Introduction
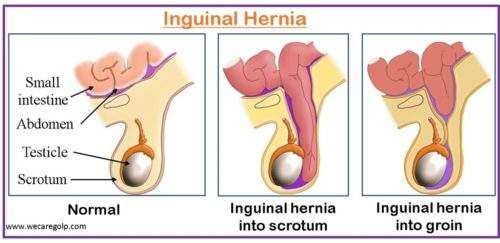
An inguinal hernia (IH) is a hernia (protrusion) of intraabdominal or extraperitoneal organs that occurs through the inguinal canal due to weakness of the lower abdominal muscles like a transverse and oblique muscle.
- The weakening of the lower abdominal muscle makes a hole in the abdominal wall, and some intra-abdominal contents are pushed via this opening into the groin. It could be fat, the bowel, or the genitourinary tract.
- One of the most frequent causes for referring a primary care patient for surgical intervention is inguinal hernias
- The bulge that results might be painful, especially if the patient coughs, bends over, or lifts a heavy object. Many hernias, however, are painless. Not all inguinal hernias are harmful.
- Untreated inguinal hernias can have serious implications, including blocking or strangling the hernia’s contents, which can be lethal.
Incidence
- Of all abdominal wall hernias, inguinal hernias make up 75% of cases. There are two peaks in the occurrence of inguinal hernias, one at age 5 and the other at age 70.
- Men are more likely than women to experience it. Men account for around 90% of all inguinal hernias, whereas females account for approximately 10%.
- Around 25% of males and less than 2% of women will develop an inguinal hernia in their lives.
- In men, the incidence of inguinal hernia ranges from 110 per 100,000 people in the 16-to-24-year age range to 2000 per 100,000 people in the 75 and older age range.
Classification of Inguinal Hernia
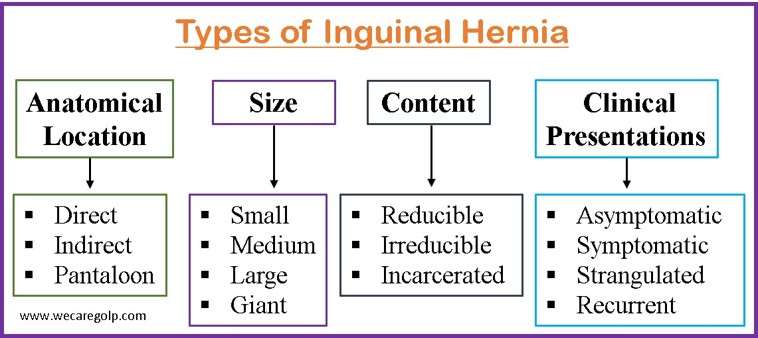
Based on the Anatomical Location
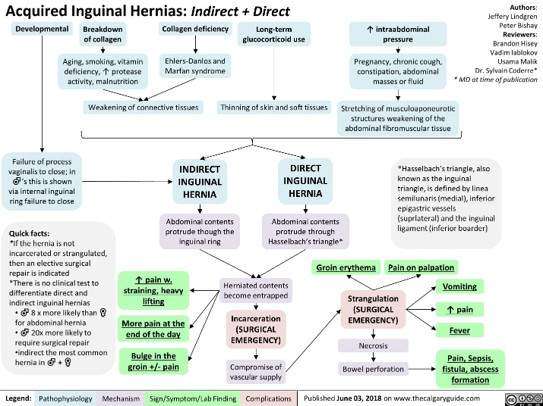
Direct inguinal hernia
- Direct inguinal hernias occur in response to the degeneration of the connective tissue of the abdominal muscles, leading to muscle weakness in adults.
- Fat or the small intestine slides through the weak muscles into the groin, causing a hernia. A direct hernia develops gradually as a result of constant muscular tension.
- This form of hernia arises when abdominal tissue protrudes through a weak place in the abdominal wall in Hesselbach’s triangle, a tiny region of the groin.
- Direct inguinal hernias are more common in elderly persons and are commonly caused by abdominal muscle weakness induced by
- Age
- Excessive lifting
- Chronic coughing
- Peritoneal dialysis (due to dialysis solution)
- Ascites
- Chronic obstructive pulmonary disease (COPD)
Indirect inguinal hernia
- Indirect inguinal hernias are congenital hernias that are substantially more frequent in males than females due to the way males grow in the womb.
- In a male fetus, the spermatic cord and both testicles regularly descend the inguinal canal into the scrotum, the sac that stores the testicles, from an intra-abdominal site.
