Introduction
Japanese encephalitis (JE) is a severe, vector-borne viral encephalitis disease that can be found all over the world but is most prevalent in Asia, the Western Pacific, and northern Australia. Based on incidence and severity, the Japanese encephalitis virus (JEV), a flavivirus spread by mosquitoes, is the main cause of viral encephalitis in Asia. The virus is spread via the bite of mosquitoes of the Culex species.
- In Asia, JEV is currently the leading cause of childhood viral neurological infection and disability.
- Even though most infections are asymptomatic, clinical instances of Japanese encephalitis often present as severe encephalitis, and many survivors experience neurological sequelae
- It does not spread from one person to another.
- Japanese encephalitis typically affects children but all ages can be affected in a population that has never been exposed
- In endemic regions, most people gain immunity by the time they are adults.
- During epidemics, unvaccinated populations may experience high rates of morbidity and mortality.
- Although it can happen in metropolitan areas under specific circumstances, transmission happens most frequently in agricultural regions like farms and rice paddies.
- About one out of every four occurrences of symptoms is deadly.
- Beyond supportive care, there is no specific medicine available, but an efficient vaccine to prevent infection is available.
- For high-risk visitors to endemic regions, immunization is advised. Children’s immunization programs have been undertaken in several endemic regions.
- Preventing mosquito bites is the best form of defense.
Incidence
- Japanese encephalitis (JE) is thought to affect about 68,000 people annually. Most of Asia and portions of the western Pacific are affected by the endemic JEV virus.
- The risk of JE is extremely low for visitors to Asia, although it varies depending on the season, destination, length of stay, and activities.
- The incidence of JE among visitors from nonendemic countries to Asia is 1 case per 1 million visitors, according to estimates.
- 88 cases of JE among people from nonendemic countries were recorded between 1973 and 2020.
- Only 13 JE cases have been reported among visitors from the United States since vaccination became available in the country in 1993.
- With up to 70,000 cases recorded each year, JE is the most common viral encephalitis in Asia.
- Case fatality rates vary from 0.3% to 60% and are influenced by age and population. There have also been sporadic outbreaks in American possessions in the Western Pacific.
- The risk is greatest for people living in rural regions where Japanese encephalitis is endemic, it rarely affects people in cities.
Incubation Period of Japanese Encephalitis
- Humans typically take 5 to 15 days to go through the period of incubation.
Causes of Japanese Encephalitis
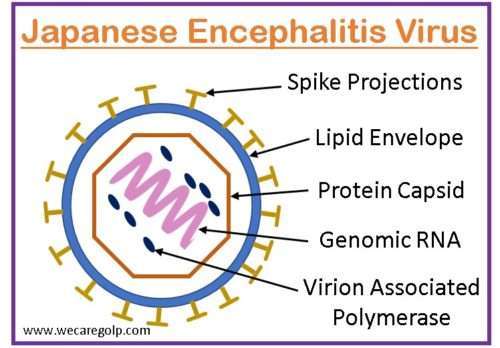
- Japanese encephalitis is caused by the Japanese encephalitis virus (JEV), a single-stranded RNA virus that is closely linked to the West Nile flavivirus.
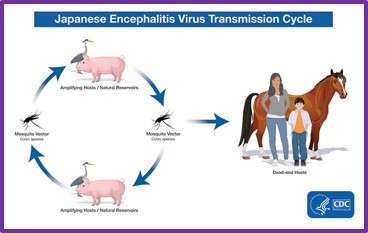
- The Culex species of mosquito, which is primarily prevalent in rural, agricultural parts of Asia, including areas with rice crops, transmits the virus through bites.
Risk Factors of Japanese Encephalitis
The following groups of people are more susceptible to contracting the Japanese encephalitis virus:
- Travelers or expatriates who have spent a lot of time in rural, endemic areas.
- Tourists who camp or hike without a mosquito net when visiting locations where irrigation flooding is practiced.
- Hotels in endemic regions without air conditioning, bed nets, or window coverings.
- Individuals who work in or engage in high-risk outdoor activities (such as camping, fishing, hiking, or gardening).
- People who work or live near piggeries (pigs can contract high viral levels from mosquito bites and can spread the virus to more mosquitoes).
- People who live in rural areas where the disease is endemic.
- Military personnel on active duty went to an endemic area.
Mode of Transmission of Japanese Encephalitis
- JEV is spread to people and animals through mosquito bites carrying the disease.
- The primary mosquitoes that transmit JEV are members of the genus Culex, like Culex tritaeniorhynchus.
Signs and Symptoms of Japanese Encephalitis
Potential signs
- A headache
- Fever
- Neck stiffness
- Nausea and vomiting
- Tremors
- Spastic paralysis.
Other signs
Additionally, a person’s brain function may alter.
- Stupor
- Disorientation
- Coma
- Children’s seizures
- Testicles can enlarge
Pathophysiology of Japanese Encephalitis
- The Japanese encephalitis virus adheres to host cell membranes and begins to spread at the site of the bite and the neighborhood lymph nodes.
- The subclinical disease results from subsequent viremia, but most patients are treated before the virus affects the central nervous system.
- Neuroinvasive illnesses manifest if the virus invades the blood-brain barrier and spreads hematogenously to the brain.
- The Japanese encephalitis virus can influence the formation of neural stem cells in addition to having direct neurotoxic effects.
