Introduction
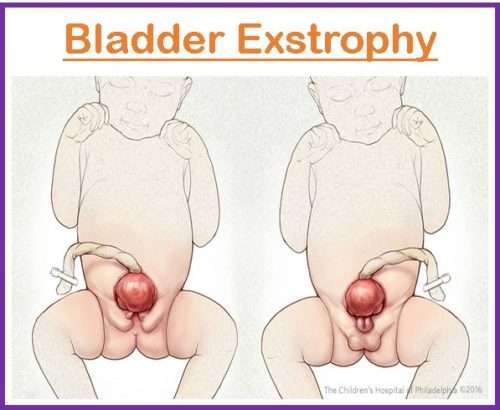
Bladder exstrophy also known as ectopic vesicae is defined as a rare congenital condition that is characterized by a variety of defects affecting the ventral body wall, urinary system, genitalia, bony pelvis, spine, anus, and other structures.
- It happens early in the development of a fetus in the womb.
- The lower abdominal wall and pelvic bones do not form properly during fetal development in bladder exstrophy, resulting in a defect that exposes the interior of the bladder to the outside of the body.
- The bladder is flipped inside out, exposing its mucosal surface on the lower abdomen. The urethra, the tube that transports urine from the body, is frequently shortened and enlarged.
- The external genitalia may be impacted as well, and males may develop epispadias or an aberrant location of the urethral opening. When epispadias is present with bladder exstrophy, it is known as the bladder-epispadias-exstrophy complex (BEEC).
- Bladder exstrophy is usually detected at birth or during prenatal ultrasounds. Early detection is critical since early surgery can result in better results.
Incidence
- According to the most comprehensive international statistics, its prevalence is around 2 per 100,000 births.
- Males are more likely than females to have the disorder, with a male-to-female ratio of roughly 6:1.
- Different ethnic groups have reported cases of bladder exstrophy, however, Caucasian people seem to experience it more frequently.
- Since bladder exstrophy occasionally runs in families or is linked to certain genetic disorders, there is some evidence to support the possibility that the ailment may have a hereditary component.
- With some research indicating that the ailment may be more prevalent in newborns born to older moms, maternal age has been suggested as a possible risk factor for bladder exstrophy.
Causes of Bladder Exstrophy
- Several environmental variables, including maternal nutrition, teratogenic agent exposure, and intrauterine pressure, have been proposed as possible contributors to bladder exstrophy.
- Furthermore, studies have shown that maternal smoking and irradiation during the first trimester enhance the incidence of severe variants of the BEEC spectrum. Periconceptional folate, on the other hand, lowers the incidence of these severe types.
- DNA methylation and histone changes, for example, may have a role in the genesis of bladder exstrophy. Some research has shown that epigenetic changes in genes involved in bladder and pelvic development may play a role in the illness.
- Several genetic mutations and chromosomal anomalies have been linked to the illness, and bladder exstrophy has been recorded in families with a history of the ailment. The inheritance pattern of bladder exstrophy, on the other hand, is unclear, and it is thought to be a multifactorial feature with a complicated genetic base.
- It is hypothesized to be caused by a developmental abnormality in the lower abdomen wall and pelvic bones during fetal growth.
- A cloacal membrane that is unusually large generates a wedge effect and inhibits mesenchymal tissue from migrating medially. As a result, the lower abdomen wall lacks shape. Following a rupture of the cloacal membrane, all the contents herniate, resulting in the clinical picture of BEEC.
Signs and Symptoms of Bladder Exstrophy
- The bladder and urethra are exposed from the abdomen
- Pubis symphysis is widely separated
- Urinary incontinence
- Dribbling of urine
- Bladder mucosa ulcer
- Flattened puborectal sling
- Short, wide urethra
- Meatal stenosis or dorsal hood
- Bifid scrotum, undescended testes: Males
- Bifid/enlarged clitoris, slightly anterior vaginal opening, labia minora separated: Females
- Urinary tract infections (UTIs)
- Vesicoureteral reflux (VUR)
- Displacement of the umbilicus or umbilical hernia
Pathophysiology of Bladder Exstrophy
- During embryonic development, mesodermal tissues that ordinarily give rise to the pelvic bones and lower abdominal wall are unable to migrate and differentiate appropriately.
- As a result of the developmental problem, the lower abdominal wall has a midline defect, which causes the pubic bones to separate and the bladder and urethra to protrude from the body.
