Introduction
Chronic kidney disease (CKD) is a long-term disease marked by gradual and permanent kidney deterioration that impairs kidney function over time.
- The National Kidney Foundation defines chronic kidney disease (CKD) as either kidney damage or a persistent decline in kidney function lasting at least three months. Glomerular filtration rate (GFR), a measurement of how well the kidneys are removing waste from the blood, is frequently used to assess kidney function.
- Renal impairment or an estimated glomerular filtration rate (eGFR) of less than 60 ml/min per 1.73 square meters that persists for at least three months are both considered to be signs of chronic kidney disease (CKD). Kidney function gradually declines in CKD, eventually requiring therapy with a kidney replacement (dialysis or transplantation).
- The characteristics of CKD that may indicate a loss of functional nephrons are
- Persistent urine abnormalities
- Structural abnormalities
- Impaired excretory renal function
- Most CKD patients have a higher risk of death and cardiovascular disease.
Incidence
- Around 15% of people in the United States have CKD, and millions more are at higher risk of acquiring it, according to the Centers for Disease Control and Prevention (CDC).
- According to the Global Burden of Disease research, there were 697.5 million instances of chronic kidney disease (CKD) globally in 2020, an increase of 29.3% since 1990.
- It affects elderly persons more often.
- Also, those who have risk factors like diabetes and high blood pressure are more likely to experience it. CKD is thought to be prevalent in about 40% of patients with diabetes. The incidence of CKD among those who have hypertension is predicted to be approximately 20-30%
- CKD caused 2,968,600 (1% of disability-adjusted life years) and 2,546,700 (1% to 3%) life years lost globally in 2012.
Classification of Chronic Kidney Disease
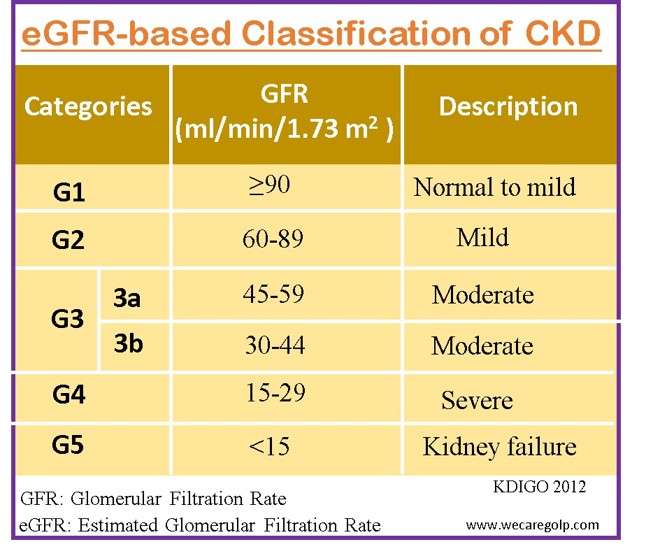
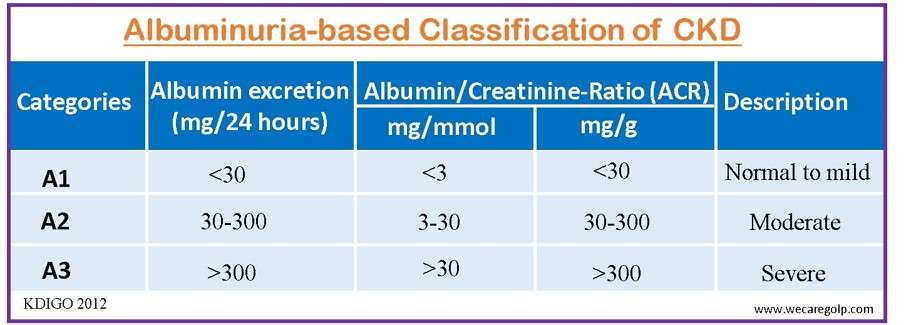
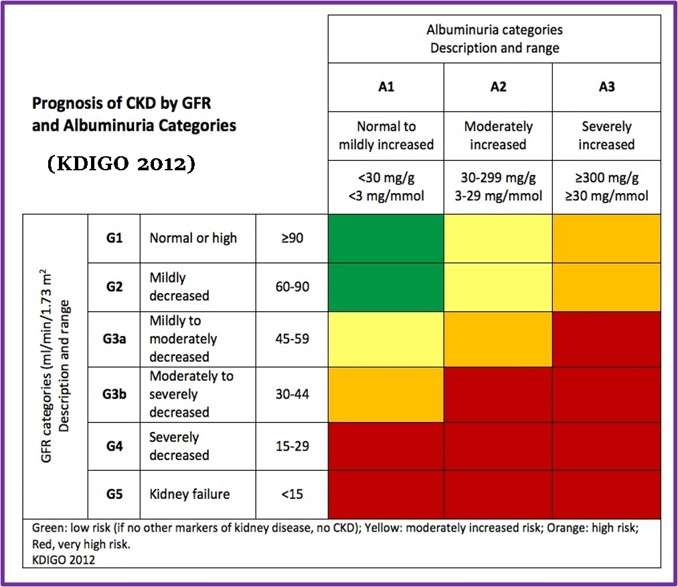
The classification of CKD is based on the estimated glomerular filtration rate (eGFR) and the amount of proteinuria, and it aids in the risk stratification of patients.