- Shortly after birth, the inguinal ring’s entry to the inguinal canal does not always close properly, resulting in a weakening of the abdominal wall.
- Fat or a portion of the small intestine can pass through the weakness and into the inguinal canal, resulting in a hernia.
- In a woman, an indirect hernia occurs when the reproductive organs or small intestine protrude into the groin through a weakness in the abdominal wall.
- The most frequent kind of inguinal hernia is an indirect hernia. Premature children are more vulnerable to indirect inguinal hernias because the inguinal canal has less time to close.
Pantaloon hernia
- When both a direct and an indirect hernia develop on the same side of the groin, this condition is known as a pantaloon hernia.
- The pantaloon hernia has its name because the two hernia sacs are separated by epigastric vessels and resemble a pair of pants.
- Since the abdominal tissue protrudes through both Hesselbach’s triangle and the inguinal canal, this hernia is a mix of a direct and an indirect inguinal hernia.
Based on the Size
Small hernia
- Small hernias may move back and forth through the abdominal opening without causing any symptoms.
- It generally has a diameter of less than 1 cm and is often diagnosed accidentally which may not need any treatment unless any complications are present.
Medium hernia
- This type of hernia causes mild pain which is aggravated by physical activity. It generally has a diameter between 1 cm and 3 cm.
- Surgical repair is indicated if there are changes in size causing various complications.
Large hernia
- It has more than 3 cm in diameter and can cause substantial pain, discomfort, and other consequences such as bowel blockage or strangling.
- This hernia necessitates immediate medical care and surgical treatment.
Giant hernia
- This is a rare type of hernia which is massive in size (50 kg).
- Extreme pain, immobility, and other various complications are seen requiring complex surgical repair.
Based on the content
Reducible Hernia
- In this type of hernia. herniated tissue can be pushed back into the abdomen.
- This implies that hernia sac contents, such as small intestine or fatty tissue, can be physically moved back into the abdominal cavity via the hernia hole or defect.
- Reducible hernias are not considered a medical emergency in most cases, but they should be assessed by a doctor to determine if surgery is required to repair the hernia and avoid consequences such as intestinal blockage or strangling.
Irreducible Hernia
- An irreducible hernia cannot be repaired by pushing the herniated tissue back into the abdomen.
- This means the contents of the hernia sac are stuck outside of the abdominal cavity and cannot be decreased manually.
- It can be life-threatening because the trapped tissue can become strangulated and die.
- The following can be shown at the location of the hernia
- Pain
- Swelling
- Discomfort
Incarcerated Hernia
- An incarcerated hernia arises when herniated tissue becomes stuck and cannot be easily repositioned.
- A hernia that has been entrapped might cause intestinal blockage or strangulation.
- A hernia that has been imprisoned is one in which the herniated tissue has become trapped and cannot be reduced.
- This indicates that the contents of the hernia sac are stuck outside the abdominal cavity and cannot be pulled back in.
- It can cause intestinal blockage, a medical emergency that needs rapid treatment to avoid tissue death.
- Symptoms may include
- Pain
- Nausea and vomiting
- Inability to pass gas or have a bowel movement
Based on the Clinical Presentation
Asymptomatic inguinal hernia
- Asymptomatic inguinal hernias are hernias that do not cause symptoms.
- It is frequently detected by chance during a normal medical examination or imaging investigation.
- Even though an inguinal hernia is asymptomatic, it must be evaluated by a specialist to decide whether surgery is required to treat the hernia and avoid complications such as intestinal blockage or strangling.
Symptomatic Inguinal Hernia
- A symptomatic inguinal hernia is a hernia that causes symptoms such as
- Pain
- Discomfort
- A groin protrusion
- Symptoms may aggravate by
- Physical exercise
- Coughing
- Straining during urination or defecation
- Surgical correction of symptomatic hernias is frequently required to ease symptoms and avoid complications.
Strangulated Inguinal Hernia
- A strangulated hernia arises when the contents of the hernia become ischemic owing to a weakened blood supply.
- This happens most often when there is a tiny hole in the musculature and a substantial number of contents within the hernia itself.
Recurrent inguinal hernia
- It arises when a previously healed hernia reappears.
- Recurrent inguinal hernias are more difficult to treat than original hernias and may need more sophisticated surgical procedures.
Causes of Inguinal Hernia
Both a congenital and an acquired component are thought to exist in inguinal hernias. Adult hernias are typically thought of as being acquired.
- Patent processus vaginalis
- A patent processus vaginalis is the most common cause of an indirect inguinal hernia. It is the direct outcome of the testis migrating from its abdominal site to the scrotum, which occurs at 28 weeks of gestation.