- The midline abnormality causes the bladder to flip inside out and protrude outside the body.
- Abnormalities of the urinary system include a short, broad urethra that may be meatal stenotic or have a dorsal hood. Additionally, the prostate gland may be abnormally misplaced.
- It leads to constant seepage of urine from the exposed orifices and accumulation of urine on the skin.
- The pelvic bones are frequently widely spaced, flattened, and underdeveloped, and they occasionally twist outward. Frequently, the sacrum is shortened and flattened.
- Affected structures include the external genitalia, which in men may result in a bifid scrotum and undescended testes. The labia minora may be widely parted in females, and the clitoris may be bifid or larger.
- The following complications may occur.
- Urinary incontinence
- Urinary tract infections
- Bladder stones
- Renal dysfunction
Diagnosis of Bladder Exstrophy
- During a routine sonogram, bladder exstrophy can frequently be detected before birth. Regardless, this condition will be diagnosed immediately after birth during the initial physical examination. The baby’s bladder can be seen outside the belly.
- It may be diagnosed clinically and does not need any extra testing.
- The preoperative work-up includes routine hemograms and blood chemistry tests.
- It is essential to get plain radiographs of the abdomen and pelvis to determine the severity of pubic diastasis.
- It is unusual to have upper tract injury before bladder plate closure because of ongoing urine leaks.
- However, a KUB (kidney, ureter, and bladder) ultrasound should be performed to rule out any concomitant upper urinary tract abnormalities which show abdominal wall bulk in the suprapubic area, below a low umbilical cord insertion. Males have widely separated pubic bones, and a small and broad penis, while females have hemiclitoris on either side of the bladder.
- Nuclear scintigraphy scans and other radiological tests are only performed as follow-up measures.
- It is always preferable to rule out Mullerian structural abnormalities in females by doing an abdominal or perineal ultrasound.
- Bladder swab sampling to assess the local microflora (although enough research is not available for this test)
Treatment of Bladder Exstrophy
Medical Management
Antibiotics
- Urinary tract infection and other skin-related infection is frequently associated with bladder exstrophy when not addressed can cause significant damage to the kidney and cause skin ulcer. Hence, prophylactic antibiotics may be administered to prevent these complications.
- Trimethoprim-sulfamethoxazole
- Nitrofurantoin
- Cephalexin
- Cefadroxil
- Amoxicillin-clavulanate
Bladder management
- Bladder management is needed to prevent the complications. This includes
- Intermittent catheterization,
- Clean intermittent catheterization, or
- Anticholinergic drugs.
- This technique may be used to reduce bladder contractions and enhance bladder emptying.
Nutritional management
- Some individuals with bladder exstrophy may require nutritional assistance, particularly after surgical intervention of the bladder or colon.
- Enteral or parenteral feeding, vitamin and mineral supplements and malnutrition monitoring can be done for nutritional management.
Surgical Management
Patients with bladder exstrophy may be at risk of renal failure due to urinary tract abnormalities. Surgical reconstruction can be done to reduce the effect on the renal system.
- The surgical therapy of classical bladder exstrophy includes operations such as epispadias repair, bladder neck reconstruction, bladder augmentation, and ureteric reimplantation in addition to bladder closure.
- Along with exstrophy restoration, defects in the bony pelvis and pelvic floor must be treated.
- For bladder exstrophy, many methods have been reported. They are divided into two categories:
- Reconstructive procedures and
- Diversion techniques.
- The main aims of exstrophy repair are
- To close the bladder and create a storage receptacle that grows with the child,
- To preserve upper tract function, and
- To reconstruct the genitalia to provide satisfactory functional results in terms of continence and sexual function.
The two most prevalent reconstructive procedures performed by pediatric surgeons worldwide are modern staged repair of exstrophy (MSRE) and Complete primary repair of exstrophy (CPRE).
Modern Staged Repair of Bladder Exstrophy (MSRE)
- The fundamental idea is to do a phased repair (three different operations) on the proper dates. The theory is that each treatment will produce some level of outflow resistance and will aid in bladder growth.
- The main turn-in (bladder closure), performed during the first three days, may help to avoid osteotomy, protect the lower abdomen skin from ammoniacal contents, and protect the bladder from stress. Although the first step is usually completed during the neonatal period, it is sometimes necessary to postpone it. When the bladder template is exceedingly tiny and the closure is technically impossible, this is done.
