routine vaccinations and usually started at the age of 6 weeks.
Incidence
- Worldwide 24 million cases occur per year.
- Approximately 161,000 death occurs per year.
- Incidence in the United States: 15,000 cases in 2018.
- Whooping cough is more common in developing countries, with the highest mortality rate in infants (usually no or scant maternal passive immunity unless the mother was given a Tdap booster vaccine in the early third trimester).
- Cases are more common in adolescents as vaccine-induced immunity wears off after 4-12 years.
Causes of Whooping Cough
- The bacteria B. pertussis causes whooping cough.
- It is an airborne disease (via droplets) that spreads easily through infected people’s coughs and sneezes
- When an infected person coughs or sneezes, tiny germ-laden droplets are sprayed into the air and breathed into the lungs of anyone who happens to be nearby.
Risk Factors of Whooping Cough
Risk factors include:
- Pregnancy
- Exposure to an epidemic
- Lack of immunization
- Close contact with an infected individual
- Young infants, particularly those born prematurely
- Patients with underlying cardiac, pulmonary, neuromuscular, or neurologic diseases are also at risk.
Transmission
- Person-to-person contact via aerosolized droplets from a diseased patient’s respiratory secretions
- The disease is contracted by 90% of non-immune household contacts.
- Unvaccinated children are primarily infected by adolescents and adults.
- Elderly siblings with mild to asymptomatic diseases infect infants and young children.
Incubation period
The average time between exposure and the onset of symptoms is 7–14 days (range 6–20 days), with some cases taking up to 42 days.
Signs and Symptoms of Whooping Cough
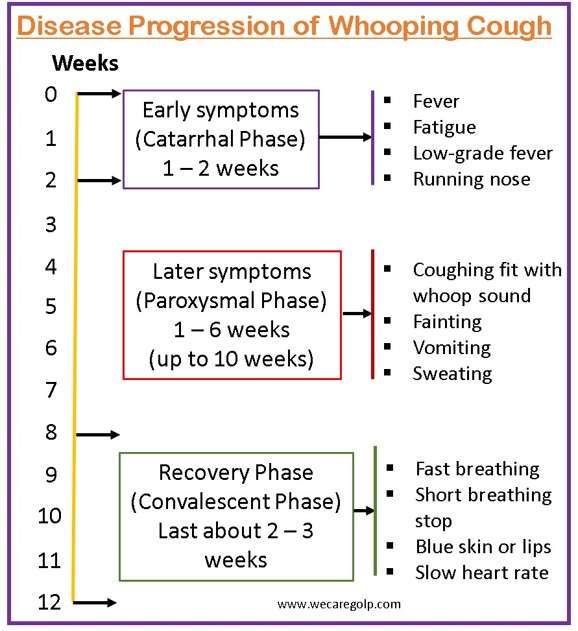
Pertussis infection typically progresses in three stages: catarrhal, paroxysmal, and convalescent.
Catarrhal phase (Early symptoms)
- The catarrhal phase is characterized by
- Fever,
- Fatigue,
- Rhinorrhea (running nose),
- Conjunctival injection,
- Other upper respiratory tract infections.
- The catarrhal phase of the disease lasts one to two weeks and is the most infectious stage.
Paroxysmal phase (Later symptoms)
- The paroxysmal phase follows the catarrhal phase and lasts from one to six weeks (up to 10 weeks).
- It is characterized by
- Staccato cough paroxysms (violent, uncontrolled, rapid, painful coughing fit) and
- Fever resolution.
- These episodes are more common at night and may be triggered by cold or noise.
- Patients appear nontoxic in between paroxysms, but during coughing episodes, they may exhibit
- High-pitched “whoop” sound when they try to inhale after a coughing fit
- Post-tussive emesis (vomiting after coughing)
- Syncope (fainting)
- Cyanosis (blue or grey skin or lips due to lack of oxygen in the blood)
- Diaphoresis (excessive sweating)
- Apnea (temporal cessation of breathing)
- Urinary incontinence (poor bladder control).
- The patient usually feels fine between spells.
Convalescent phase (Recovery Phase)
- A residual cough can last for weeks or months, usually after being exposed to another upper respiratory infection or irritant.
- In infants, atypical presentations are common, and fever may not occur.
- The possible signs and symptoms are
- Tachypnea (fast breathing)
- Apnea
- Cyanosis
- Episodic bradycardia (slow heart rate).
Pathophysiology of Whooping Cough
- Infection is caused by inhaling B. pertussis-containing airborne droplets.
- Bacteria adhere to and damage the ciliated epithelium of the nasopharynx, causing mucociliary elevator inhibition (which may spread to the bronchial tree and lungs in severe cases).
- Bacteria can also evade intracellular digestion and thus invade the host’s immune system.
- Virulence factors (for example, tracheal cytotoxin, dermonecrotic toxin, and adenylate cyclase) cause cilia inflammation and destruction.