- Typically, the process is eliminated during the first few months of life. If all or part of the process stays patent, the defect can cause
- An indirect inguinal hernia
- A scrotal hydrocele
- An encysted hydrocele of the cord
- A “Nuck” hydrocele in a female patient.
- Inguinal hernias occur as a result of a failure to close the canal via which the testes descend from the abdomen and grow into the scrotum. They are more frequent in preterm newborns and boys and affect 1% to 5% of children.
- Increased pressure within the abdomen
- Coughing
- Straining (Repetitive straining during urination or bowel movements)
- Carrying large objects
- Other daily activities which can predispose to inguinal hernia
- The combination of increased abdominal pressure and an existing abdominal wall weakness
- Pregnancy
- Abdominal wall defects (Inflammatory bowel disease)
- Smoking cigarettes
- It has also been proven that smoking cigarettes increases the risk of developing an inguinal hernia.
- It has been demonstrated that patients who smoke have considerably higher levels of circulating serum electrolyte activity.
- Smokers’ serum contains free, unbound, and active protease and elastase substances that disrupt the blood’s protease-antiprotease system, cause the rectus sheath’s collagen and elastin to break down, weaken the fascia transversalis, and increase the risk of inguinal hernias.
- Advanced age
- Ascites
- Cystic fibrosis
- Positive family history
- Connective tissue disorders such as Marfan syndrome or Ehlers-Danlos syndrome can weaken the abdominal wall and increase the risk of hernias.
Signs and Symptoms of Inguinal Hernia
- Pain or discomfort in the groin that is dull, aching, or acute which gets worse with physical activity, coughing, or straining.
- A visible bulge or swelling in the groin region is more visible while standing or in strenuous activity and swelling may be reduced while laying down.
- Testicular or scrotal pain which is aggravated by exercise.
- A sensation of fullness or pressure in the groin area.
- Constipation, vomiting, nausea, and discomfort in the abdomen may all be signs of blockage (when bowel contents cannot flow) or strangulation.
- A scorching or prickling feeling could radiate down the leg or through the pelvis.
Pathophysiology of Inguinal Hernia
- As the abdominal muscles contract, the transversus abdominus and internal oblique’s arching fibers also tighten. The posterior wall is shielded against herniation by this, which functions as a shutter. This is called Shutter Mechanism.
- The deep ring is also made narrower by this contraction. The closure mechanism is the process through which the deep ring narrows.
- Inguinal hernias can be prevented by two key physiological mechanisms when there is increased abdominal pressure. These are the Shutter and Closing Mechanisms.
- The genesis of a hernia may be influenced by the dysfunction of these two systems. Appendectomy has been linked to a threefold increased incidence of right-sided inguinal hernia. This could be because the appendectomy damaged the nerves in the abdominal wall, which could lead to dysfunction of the shutter mechanism.
- Increased intra-abdominal pressure, which can be brought on by several conditions including persistent coughing, constipation, obesity, or hard lifting, is one of the major causes of inguinal hernia. The weak spots in the inguinal canal may protrude outward as a result of the increased pressure, resembling a sac.
- The sac can result in pain, discomfort, and other symptoms and may hold a part of the intestine, the omentum, or other abdominal contents.
- Inguinal hernias may also occur as a result of anomalies in collagen-containing connective tissue, according to research.
- The pathophysiology may get more complicated after a hernia has formed. The herniated tissue may become imprisoned or confined inside the inguinal canal, which may result in discomfort, edema, and other symptoms.
- In extreme circumstances, the blood flow to the herniated tissue may be hampered, resulting in tissue strangling and death.
Diagnosis of Inguinal Hernia
Clinical Examination
An accurate physical examination is necessary to diagnose an inguinal hernia.
- Inspection of any visible bulges or asymmetries in the groin or scrotum
- Palpation of the inguinal canal
- Asked to stand and cough or do the Valsalva technique
Imaging
Ultrasound
- The least intrusive technique is an ultrasound, although its effectiveness depends heavily on the examiner.
- To raise intra-abdominal pressure, the Valsalva technique should be used throughout the test.
- An inguinal hernia may be found with an ultrasound, which has an 86% sensitivity and 77% specificity.
Computed Tomography (CT) Scan
- When the diagnosis is difficult to make, CT imaging is helpful.
- The groin anatomy can be more clearly defined with a CT scan, which can also be used to identify other groin mass causes and severe hernia situations such as incarceration or strangulation.
- A CT scan has a sensitivity of 80% and a specificity of 65% for detecting inguinal hernias.