- The second step, epispadias repair or genitalia reconstruction, is done between the ages of 6 and 9 months. This promotes early bladder cycling and offers outlet resistance for bladder growth.
- The final treatment is bladder neck repair, which is done when the child has enough bladder capacity (at least 100 ml) and has reached a particular age (4-5 years).
Complete Primary Repair of Bladder Exstrophy (CPRE)
- It is also known as Mitchell’s repair since it was invented by Michael Mitchell. The method seeks to complete the entire surgery in a single sitting, including bladder turn-in, bladder neck repair, and epispadias repair.
- The goal is to begin early bladder cycling to enable healthy bladder development. The vesicourethral unit is buried deep into the pelvis after full penile disassembly and split of the intersymphyseal bands.
Complications of Bladder Exstrophy
- Sexual dysfunction
- Renal failure
- Adenocarcinoma
- Epispadias
- Bowel obstruction
- Hernias
- Pelvic organ prolapses
- Surgery related complications
- Wound dehiscence and bladder dehiscence
- Bladder prolapses
- Painful micturition (dysuria)
- Bladder spasms
- Urethral obstruction
- Urethrocutaneous fistula
- Urethral stricture
- Loss of hemiglans/corpora
- Persistent dorsal chordee
- Persistent incontinence
- Bladder stones
Prevention of Bladder Exstrophy
- Prenatal advice, such as mother education on smoking, teratogenicity, and folate consumption during the first trimester, can minimize the incidence of bladder exstrophy.
- Early identification of this illness is critical for secondary prevention.
- Surgery is the most common treatment, and early surgical intervention can minimize the risk of complications and improve long-term outcomes.
- Families with a history of bladder exstrophy may benefit from genetic counseling to better understand the risks of recurrence and make well-informed family planning decisions.
Prognosis
- The severity of the disease, the age at which it is detected and treated, and the existence of concomitant disorders all influence the prognosis for bladder exstrophy.
- Most people with bladder exstrophy can achieve favorable long-term results, including normal urine and sexual function, with early diagnosis and adequate treatment.
- Most patients have a long-term sexual function that is normal. Fertility among men is significantly lower than that of women. Patients who have had diversion procedures had a greater ejaculatory function and fertility than patients who have had reconstructive treatments.
- However, there may be ongoing bladder and bowel control issues, such as the requirement for intermittent catheterization, medication management, and occasional surgery.
- Individuals suffering from bladder exstrophy may also have emotional and psychological difficulties as a result of their disease.
Summary
- Bladder exstrophy is a congenital condition that occurs along the exstrophy-epispadias continuum, most notably involving protrusion of the urinary bladder through an abdominal wall defect.
- Its symptoms vary, but they frequently include anomalies of the bony pelvis, pelvic floor, and genitalia.
- The underlying embryologic process causing bladder exstrophy is unclear, however, it is assumed to be caused in part by a failure of cloacal membrane reinforcement by underlying mesoderm.
- The condition affects both men and women and can cause medical and mental problems such as urine incontinence, recurrent urinary tract infections, and sexual dysfunction.
- Bladder exstrophy is often treated with a series of procedures to restore the pelvic area and reconstruct the bladder.
- Early detection and management are critical in the treatment of bladder exstrophy. Individuals with bladder exstrophy can live healthy and productive lives with adequate medical treatment and support.
References
- Anand, S., & Lotfollahzadeh, S. (2022). Bladder Exstrophy. StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK563156/
- Bhatnagar, V. (2011). Bladder exstrophy: An overview of the surgical management. Journal of Indian Association of Pediatric Surgeons, 16(3), 81. doi: 10.4103/0971-9261.83483
- Crigger, C.B. (2022, May). Exstrophy and Epispadias. Medscape. Retrieved on 2023, Apr 19from https://emedicine.medscape.com/article/1014971-overview
- Dickson, A. P. (2014). The management of bladder exstrophy: the Manchester experience. Journal of Pediatric Surgery, 49(2), 244-250. https://doi.org/10.1016/j.jpedsurg.2013.11.031
- Inouye, B. M., Massanyi, E. Z., Di Carlo, H., Shah, B. B., & Gearhart, J. P. (2013). Modern management of bladder exstrophy repair. Current urology reports, 14, 359-365. https://link.springer.com/article/10.1007/s11934-013-0332-y
- Mitchell, M. E. (2005). Bladder exstrophy repair: complete primary repair of exstrophy. Urology, 65(1), 5-8. https://doi.org/10.1016/j.urology.2004.07.030