- Inflammatory exudate secretion into the respiratory tract (RT) impairs the removal of mucus and debris from the RT resulting in an increased risk of secondary infections.
- Organisms have been discovered in alveolar macrophages as well as the ciliated respiratory epithelial cells of the lower respiratory tract, which may explain the prolonged duration of the cough.
- The pertussis toxin is responsible for most of the systemic manifestations associated with whooping cough (e.g., lymphocytosis, pulmonary hypertension).
Diagnosis of Whooping Cough
History
- Possible exposure to other “whooping cough” cases and vaccination (because the vaccine does not provide complete protection, pertussis should be considered even in vaccinated children!)
Physical Examination
- A physical examination will be carried out by a healthcare professional.
- Sometimes there is a mild fever.
- There may be subconjunctival and petechial hemorrhages on the upper body.
- Typically, chest auscultation is normal.
Laboratory Tests
- Nasopharyngeal swab for culture (gold standard)
- A complete blood count shows nonspecific lymphocytosis.
- Serology testing can be done several weeks after symptoms first appear. A two-fold increase in pertussis antibody titer is diagnostic.
- Polymerase chain reaction (PCR) analysis is most accurate when performed within the first three to four weeks of coughing. A PCR test looks for genetic material from the whooping cough bacteria in your fluid sample. The results could be ready in as little as two hours.
Chest X-ray
- It may also be taken to look for inflammation or fluid in the lungs, which can occur when pneumonia complicates pertussis and other respiratory infections.
Treatment of Whooping Cough
- The primary goal of antibiotic treatment is to reduce disease carriage and spread.
- Because whooping cough is a bacterial infection, antibiotics are used to treat it. When given in the early stages of the disease, they are most effective in reducing the severity of whooping cough.
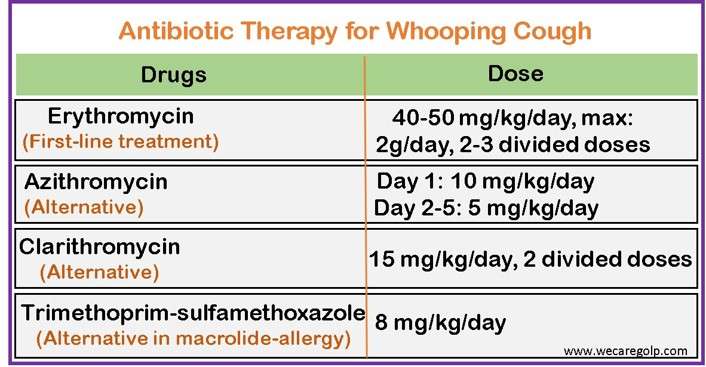
- The macrolides are not recommended for infants younger than 4 weeks old due to the risk of infantile hypertrophic pyloric stenosis.
- It may be advised that family members of someone who has whooping cough take antibiotics to avoid contracting the disease and spreading it to others.
Supportive Care
Further whooping cough treatment is supportive and focuses on making the patient comfortable. It includes
- Bed rest
- Smaller, more frequent meals
- Thick mucus can be removed with saline nose drops.
- Maintaining adequate fluid intake to avoid dehydration (clear fluids are preferred).
- The use of a humidifier to warm and moisten the air may aid in the soothing of the airways and the reduction of coughing spasms.
- Sitting in a steamy bathroom with the child can also be beneficial.
- Cough suppressant medications are ineffective in the treatment of whooping cough.
Hospital Management
- In the most severe cases of whooping cough, hospitalization may be required.
- This is most needed in infants under the age of six months, with approximately 75% of those affected in this age group requiring hospitalization.
- Management in the hospital may include:
- Oxygen administration
- Suctioning mucus and secretions
- Fluid administration via a drip in the hand or arm to prevent dehydration
- Watch for signs of complications
- Separation from other children to prevent disease transmission
Complications of Whooping Cough
Strenuous coughing is linked to several pertussis complications.
- Broken or fractured ribs
- Abdominal hernias
- Cerebral hemorrhages
- Broken blood vessels in the sclera portion of the eyes
- Pneumonia
- Pulmonary hypertension
- Ear infections
- Seizures
- Weight loss
- Dehydration
In infants older than 6 months, complications are frequently more severe and can be fatal. These include
- Pneumonia
- Slowed or stopped breathing
- Dehydration or weight loss as a result of feeding difficulties
- Seizures
- Encephalopathy (brain damage)
Prevention of Whooping Cough
- Wash your hands frequently with soap and water. If soap and water are not available, use an alcohol-based hand sanitizer.
- Avoid touching the face with dirty hands.
- Clean and disinfect frequently touched surfaces, including toys.
- Use a tissue or upper shirt sleeve to cover coughs and sneezes rather than the hands.
- Avoid close contact with sick people.
Vaccination
Getting vaccinated is the most effective way to avoid whooping cough.