Patients are categorized as G1-G5 based on eGFR and A1-A3 based on ACR (albumin-to-creatinine ratio).
eGFR-based classification
Albuminuria/proteinuria-based classification:
This classification uses the level of albumin or protein in the urine to stage CKD into three categories.
Combination-based classification:
The classification that combines estimated glomerular filtration rate (eGFR) and albuminuria/proteinuria levels to stage chronic kidney disease (CKD) into five categories is called the Kidney Disease Improving Global Outcomes (KDIGO) classification. The five stages are:
- G1: eGFR ≥ 90 mL/min/1.73 m² with A1
- G2: eGFR 60-89 mL/min/1.73 m² with A1 or A2
- G3a: eGFR 45-59 mL/min/1.73 m² with A1 or A2
- G3b: eGFR 30-44 mL/min/1.73 m² with A1, A2, or A3
- G4-G5: eGFR < 30 mL/min/1.73 m² with A1, A2, or A3
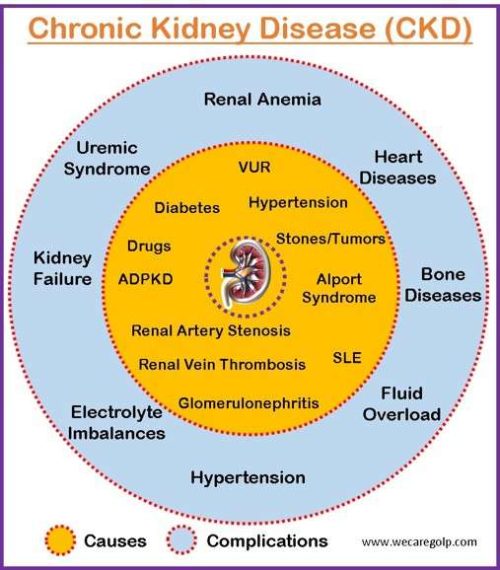
Causes of Chronic Kidney Disease
- Diabetes mellitus (leading cause)
- Hypertension
- Glomerulonephritis:
- Primary glomerular disease
- Membranous nephropathy
- Immunoglobulin A (IgA) nephropathy
- Focal and segmental glomerulosclerosis (FSGS)
- Minimal change disease
- Membranoproliferative glomerulonephritis (MPGN)
- Postinfectious glomerulonephritis (PIGN)
- Rapid progressive glomerulonephritis (RPGN)
- Secondary glomerular disease
- Rheumatoid arthritis
- Mixed connective tissue disease
- Scleroderma
- Primary glomerular disease
- Vascular diseases
- Renal artery stenosis
- Atheroemboli
- Hypertensive nephrosclerosis
- Renal vein thrombosis
- Inherited kidney diseases
- Autosomal dominant polycystic kidney disease (ADPKD)
- Alport syndrome
- Kidney cysts
- Congenital defects of the kidney or bladder
- Renal agenesis (only one kidney)
- Renal hypoplasia (small kidneys)
- Renal dysplasia (abnormally formed kidney)
- Horseshoe kidney (kidneys fused together)
- Vesicoureteral Reflex (VUR)
- Duplicated ureter
- Autoimmune diseases
- Systemic lupus erythematosus (SLE)
- Morbus Wegner
- Tubulointerstitial
- Multicystic dysplastic kidney (MCDK)
- Juvenile nephronophthisis
- Chronic interstitial nephritis
- Posterior urethral valves (PUV)
- Obstructive uropathy (blockage of the urinary tract)
- Drug-induced nephrotoxicity (damage to the kidneys caused by medications)
- Paracetamol
- Phenacetin
- Non-steroidal anti-inflammatory drugs (NSAIDs),
- Recurrent renal stone
- Unrecovered acute kidney injury
- Other multiple risk factors or comorbidities
- Obesity
- Recurring infections
- Smoking
- Aging
Signs and Symptoms of Chronic Kidney Disease