- Any related pathology, such as tumors or abscesses, can be found via a CT scan.
Magnetic Resonance Imaging (MRI)
- Inguinal hernias may be found with MRI with a sensitivity and specificity of 95% and 96%, respectively.
- Nevertheless, due to its expense and difficult access, MRI is seldom utilized to diagnose an inguinal hernia.
- When necessary, MRI can be utilized to help distinguish between inguinal hernias and sports-related injuries.
Treatment of Inguinal Hernia
Watchful Waiting
- Watchful waiting, commonly known as “watch and wait,” is a non-surgical technique for the treatment of inguinal hernia.
- Patients with tiny, asymptomatic hernias or those who are poor surgical candidates often employ this method.
- The aims of careful waiting are
- To monitor symptoms of a hernia
- To plan the action, if consequences arise
- Yet, patient waiting neither heals nor stops the hernia from enlarging over time.
Pharmacological Management
- Analgesics: Analgesics help ease the pain that an inguinal hernia frequently causes. Stronger prescription drugs like opioids may be required in times of extreme pain, although they are typically only used temporarily owing to the risk of misuse and dependency. Mild to moderate pain can be managed by
- Acetaminophen and
- Non-steroidal anti-inflammatory medicines (NSAIDs)
- Muscle relaxants: Inguinal hernias can cause the abdominal muscles to cramp or spasm, which can be relieved by muscle relaxants like
- Cyclobenzaprine and
- Baclofen
- Proton pump inhibitors (PPIs): These drugs relieve the symptom of acid reflux caused by an inguinal hernia.
Surgical Management
The only effective treatment for an inguinal hernia is surgery.
Open hernia repair
- In the groin, a single, lengthy incision is made for open hernia repair surgery. Either the hernia sac is pushed back or it is tied off and taken out.
- Traditionally, the hernia’s weak area in the muscular wall has been treated by stitching the margins of healthy muscle tissue together (herniorrhaphy). This is excellent for indirect hernias, which are smaller hernias that have been since birth, and for tissues that are healthy since sutures may be used without putting further strain on the tissue.
- Nevertheless, the surgical strategy differs according to the muscle wall region that must be treated and the surgeon’s personal choice.
Laparoscopic repair
- Although the major justification for the use of laparoscopic inguinal hernia repairs has been for bilateral and recurring inguinal hernias, laparoscopic inguinal hernia repair has become a viable choice for the treatment of an inguinal hernia.
- The lower abdomen is cut in three places with incisions of half an inch or less.
- A camera called a laparoscope is placed into the abdomen during laparoscopic hernia surgery to view the hernia defect on a monitor.
- The movements of the surgeon are directed by the picture on the monitor.
- A prosthetic mesh is then used to cover the hernia defect after the hernia sac has been extracted from the abdominal wall defect.
- Surgeons take special care to avoid damaging the vas deferens, bleed-prone blood vessels, or nearby nerves when performing this procedure.
Herniorrhaphy
- The oldest and most common form of hernia surgery is herniorrhaphy.
- A long incision is made over the hernia by the surgeon, who then uses surgical instruments to widen the cut so they may access the hernia.
- The hernia sac is then extracted, and any displaced tissues or organs are restored to their proper positions.
- The sides of the muscle hole or aperture through which the hernia protruded are stitched by the surgeon.
- The incision is sewn up after being sterilized.
- It can be performed using either an open or laparoscopic technique.
Hernioplasty
- In a hernioplasty, the surgeon covers the muscle opening with a flat, sterile mesh, typically composed of flexible polymers like polypropylene or animal tissue, rather than sewing it shut.
- The mesh-shaped hole is carefully trimmed around by the surgeon, who then sutures the patch into the surrounding, healthy tissues.
- The mesh will serve as a regenerative scaffold for the damaged or frail tissues surrounding the hernia.
- Tension-free hernia repair is the most popular name for hernioplasty.
Complications of Inguinal Hernia
- Chronic and persisting pain
- Infertility
- Incarceration
- Bowel obstruction
- Bowel strangulation
Postoperative complications
- Seroma / hematoma formation
- Urinary retention
- Neuralgias
- Testicular pain and swelling
- Mesh infection and wound infection
- Recurrence of hernia
- Inguinal hernia elective repair has a generally low recurrence rate.
- Recurrence rates for mesh repairs are between 3% and 5%, whereas rates for suture repairs are between 10% and 15%.
- Technical issues include the wrong mesh size, too much tension during repair, missing hernias, and tissue ischemia are linked to recurrence.
- Smoking, steroid usage, diabetes, malnutrition, and persistent cough are comorbidities linked to hernia recurrence.
