Introduction
Influenza (Flu) is a severe, extremely contagious viral respiratory infection that is mostly brought on by the influenza virus. Influenza viruses are members of the Orthomyxoviridae RNA virus family and are divided into influenza A, B, C and D based on their main antigenic distinctions. A wide range of animal species, in addition to humans, are infected by influenza, while some influenza strains are species-specific, emerging strains have the potential to spread from other animals to people.
- The nose, throat, bronchi, and occasionally lungs are the main areas affected, but other organs like the heart, brain, and muscles can also be affected.
- With pandemics, epidemics, or seasonal patterns, it occurs all over the world and significantly increases morbidity and mortality.
- Flu epidemics occur yearly in the fall and winter in temperate regions, resulting in severe morbidity and mortality.
- These viruses are spread by respiratory droplets that are expelled from the mouth and respiratory system when someone coughs, talks, or sneezes.
- To become infected, close contact (1 m) is frequently required.
- Although most people recover after a few days. Influenza can cause complications and even result in death, especially in high-risk populations, including pregnant women and those with preexisting medical conditions.
Incidence
- Influenza can strike at any time of year in tropical regions.
- According to the WHO, annual influenza epidemics cause between 250,000 and 500,000 deaths and 3-5 million episodes of serious illness globally.
- The frequently reported number of 36,000 annual flu-related deaths was taken from years when the prevalent virus subtype was H3N2, which tends to be more deadly than H1N1 (according to CDC).
- As of early January 2020, there had been 55,000 influenza-related hospitalizations reported during the 2019–2020 flu season, and 2900 deaths that could have been caused, including 27 pediatric fatalities, had also been reported.
Incubation period
- The incubation time is between 24 and 48 hours.
- About 72 hours after first coming into contact with the virus, symptoms start to show, and an infected individual is contagious for three days.
- It is typically a self-limiting illness that lasts between two and seven days.
Types of Influenza Virus
There are four subtypes of seasonal influenza viruses: A, B, C, and D: Each year, influenza A and B outbreaks occur.
Influenza A viruses
- Influenza A viruses are further divided into subtypes based on how the two proteins on the surface of the virus—hemagglutinin (HA) and neuraminidase (NA)—combine.
- There are 18 different HA subtypes named H1 to H18.
- There are 11 different NA subtypes named N1 to N11.
- Subtypes A (H1N1) and A (H3N2) are now present in humans.
- Only influenza A viruses have been known to cause pandemics.
Influenza B viruses
- Lineages can be used to categorize influenza B viruses rather than subtypes.
- Currently circulating two lineages of influenza type B viruses are B/Yamagata and B/Victoria.
Influenza C virus
- Because the influenza C virus is less frequently found and typically only causes minor infections, it is not of significant public health concern.
Influenza D viruses
- Influenza D viruses are known to primarily infect cattle; they are not known to infect or afflict humans.
Causes of Influenza
- The causative organism is the influenza virus.
- The most prevalent forms that humans contract are A, B, and C. With more severe symptoms, types A and B are seasonal (most cases occur in the winter).
- The number of occurrences remains roughly constant throughout the year, and influenza C does not have particularly severe symptoms or a seasonal pattern.
- Types A and B are often responsible for most flu epidemics and outbreaks, with type C typically inflicting intermittent, minor upper respiratory symptoms.
Risk Factors of Influenza
The risk of contracting the flu or its consequences may be impacted by the following factors.
Age
- Children under the age of two and people over the age of 65 typically experience worse outcomes from seasonal influenza.
Conditions of living or employment
- Individuals are more susceptible to the flu if they reside or work in settings with a high population of inmates, such as nursing homes or military barracks.
- Also, those who are hospitalized are more vulnerable.
A weakened immune system
- The immune system can be compromised by HIV/AIDS, blood cancer, organ transplants, anti-rejection drugs, long-term steroid usage, and cancer therapies.
- This might make it easier to get the flu and raise the possibility of complications.
Chronic conditions
Chronic illness enhances the risk of complications.
- Asthma and other lung ailments
- Diabetes
- Heart disease and stroke
- Brain disorders
- Metabolic disorders
- Chronic kidney disease
- Liver disease
Race
- Those who identify as American Indians or Alaska Natives may be at higher risk for influenza complications.