Stage 1 to Stage 3 (Early stage)
- Often asymptomatic
- Mild fatigue
- Mild decrease in appetite
- Increased need to urinate
- Trouble sleeping
Advanced Stages (Stage 4 to Stage 5)
- Nausea and vomiting
- Loss of appetite (anorexia)
- Oliguria, anuria, hematuria
- Fatigue and weakness
- Decreased mental sharpness
- Muscle twitches and cramps
- Swelling in feet and ankles
- Persistent itching
- Protein-energy malnutrition
- Loss of lean body mass
- Muscle weakness
- Skin disorder: Dry skin, pruritus, ecchymosis
- Increased somnolence
- Failure to thrive
- Pericardial friction rub-uremic pericarditis
- Uremic frost
- High blood pressure
- Shortness of breath
- Abnormal heart rhythms
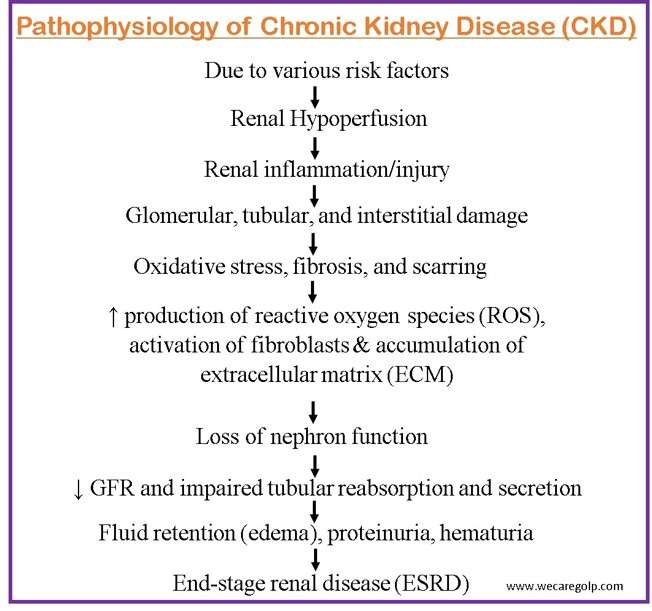
Pathophysiology
- The presence of risk factors such as diabetes, hypertension, obesity, smoking, and family history is the initial step in the pathophysiology of CKD. Several risk factors can induce chronic kidney damage, resulting in renal hypoperfusion, or decreased blood flow to the kidneys.
- This can be caused by several factors, including poor autoregulation of renal blood flow, activation of the renin-angiotensin-aldosterone system (RAAS), or increased intraglomerular pressure.
- Renal hypoperfusion can result in renal injury and inflammation, which can harm many sections of the kidney, including the glomeruli, tubules, and interstitium.
- Glomerular damage from increasing intraglomerular pressure can result in glomerular sclerosis and proteinuria. Ischemia, toxins, and inflammation can all cause tubular injury, resulting in decreased reabsorption and release of numerous substances such as electrolytes and medicines.
- Interstitial injury can develop as a result of inflammatory cell infiltration and fibrosis buildup, resulting in tubular atrophy and gradual loss of nephron function.
- In CKD, oxidative stress is a significant modulator of kidney damage and inflammation. Elevated reactive oxygen species (ROS) production can cause cell and tissue damage such as lipid peroxidation, protein oxidation, and DNA damage.
- ROS can also activate signaling pathways that are implicated in inflammation, apoptosis, and fibrosis. Moreover, chronic kidney damage can activate fibroblasts, resulting in extracellular matrix (ECM) buildup and the development of interstitial fibrosis.
- When nephron function declines over time, it can cause CKD symptoms such as fluid retention and edema, hypertension, anemia, tiredness, and changes in urine output.