Prevention of Inguinal Hernia
- Maintaining a healthy body weight: Pressure on the abdomen is reduced when normal weight is maintained.
- Refrain from doing strenuous activities and heavy lifting: Because it can extremely lead to straining of abdominal muscles, proper positioning, and technique should be taken into consideration while lifting objects.
- Restrict smoking: As smoking has a high risk of weakening the abdominal muscles, it should be restricted to avoid an inguinal hernia.
- Early treatment of medical condition: Significant medical conditions like Chronic Obstructive Pulmonary Disease and constipation can cause pressure on the intrabdominal wall, it should be treated early to avoid the risk of inguinal hernia. Constipation can be avoided by adequate hydration and intake of a high-fiber diet.
- Avoid straining factors: Tight clothes, such as belts or undergarments that are too small, can exert strain on the abdominal muscles and raise the possibility of hernia formation.
Prognosis
- Generally, inguinal hernias have a favorable prognosis. Inguinal hernias tend to deteriorate with time and often have surgical treatment to avoid complications such as intestinal blockage or strangling. If the hernia is not addressed, it can get bigger, more painful, and more likely to develop problems.
- With surgical correction, the prognosis is usually favorable, and most patients receive relief from symptoms and a lower risk of complications. Healing time and the risk of complications might vary based on the surgical method chosen, the size of the hernia, and the patient’s overall health.
- It is critical to recognize that prompt diagnosis and treatment are critical for achieving the best potential outcome for inguinal hernias.
- According to recent studies, men who are asymptomatic or only mildly sick might choose to wait it out. While there is little possibility of imprisonment and strangling, watchful waiting is seen as a suitable course of therapy.
- It is recognized practice to provide elective surgery to all medically qualified hernia patients, even those with symptomatic inguinal hernia. As femoral hernias have a significant risk of incarceration, they should always be corrected.
Summary
- An inguinal hernia is an abnormal protrusion of intraabdominal contents, typically fat, through the inguinal canal.
- Its anatomical location permits additional classification: A direct inguinal hernia protrudes laterally to the inferior epigastric vessels through the deep inguinal ring, whereas an indirect inguinal hernia protrudes medially to the inferior epigastric vessels through a defect in the posterior wall of the inguinal canal.
- Causes include congenital and acquired. Undescended testis, coughing, straining, and increased abdominal pressure are the primary cause of inguinal hernia.
- In cases when the clinical diagnosis is unclear, imaging, ideally with ultrasonography, is recommended.
- Inguinal hernias can only be successfully treated by surgery, which can be done either open or laparoscopically.
- An inguinal hernia that has been strangled is a surgical emergency. For people with a hernia, manual hernia reduction can be considered a temporary solution prior to surgery, whether there is a bowel obstruction or not.
- Conservative management may be taken into consideration in certain individuals who have a tiny, simple inguinal hernia.
References
- Abdulhai, S., Glenn, I. C., & Ponsky, T. A. (2017). Inguinal hernia. Clinics in perinatology, 44(4), 865-877. https://doi.org/10.1016/j.clp.2017.08.005
- Berndsen, M. R., Gudbjartsson, T., & Berndsen, F. H. (2019). Inguinal hernia-review. Laeknabladid, 105(9), 385-391. DOI: 10.17992/lbl.2019.09.247
- Jiang, Z. P., Yang, B., Wen, L. Q., Zhang, Y. C., Lai, D. M., Li, Y. R., & Chen, S. (2015). The etiology of indirect inguinal hernia in adults: congenital or acquired?. Hernia, 19, 697-701. https://link.springer.com/article/10.1007/s10029-014-1326-5
- Köckerling, F., & Simons, M. P. (2018). Current concepts of inguinal hernia repair. Visceral medicine, 34(2), 145-150. https://doi.org/10.1159/000487278
- Morrison, Z., Kashyap, S., & Nirujogi, V. L. (2022). Adult Inguinal Hernia. StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK537241/
- Öberg, S., Andresen, K., & Rosenberg, J. (2017). Etiology of inguinal hernias: a comprehensive review. Frontiers in surgery, 4, 52. https://doi.org/10.3389/fsurg.2017.00052
- Pastorino, A., & Alshuqayfi, A. A. (2021). Strangulated hernia. StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK555972/
- Shakil, A., Aparicio, K., Barta, E., & Munez, K. (2020). Inguinal hernias: diagnosis and management. American family physician, 102(8), 487-492. https://www.aafp.org/dam/brand/aafp/pubs/afp/issues/2020/1015/p487.pdf