Using aspirin before age 19
- People under the age of 19 who take long-term therapy with aspirin are at risk of developing Reye’s syndrome if they catch influenza.
Pregnancy
- Pregnant women are more likely to experience influenza-related complications, particularly in the second and third trimesters.
- This threat persists for up to two weeks following the birth of the baby.
Obesity
- A higher body mass index (BMI) increases the likelihood of flu complications in a human.
Mode of Transmission of Influenza
Droplet transmission
- The spread of flu in the air by droplet particles (>10 m) released by an infected host (such as while coughing) and depositing either directly on mucosal membranes or by inhalation.
- Inhalation is the most likely way for an infectious virus particle to get to its target cell.
Bioaerosol transmission
- The spread of influenza through the air by respirable droplet nuclei (10 m).
- Particles enter the lung from a distance and start an infection there.
Contact transmission
- Direct Contact: Physical touch that directly transmits the virus, such as kissing.
- Indirect contact. Transmission via an intermediary object, such as a fomite.
Signs and Symptoms of Influenza
The flu’s symptoms typically appear suddenly and can include:
- Fever
- Chills
- Body pains
- Cough
- Frontal or retro-orbital headache
- Painful throat
- Runny or congested nose
- Red watery eyes
- Feeling drained or worn out
- Vomiting or diarrhea (usually only in kids).
Pathophysiology of Influenza
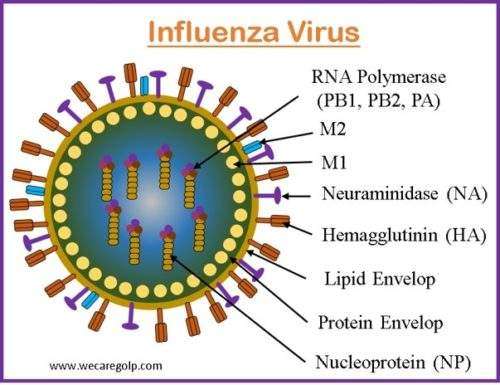
- The Orthomyxoviridae family of viruses includes enclosed, single-stranded, negative-sense influenza viruses.
- Inflammation of the upper respiratory tract and trachea is caused by influenza, an acute illness that affects the upper respiratory system.
- Beginning at the time of inoculation and reaching a peak, on average, within 48 hours, the virus replicates in the upper and lower respiratory passages.
- The three different influenza viruses—influenza A, influenza B, and influenza C—can be identified by their core nucleoproteins (IAV, IBV, and ICV).
- The components of pathogenicity known as hemagglutinin and neuraminidase are important targets for the neutralizing antibodies of acquired immunity against influenza.
- By attaching to respiratory epithelial cells, hemagglutinin promotes cellular infection.
Neuraminidase breaks the connection, securing freshly duplicated virions to the cell surface, and allowing the infection to spread. - The capacity of a particular hemagglutinin to bind to various sialic acid receptors on respiratory tract epithelial cells accounts in part for the species specificity of influenza strains.
Diagnosis of Influenza
The evaluation of an influenza patient includes:
History
- Presence of respiratory symptoms
- History of the patient’s past travel experiences, if any.
Physical examination
- Auscultate the lung fields for the presence of wheezes, crackles (rales), rhonchi, or decreased breath sounds
- Evaluate the respiratory state for rate, depth, ease, use of accessory muscles, and work of breathing.
Rapid influenza diagnostic tests (RIDTs)
- RIDTs are immunoassays that can qualitatively display the results (positive vs. negative) of detecting influenza A and B viral nucleoprotein antigens in respiratory specimens.
Viral culture
- To identify the influenza A virus subtypes and influenza A and B virus strains that are contagious and to keep track of emerging virus strains, some respiratory samples must be collected for viral culture.
- Viral culture can assist in determining additional causes of disease during epidemics of influenza-like illness.
Immunofluorescence assays
- It detects antigens using a fluorescent microscope and can produce results with moderate sensitivity and high specificity in 2-4 hours.
- It is possible to identify influenza A and B viral antigens in respiratory tract specimens using both direct and indirect fluorescent antibody (DFA and IFA) staining tests.
Polymerase chain testing
- The only in vitro diagnostic test for influenza that has been approved by the FDA for use with samples from the lower respiratory tract is RT-PCR (reverse transcription polymerase chain reaction) testing of nasopharyngeal throat secretions.