- These symptoms can be caused by several causes, including inadequate salt and water balance management, sympathetic nervous system activation, and decreased erythropoietin production.
- The condition may eventually proceed to end-stage renal disease (ESRD), in which the kidneys are no longer able to work properly enough to preserve life.
- The patient will need renal replacement therapy, such as dialysis or a kidney transplant, at this stage.
Diagnosis of Chronic Kidney Disease
Apart from history taking and physical examination, the following tests can help diagnose chronic kidney disease.
Blood Tests
Blood tests are the most prevalent CKD diagnostic method.
- High levels of serum creatinine and blood urea nitrogen (BUN) levels in the blood generally suggest decreased kidney function.
- Besides serum creatinine and BUN, other tests may include
- Cystatin C
- Phosphate and calcium
- Parathormone
- Erythrocytes, hemoglobin, iron
- Blood gas analysis
- Immunological parameters
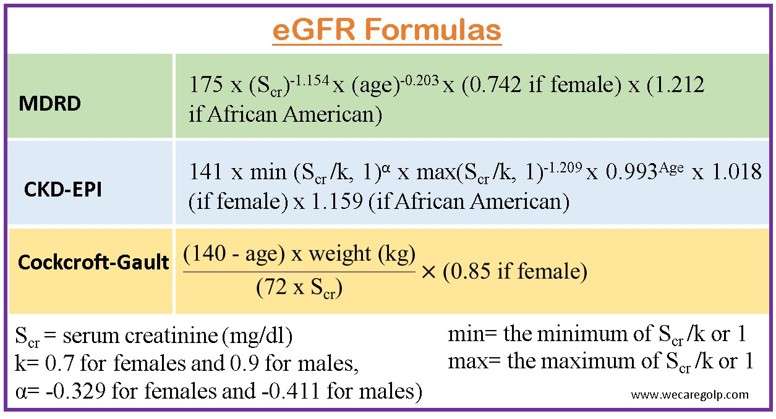
- Estimated glomerular filtration rate (eGFR) examines how efficiently the kidneys filter waste items from the blood. It is calculated using different formulas that consider creatinine level, age, gender, and race.
- Modification of Diet in Renal Disease (MDRD) formula
- CKD Epidemiology Collaboration (CKD-EPI) formula (new and more accurate)
- Cockcroft-Gault formula(not suggested for individuals with varying renal function or poor muscle mass)
Glomerular filtration rate evaluation
- For individuals in whom the difference between AKI and CKD is uncertain, kidney function tests should be repeated in 2 weeks following the initial finding of low eGFR ≤ 60 ml/min/1.73 m.
- CKD is verified if earlier testing demonstrates that the low eGFR is persistent or if repeat blood test findings over 3 months are consistent.
- If eGFR based on serum creatinine is known to be less reliable, additional indicators such as cystatin-c or isotope-clearance testing can be performed.
Assessment of chronicity
- When an eGFR of less than 60 ml/min/1.73m is identified in a patient, the prior blood and urine test results, as well as the clinical history, must be reviewed to identify whether this is the consequence of AKI or CKD that has been present but asymptomatic.
Urine Tests
- Furthermore, urine tests are utilized to identify CKD. The urine test calculates the urine’s protein content.
- Very little protein should typically be present in urine. Nevertheless, protein can leak into the urine if the kidneys are not working properly.
- Proteinuria should be evaluated by collecting an early morning urine sample and calculating the albumin-creatinine ratio (ACR).
- Albuminuria is now classified from A1 to A3 (as described in the classification section) removing prior designations such as microalbuminuria.
Imaging
- Renal ultrasonography is useful for screening for hydronephrosis, which may not be seen in early blockage or dehydrated individuals, or for the involvement of the retroperitoneum with fibrosis, malignancy, or widespread adenopathy; in severe kidney failure, tiny, echogenic kidneys are seen.
- Retrograde pyelography is used to diagnose renal stones and in instances when there is a high suspicion of blockage despite negative renal ultrasonograms.
- CT scan is useful for better defining renal tumors and cysts that are typically shown on ultrasonograms. It is also the most sensitive technique for diagnosing kidney stones.
- Magnetic resonance imaging (MRI) is useful in individuals who need a CT scan but cannot get intravenous contrast; accurate in the detection of renal vein thrombosis.