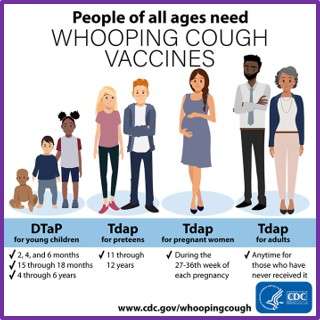
- DTaP is the recommended pertussis vaccine for infants and children. This protects children from three diseases: diphtheria, tetanus, and whooping cough (pertussis).
- DTaP shots are administered at the ages of 2, 4, and 6 months. Boosters are also given at 15 to 18 months and 4 to 6 years of age to maintain protection.
- Children aged 7 to 10 who have not been fully immunized with DTaP should receive the Tdap (with a lower concentration of diphtheria and tetanus toxoid) vaccine, which protects against diphtheria, tetanus, and whooping cough (pertussis).
- Preteens who go to the doctor for their regular checkup at 11 or 12 years old should get a Tdap booster shot.
- Adults aged 19 and up who have not received a Tdap vaccine require a booster shot.
- Adults should receive tetanus and diphtheria (Td) booster shots every 10 years. They should also replace one of the boosters with a Tdap vaccine. Tdap can be given earlier than the 10-year interval.
- If adults spend any time with infants, they must be up-to-date on their pertussis-containing vaccines. Parents, grandparents, siblings, babysitters, relatives, and friends are all included.
- Pregnant women should get Tdap in the third trimester of every pregnancy to pass immunity to their newborn until the baby is old enough to start shots at 2 months.
- Before traveling, travelers should be up-to-date on their pertussis vaccines. Whooping cough is found all over the world.
- If they have not already, healthcare workers who have direct contact with patients should get a single dose of Tdap.
Prognosis
- Most people infected with pertussis will recover completely, although after a months-long illness.
- Infants and older adults have the highest mortality and morbidity rates.
- The infant death rate is about 2% of cases and accounts for 96% of pertussis deaths.
- Morbidity in older adults is higher due to other chronic medical conditions as well as an increased rate of complications, such as pneumonia.
- Some patients may develop secondary complications such as pneumonia, seizures, or encephalopathy.
Whooping Cough Vaccine and Pregnancy
- Pregnant women are not at risk from pertussis vaccines.
- To boost their protection against whooping cough, they should receive the whooping cough vaccination between 20 and 32 weeks of pregnancy.
- Getting vaccinated at this stage of pregnancy ensures that the mother passes on whooping cough antibodies to her growing child.
- This protects the baby after birth, even before they are old enough to be immunized.
- A combination vaccine against diphtheria, tetanus, and whooping cough is recommended for every pregnancy, from 20 to 32 weeks gestation, and at any time up to delivery. The newborn may not be adequately protected if the vaccine is administered within two weeks of birth.
Summary
- Pertussis is a highly contagious, acute respiratory tract infection.
- It is of concern because rates of infection continue to increase.
- Pertussis spreads easily from person to person, mainly through droplets produced by coughing or sneezing.
- The disease is most dangerous in infants and is a significant cause of disease and death in this age group.
- Prevention, correct diagnosis, and prompt treatment of pertussis are essential components of infection management.
- Vaccination is a critical aspect of infection prevention. Herd immunity also greatly aids in the reduction of infection and transmission among people of all ages, particularly infants.
References
- Polinori, I., & Esposito, S. (2019). Clinical findings and management of pertussis. Pertussis Infection and Vaccines, 1183, 151-160. https://doi.org/10.1007/5584_2019_410
- Decker, M. D., & Edwards, K. M. (2021, Oct 1). Pertussis (whooping cough). The Journal of Infectious Diseases, 224(4), S310-S320. https://doi.org/10.1093/infdis/jiaa469
- Lauria, A. M., & Zabbo, C. P. (2022, Jan). Pertussis. StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK519008/
- Fry, N. K., Campbell, H., & Amirthalingam, G. (2021). JMM Profile: Bordetella pertussis and whooping cough (pertussis): still a significant cause of infant morbidity and mortality, but vaccine-preventable. Journal of Medical Microbiology, 70(10). https://doi.org/10.1099/jmm.0.001442
- Forsyth, K. D., Tan, T., von König, C. H. W., Heininger, U., Chitkara, A. J., & Plotkin, S. (2018, Nov 19). Recommendations to control pertussis prioritized relative to economies: A Global Pertussis Initiative update. Vaccine, 36(48), 7270-7275. DOI: 10.1016/j.vaccine.2018.10.028 .
- Nieves, D. J., & Heininger, U. (2016, Jun). Bordetella pertussis. Emerging Infections 10, 311-339. https://doi.org/10.1128/9781555819453.ch17
- Cleveland clinic. (2023, Jan 6). Whopping cough (pertussis). Retrieved on 2023, Feb 10 from https://my.clevelandclinic.org/health/diseases/15661-whooping-cough-pertussis


You’re doing a splendid job
Keep going
Thank you. Please follow us on Facebook at “https://www.facebook.com/wecaregolp” for the coming update!