Serologic testing
- Many serologic tests have become available to avoid the costly and time-consuming problem of culturing, 30–60 minutes are needed to complete the test’s various phases.
Chest radiography
- It is used to rule out pneumonia in elderly or high-risk patients who have pulmonary symptoms.
- With avian influenza, pulmonary infiltrates are seen in nearly all patients; the radiographic features range from diffuse or patchy infiltrates to lobar multilobar consolidation.
Treatment/Management of Influenza
Reducing morbidity and avoiding complications are the main objectives of influenza treatment.
Symptomatic Treatment
Taking care of flu symptoms will not make the illness go away faster, but it will make you feel better.
- Rest until the flu is completely gone, particularly if the sickness is severe.
- Prevent dehydration by drinking enough fluids.
- Fever, headaches, and muscle aches can all be treated with acetaminophen (Tylenol).
- Most of the time, coughs go away on their own, so cough medications are rarely beneficial.
Antiviral Therapy
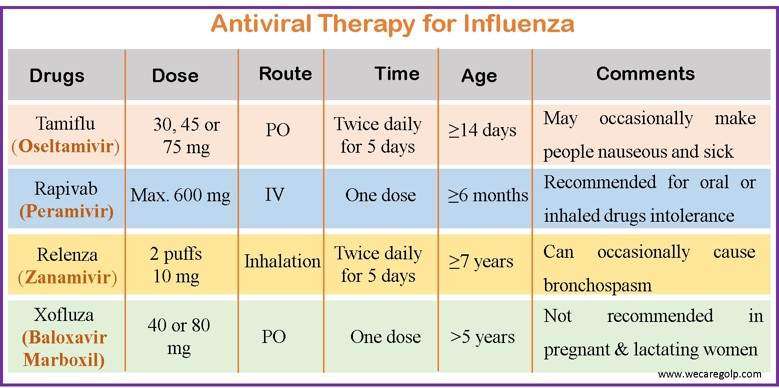
- Influenza can be treated or prevented with antiviral medications.
- The medication can lessen the intensity and length of flu symptoms, but it does not cure them when used as a treatment.
- Antiviral drugs are most effective in the first 48 hours after seasonal flu symptoms appear.
- The CDC advises using four influenza antiviral medications approved by the FDA to treat recently circulating influenza viruses.
Complications of Influenza
The possible complications of influenza include
- Pneumonia is an inflammation of the lungs. Primary influenza Viral pneumonia develops within 24 to 36 hours of the onset of flu symptoms and is unresponsive to antibiotic treatment. Secondary bacterial pneumonia usually appears after a period of recovery from the flu. With medication, people with this kind of pneumonia typically recover.
- Bronchiolitis is an inflammatory condition affecting the tiny airways (bronchioles). Infants are most commonly affected by bronchiolitis, which is the most devastating lower respiratory infection.
- Sinusitis is a condition in which the mucous membranes lining the sinuses of the face and the nose become infected or swollen.
- An increase in the severity of chronic obstructive pulmonary disease (COPD)
- Myocarditis, myositis, and pericarditis
- Dehydration
- Ear infections
- Deterioration of chronic medical illnesses such as diabetes, asthma, and lung and heart disorders.
Prevention of Influenza
Vaccination
- Being vaccinated every year is the best method you can use to protect yourself from the flu.
- Influenza vaccine protects against the following viruses
- Influenza A(H1N1) virus
- Influenza A(H3N2) virus
- Influenza B/Victoria lineage virus
- Influenza B/Yamagata lineage virus
- Other flu viruses similar to influenza viruses (antigenically)
- The ideal time to receive the vaccination is in October or November.
- All individuals 6 months of age and older are advised to have a standard annual influenza vaccination, preferably prior to the commencement of influenza activity in the community
- The two most common influenza vaccines are:
- Inactivated influenza Vaccines (IIV)
- Live, attenuated influenza (LAIV)
Inactivated influenza Vaccine (IIV)
- It may be administered either intramuscularly or topically. The flu vaccine administered intramuscularly is safe for anyone older than 6 months, including healthy individuals and those with ongoing medical issues.
- The age range for the subcutaneous flu vaccination is between 18 and 64.