- Renal radionuclide scan (Renal scintigraphy) evaluates the anatomy and physiology of the kidney using radiopharmaceuticals. It is valuable to detect narrowing structures of the kidney regarding kidney injuries, failure, and transplantation.
Biopsy
- When kidney damage and/or proteinuria approaching the nephrotic range are present and the diagnosis is unresolved after a proper workup, a percutaneous kidney biopsy is often needed.
Treatment of Chronic Kidney Disease
- There is no cure for chronic kidney disease. CKD significantly raises the risk of cardiovascular disease, and people with CKD frequently have other heart disease risk factors, such as hyperlipidemia.
- Therefore, cardiovascular disease is the leading cause of death in CKD patients.
- Aggressive treatment of hyperlipidemia is warranted.
Treatment goals
- Slow or stop the progression of the disease
- Control and treat underlying causes (diabetes, hypertension, etc.)
- Control and treat other risk factors
- Treat complications of the disease
- Replace lost kidney function.
Control of blood glucose
- Maintaining good control of diabetes is critical.
- All diabetes complications, including chronic kidney disease, are significantly more likely to occur in people with diabetes who are unable to control their blood glucose levels.
Control of high blood pressure
- This also slows the progression of chronic kidney disease.
- If you have kidney disease, it is best to keep your blood pressure below 130/80 mm Hg.
- Antihypertensive drugs such as angiotensin-converting enzyme (ACE) inhibitors and angiotensin receptor blockers (ARB) have a unique advantage in protecting the kidneys.
Strategies for slowing the progression and treating conditions underlying CKD include the following:
Diet
Diet control is essential to slowing the progression of chronic kidney disease and should be done in close consultation. The following are general dietary guidelines:
- Protein restriction: The development of chronic kidney disease may be slowed down by reducing protein intake.
- Salt restriction: To prevent fluid retention and aid in blood pressure control, limit consumption of salt intake to 2 to 4 grams per day.
- Fluid intake restriction: Drinking too much water does not prevent kidney disease. Restriction of water intake is usually recommended.
- Potassium restriction: Due to the inability of the kidneys to remove potassium, this is necessary for advanced kidney disease. Heart rhythm problems can occur when potassium levels are too high. Examples of foods high in potassium include bananas, oranges, nuts, mushrooms, lemons, and potatoes.
- Phosphorus restriction: To protect bones, it is recommended to decrease phosphorus intake. Phosphorus-rich foods include dairy products, beans, cola drinks, egg yolks, etc.
- Other important measures that a patient can take include carefully following prescribed regimens to control blood pressure and/or diabetes; stopping smoking; and losing excess weight.
Medications
Angiotensin-converting enzyme inhibitors (ACE-Is):
- ACE Inhibitorsare drugs commonly used in the treatment of hypertension.
- Some commonly used AEC inhibitors (end with pril) are
- Captopril
- Enalapril
- Lisinopril
- Ramipril
- Quinapril
- Trandolapril
- These medications lower blood pressure by lowering angiotensin-II and aldosterone synthesis, two hormones that constrict blood vessels (a hormone that causes sodium retention).
- These medications not only lower blood pressure, but they also have additional effects that slow the evolution of kidney disease, such as lowering glomerular pressure and minimizing kidney scarring.
Angiotensin receptor blockers (ARBs)
- ARBs are medications that stop angiotensin-II from acting on its receptors.
- Like ACE-I, these medications protect the kidneys and delay the onset of renal failure.
- Some of them (end with sartan) are
- Losartan
- Valsartan
- Irbesartan
- Candesartan (Atacand)
- Olmesartan
Diuretics
- Diuretics are used to control edema (swelling), blood pressure, and/or potassium levels.
- Loop diuretics
- Furosemide
- Ethacrynic acid
- Bumetanide
- Torsemide
- Thiazides
- Hydrochlorothiazide
- Indapamide
- Potassium-sparing diuretics
- Spironolactone
- Amiloride
Erythropoiesis-stimulating substances (ESAs)
- Patients with CKD frequently experience anemia called renal anemia because their kidneys are unable to produce enough erythropoietin.
- Procrit (erythropoietin), one of the erythropoiesis-stimulating agents
- ESAs promote the production of red blood cells in the bone marrow, lowering the requirement for blood transfusions.