Live, attenuated influenza vaccine (LAIV)
- The live, weakened flu viruses used in the nasal spray vaccine, also known as LAIV do not actually cause the flu.
- Healthy individuals between the ages of 2 and 49 who are not pregnant may use LAIV.
Recommendation for influenza vaccine
Those who are more likely to develop significant influenza complications, as well as those who live with or provide care for high-risk patients, should get vaccinated against the flu. WHO advises annual immunization for
- Nursing home residents (the elderly or crippled)
- Elderly people
- Anyone with chronic illnesses lasting longer than six months
- Children between the ages of 6 months and 2 years old
- Pregnant women
- Healthcare professionals
- Who perform crucial societal roles.
Other Preventive Measures
- Good personal hygiene and health practices like not touching your eyes, nose, or mouth.
- Frequent hand washing (with soap and water or with alcohol-based hand rubs)
- Covering coughs and sneezes
- Avoiding close contact with sick people and staying at home if you are ill are all reasonable and effective ways to reduce the spread of influenza.
- Face masks may help prevent transmission when caring for the sick.
- Since it can spread through aerosols and direct contact with contaminated surfaces, cleaning surfaces with alcohol, a powerful disinfectant against influenza viruses is recommended.
- In hospitals, rooms or equipment that have been inhabited by patients with influenza symptoms need to be sanitized using quaternary ammonium compounds and bleach.
Prognosis
- The prognosis for patients who catch seasonal influenza without having a concomitant illness is excellent.
- Although complete healing usually requires one to two weeks and most patients recover completely.
- Some people take longer to heal and endure weeks of weakness and exhaustion.
- Infants and the elderly are most at risk of seasonal influenza-related mortality.
- In high-risk individuals, pneumonia brought on by the flu and other influenza-related illnesses is a major cause of morbidity or mortality.
- In these patients, prompt antiviral treatment can lessen the likelihood of lower respiratory illness and hospitalization.
- The case fatality rate is low (e.g., less than 1%), but because the prevalence of illness is high, the overall death toll can be substantial.
- Patients over 65 years old are thought to account for more than 80% of fatalities during typical seasonal influenza epidemics and had the highest rates of hospitalization and death.
Summary
- Influenza is a highly contagious airborne infection that occurs in seasonal epidemics and presents as an acute febrile sickness with varying degrees of systemic symptoms. It is one of the most prevalent infectious diseases.
- The virus can be spread through direct contact with an infected person’s nasal secretions and inhaling droplets released by an infected person when they cough or sneeze.
- Chills are a common sign of influenza, which is then frequently accompanied by fever, headache, sore throat, cough, runny nose, and other symptoms of illness.
- The best way to prevent it is to receive an annual flu shot.
- Relaxation, plenty of water, and avoiding strenuous activity can all aid in recovery, as can taking painkillers, decongestants, and occasionally antiviral medications.
References
- Boktor, SW., Hafner, JW. (2022, Jul 18). Influenza. StatPearls Publishing. Retrieved on 2023, March 3 from https://www.ncbi.nlm.nih.gov/books/NBK459363/
- Centers for Disease Control and Prevention. (2022, October 24). Influenzae (Flu). Retrieved on 2023, March 8 from https://www.cdc.gov/flu/about/keyfacts.htm
- Hien, H. (2022, October 31). Influenza. Medscape. Retrieved on 2023 March 7 from https://emedicine.medscape.com/article/219557-overview
- Hayden, FG., Sugaya, N., Hirotsu, N. (2018). Baloxavir marboxil for uncomplicated influenza in adults and adolescents. N Engl J Med, 379, 913-923. doi:10.1056/NEJMoa1716197
- Gaitonde, D. Y., Moore, F. C., & Morgan, M. K. (2019). Influenza: Diagnosis and Treatment. American family physician, 100(12), 751–758. PMID: 31845781
- Ryu, S., & Cowling, B. J. (2021). Human Influenza Epidemiology. Cold Spring Harbor perspectives in medicine, 11(12), a038356. https://doi.org/10.1101/cshperspect.a038356
- Boktor, SW., Hafner, JW., Doerr, C. (2022). Influenza (Nursing). StatPearls Publishing, Retrieved on 2023, March 7 from https://europepmc.org/article/NBK/nb