- Some commonly used ESAs are
- Epoetin alfa (Abseamed, Eprex, Epogen, Procrit)
- Epoetin beta (NeoRecormon)
- Darbepoetin alfa (Aranesp)
- It begins with Hb ≤ 10g/dl and targets 11.5 g/dl (not >13g/dl
- It is advised to aim for a hemoglobin level of 10–12 g/dL for CKD patients.
Phosphate binders
- If the dietary restriction of phosphorus is inadequate to regulate phosphorus levels, patients may begin taking phosphate binders like
- Calcium carbonate (Tums)
- Calcium acetate (PhosLo)
- Lanthanum carbonate (Fosrenol)
- Sevelamer (Renagel, Renvela)
Vitamin D
- Vitamin D insufficiency is a relatively widespread condition.
- Having sufficient stores of vitamin D in the body is the first step in curing metabolic bone disease.
- Activated versions of vitamin D may be provided if renal disease worsens.
- These medications include
- Doxercalciferol
- Paricalcitol
- Calcitriol (Rocaltrol, Zemplar)
- Drisdol
Renal Replacement Therapies
Dialysis or kidney transplantation are the sole options for replacing kidney functions in end-stage renal disease. When chronic renal disease has reached stage 4, preparation for dialysis and transplantation is often initiated.
Dialysis
- Hemodialysis and peritoneal dialysis are the two types of dialysis.
- There are not many distinctions between the two techniques’ results.
- The medical staff will talk with the patient about the best possibilities and assist them in making a choice that will meet both their personal and medical needs.
- It is advisable to select a dialysis modality after learning about both treatments and matching them to one’s lifestyle, daily activities, timetable, proximity to the dialysis facility, support network, and personal preferences.
- Usually, dialysis starts when the eGFR falls under 15 ml/min/1.73 m2. However, it is beneficial to begin earlier before patients have severe symptoms to prevent complications.
Hemodialysis
Hemodialysis (HD) is the most used renal replacement therapy to replace the detoxification and excretion function.
- Vascular access: Hemodialysis requires vascular access so that blood may flow quickly through the dialysis filters to facilitate the removal of wastes, toxins, and extra fluid. The three forms of vascular accesses are
- Arteriovenous fistula (AVF),
- Arteriovenous graft (AVG), and
- Central venous catheters (CVC).
- A dialyzer, which has two fluid compartments and is set up with bundles of hollow fiber capillary tubes, is used in hemodialysis, which includes pumping blood through it.
- Dialysate, the fluid used to clean the blood, is pushed down one side of a semipermeable membrane in a separate compartment, while blood is pumped along the other side in the first compartment.
- Acid concentrate and base component gradients between blood and dialysate cause the necessary changes in blood composition, including a decrease in waste products (urea nitrogen and creatinine), a correction of acid levels, and an equilibrium of different mineral levels.
- Excess water is also eliminated.
- After that, the blood is given back to the body.
Peritoneal dialysis
Peritoneal dialysis (PD) is another type of renal replacement procedure for the treatment of renal insufficiency.
- PD is a procedure to remove waste products (such as creatinine and urea) and extra water through the blood vessels that line the walls of the abdomen when the kidneys are no longer working effectively. The lining of the abdomen called the peritoneum acts as a dialysis membrane.
- This procedure filters the blood in a different way than hemodialysis.
- It does not cure or treat underlying kidney diseases like hemodialysis (HD). However, it is intended to replace as many functions of the failing kidneys as possible.
Kidney Transplantation
- Human kidney transplantation is the preferred treatment for advanced CKD because it provides the greatest results and the highest quality of life. Tens of thousands of these treatments have been carried out globally.
- Living donors, live unrelated donors, or persons who passed away for other reasons can all provide transplanted kidneys (deceased donors). Yet not everybody qualifies for a kidney transplant. To verify that a person is a good candidate for a transplant, they must undergo thorough testing. The finest results are often obtained from transplants from live relatives.
- Age-related mortality rates following transplantation are greatest in the first year and range from 6.8% for people over 50 to 2% for those between 18 and 34.
- After several months of satisfactory function, acute reversible rejection can occasionally happen, especially if the patient doesn’t take the immunosuppressive medications as directed.
- In comparison to dialysis patients, transplantation generally allows the majority of patients to resume an enhanced lifestyle and life expectancy.
Recipient Selection
- Prior to receiving transplantation approval, every applicant must undergo a rigorous risk-versus-benefit analysis. The presence of infection (HIV, Hepatitis B or C, TB), neoplasm, and correctable coronary artery disease diagnosis should all be standard components of the candidate workup.
- Renal transplantation is not always recommended. After five days of surgery, patients who don’t have any postoperative issues are frequently ideal candidates for discharge from the hospital.
- Candidates with diabetes and those who are older have more mortality rate than other transplant recipients.
- Existence of a possibly damaging antibody against the donor’s kidney at the time of the planned transplant is one of a few absolute immunologic contraindications to transplantation.
- Natural antibodies against the ABO blood group antigens and antibodies against the human leukocyte antigen (HLA) Class I (A, B, C) or class II (DR) antigens are harmful antibodies that can result in very early graft loss. These antibodies are routinely excluded by proper screening for ABO incompatibility in the candidate, HLA typing of the donor and recipient, and direct cross-matching of the candidate serum with the lymphocytes of the donor.
Donor Selection
- Live volunteer donors should be in good health and belong to the same major ABO blood type since switching major blood groups reduces the likelihood that the allograft will survive.
- Nonetheless, it is feasible to transplant a kidney from a type “O” donor into a recipient who is an A, B, or AB. Often, family members are chosen as donors who have some HLA antigen compatibility.
- Because the surgical process is challenging and the ischemia period for the transplanted kidney is prolonged when vascular abnormalities occur, selective renal arteriography should be done on donors to rule out the presence of many or aberrant renal arteries.
- Because there is a chance that the receiver will get hepatitis, HIV, or a malignant neoplasm, donors should be screened first.
Complications of Chronic Kidney Disease
Short-term complications
- Fluid overload
- Electrolyte imbalances
- High blood pressure.
- Renal anemia
- Cardiovascular disease (arterial hypertension, left ventricular hypertrophy, coronary artery disease, heart failure, ventricular arrhythmias, accelerated atherosclerosis of the vessels, endocarditis, pericarditis, and strokes)
- Kidney failure (ESRD)
- Uremic syndrome
- Bone disease (renal osteopathy)
- Water imbalances
- Acid-base imbalances (metabolic acidosis)
- Electrolyte imbalances (hyperkalemia, hyperphosphatemia, hypercalcemia)
- Renal anemia
- Malnutrition
- Neurological complications: peripheral neuropathy and encephalopathy.
Prevention of Chronic Kidney Disease
Manage blood sugar levels
- Diabetes is a major cause of CKD.
- Blood sugar control can help prevent or postpone CKD.
- Diabetics should eat a balanced diet, exercise frequently, take their medications as directed, and have their blood sugar levels checked regularly.
Maintain a healthy blood pressure
- High blood pressure is another major cause of CKD.
- Blood pressure control can help prevent or postpone CKD.
- Blood pressure should be checked regularly, and if it is elevated, it should be managed by lifestyle modifications or drugs given by a doctor.
Keep a healthy weight
- Obesity increases the risk of CKD.
- Keeping a healthy weight can help avoid or prevent the onset of CKD.
- A healthy weight may be obtained by following a nutritious diet and engaging in regular exercise.
- Smoking can damage the kidneys and increase the risk of CKD. Quitting smoking can help prevent or delay CKD.
Control cardiovascular disease
- Cardiovascular disorder raises the risk of CKD.
- Treating cardiovascular disease with lifestyle modifications and medicines prescribed by a doctor can help prevent or postpone CKD.
Minimize salt intake
- Excess salt consumption raises blood pressure, which increases the risk of CKD.
- Reducing salt consumption can help prevent or postpone the onset of CKD.
Minimize potassium and phosphate diet
- As kidney disease begins, kidneys cannot eliminate the potassium and phosphate from the body properly. It results in hyperkalemia and hyperphosphatemia.
- Reducing potassium and phosphate intake from early stages can prevent complications.
Avoid nephrotoxic drugs
- Certain medicines might cause kidney damage.
- Avoiding or using nephrotoxic medicines as advised by a healthcare expert can help avoid or postpone CKD.
Drink plenty of water
- Being hydrated can help avoid dehydration, which can harm the kidneys.
- It is critical to keep hydrated by drinking enough water, but not too much, since this might strain the kidneys.
Routine kidney function test
- It helps diagnose CKD early when the disease is more curable.
- Individuals who are at high risk of developing CKD, such as those who have diabetes or high blood pressure, should have their renal function evaluated regularly.
Prognosis
- Depending on the disease’s stage, the underlying cause, and personal characteristics like age and general health, the prognosis for CKD might change.
- Although early stages of CKD (stages 1-3) may not have much of an effect on a person’s lifetime, they nonetheless need to be closely monitored and managed to avoid progressing to more severe stages.
- End-stage renal disease (ESRD), which necessitates dialysis or kidney transplantation to maintain life, is a result of advanced stages of chronic kidney disease (CKD; stages 4-5), which are linked to a higher risk of comorbidities such as cardiovascular disease, anemia, bone disease, and infections.
- Patients with ESRD have a five-year survival rate of about 35%, although this can vary greatly depending on age, comorbidities, and availability of+ therapy. For those with ESRD, kidney transplantation gives the highest long-term survival and quality of life, but not everyone is a candidate.
Summary
- Chronic kidney disease (CKD) is a long-term disorder in which the kidneys get damaged and are unable to function correctly.
- It is a degenerative disease that frequently goes undiagnosed until it is advanced.
- A range of causes, including high blood pressure, diabetes, autoimmune illnesses, and certain drugs, can lead to CKD.
- CKD is classified into five stages, with stage 1 being the mildest and stage 5 being the most severe. There may be few or no symptoms in the early stages, but as the disease advances, symptoms such as fatigue, swelling in the legs and ankles, and changes in urine patterns may arise.
- The goal of CKD treatment is to control symptoms and limit the disease’s development. This may entail taking drugs to regulate blood pressure and blood sugar levels, altering one’s diet to manage electrolyte imbalances, and refraining from taking drugs that may worsen kidney damage. Dialysis or a kidney transplant may be required in extreme circumstances.
- Managing underlying illnesses that raise the risk of kidney damage, such as diabetes and hypertension, and avoiding drugs that might damage the kidneys are key to preventing CKD.
- Maintaining a healthy lifestyle is also crucial. This includes engaging in regular exercise, eating a balanced diet, and quitting smoking. For people who are at risk of developing CKD, routine renal function testing is advised.
References
- Arora, P. (2023, February 10). Chronic Kidney Disease. Medscape. Retrieved 2023, February 26 from https://emedicine.medscape.com/article/238798-overview
- Atkins, R. C. (2005). The epidemiology of chronic kidney disease. Kidney international, 67, S14-S18. https://doi.org/10.1111/j.1523-1755.2005.09403.x
- Centers for Disease Control and Prevention. (2019, April 4). Chronic Kidney Disease Surveillance System. Retrieved 2023, February 26 from https://www.cdc.gov/kidneydisease/surveillance/index.html
- Chen, T. K., Knicely, D. H., & Grams, M. E. (2019). Chronic kidney disease diagnosis and management: a review. Jama, 322(13), 1294-1304. doi:10.1001/jama.2019.14745
- Hill, N. R., Fatoba, S. T., Oke, J. L., Hirst, J. A., O’Callaghan, C. A., Lasserson, D. S., … & Hobbs, F. D. (2016). Global prevalence of chronic kidney disease–a systematic review and meta-analysis. PLOS ONE, 11(7), e0158765. https://doi.org/10.1371/journal.pone.0158765
- KDIGO. (2012). Clinical practice guideline for the evaluation and management of chronic kidney disease. Kidney International Supplements, 3(1), 1-150. https://kdigo.org/wp-content/uploads/2017/02/KDIGO_2012_CKD_GL.pdf
- Levey, A. S., De Jong, P. E., Coresh, J., El Nahas, M., Astor, B. C., Matsushita, K., … & Eckardt, K. U. (2011). The definition, classification, and prognosis of chronic kidney disease: a KDIGO Controversies Conference report. Kidney international, 80(1), 17-28. https://doi.org/10.1038/ki.2010.483
- 8*Vaidya, S. R., & Aeddula, N. R. (2021). Chronic renal failure. StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK535404/
- Webster, A. C., Nagler, E. V., Morton, R. L., & Masson, P. (2017). Chronic kidney disease. The lancet, 389(10075), 1238-1252. https://doi.org/10.1016/S0140-6736(16)32064-5
- Zhong, J., Yang, H. C., & Fogo, A. B. (2017). A perspective on chronic kidney disease progression. American Journal of Physiology-Renal Physiology, 312(3), F375-F384. https://doi.org/10.1152/ajprenal.00266.2016