Diagnosis of Japanese Encephalitis
A diagnosis is made by
- Clinical suspicion,
- Consistent symptoms, and
- A history of travel to a risk area.
Blood test
Clinical laboratory findings may include
- Moderate leukocytosis (raised white blood cell count)
- Hyponatremia (due to the syndrome of inadequate antidiuretic hormone secretion)
- Mild to moderate anemia
- Elevated liver enzymes
- Thrombocytopenia
- Neutrophils may predominate early in the course of the disease
Lumbar Puncture
- Lumbar puncture (spinal tap) is performed to collect cerebrospinal fluid (CSF) for diagnostic purposes.
- In roughly 50% of patients, the CSF opening pressure is increased.
- Common CSF observations include
- A mild to moderate pleocytosis of 10 to several hundred white blood cells/mm3,
- A predominance of lymphocytic cells,
- Slightly increased protein, and
- A normal ratio of CSF to plasma glucose.
Imaging
- For identifying abnormalities linked to JEV, such as alterations in the thalamus, basal ganglia, midbrain, pons, and medulla, magnetic resonance imaging (MRI) is more sensitive than computed tomography (CT) scanning.
- The most frequently reported abnormality is thalamic lesions, which, while they might be very specific for JE in the right clinical setting, are not very sensitive indicators of JE.
- Electroencephalogram (EEG) can detect abnormalities like
- Theta and delta coma
- Burst suppression
- Epileptiform activity
- Sporadically occurring alpha coma
Antibody Test
- An enzyme-linked immunosorbent assay (ELISA) is used to identify JEV-specific immunoglobulin (Ig) M antibodies in serum or CSF.
- IgM antibodies against JEV are seen in CSF, which indicates that the central nervous system has recently been infected. Although an asymptomatic illness or a recent JEV vaccination could also be the cause of IgM antibodies in the serum, which are suggestive of JE.
Treatment/Management of Japanese Encephalitis
- There are currently no known medications that are effective for JE sufferers.
- Symptomatic treatment is used. But there is a vaccine that will protect you against illness.
- Some symptoms might improve with rest, drinks, and over-the-counter painkillers.
- Hospitalization is typically necessary for close monitoring and supportive care.
Complications of Japanese Encephalitis
- Uncontrollable hand swaying
- Personality changes
- Twitching and weakening of the arms and hand muscles
- Minimal learning obstacles
- Weakness on one side of the body
- Paralysis of one limb
Prevention of Japanese Encephalitis
Here are 2 techniques to guard against contracting JEV:
- Stay clear of mosquito bites
- Get vaccinated against the virus
To avoid mosquito bites while traveling or staying in high-risk areas, you can:
- Sleep in rooms with tightly fitting gauze over the windows and doors.
- Utilize a mosquito net impregnated with an insecticide, such as permethrin.
- Spray your room with insecticide.
- Use an effective insect repellent on exposed skin and reapply it as needed; The best repellents contain diethyltoluamide (DEET), picaridin, or oil of lemon eucalyptus.
- Dressing outside in long, loose-fitting clothes.
- Making sure lodging, especially tents, are adequately furnished with mosquito netting or screens.
- Blocking all windows, doors, vents, and other entries with insect screens; employing pesticide sprays, vapor dispensing devices (indoors), and mosquito coils (outdoors) to clean out rooms and keep mosquitoes away from an area
- Clear the area surrounding your home or campsite of any stagnant water where mosquitoes can develop.
- Use mosquito coils, plug-in repellent, or fly spray where you congregate to sit or dine outside.
Vaccination
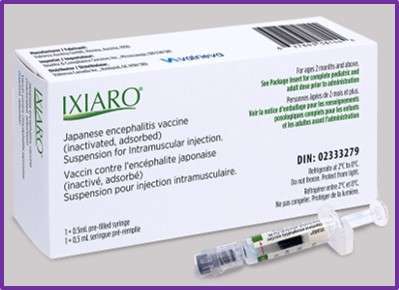
- All the country’s endemic JE receive two doses of the JE vaccine (IXIARO).
- The first dose is given at the age of 9 to 12 months along with the first dose of the measles vaccine.
- The second dosage is given at the age of 16 to 24 months along with DPT and OPV booster doses and the second dose of the measles vaccine.
- In adults who are at risk of being exposed to the virus right away, it is administered in two doses, either 28 days or 7 days apart.
- Individuals who have a weakened immune system (immunocompromised) or pregnant women can also get this immunization.
- A booster dose is recommended after 12 months or more after the two-dose vaccination series.
Prognosis
- Most patients show no symptoms. Only 1% of those who contract the virus go on to acquire the neurological condition.
- Up to 50% of patients who survive symptomatic cases may develop neurological, cognitive, or mental adverse effects, and death is significant (20–30%).
- In less developed nations, the mortality rates linked to Japanese encephalitis may surpass 35%.
- High CSF-neutralizing antibody concentrations are positive prognostic indicators. Low Glasgow coma scale (GCS), hyponatremia, and age under 10 are indicators of poor prognosis.
- About 20 to 30 percent of hospitalized patients die.
- Some people pass away following a brief fulminant course, while others do so following an extended coma.
- Long-term consequences affect between 30 and 50 percent of JE survivors.
- It is believed that JEV infection results in lifetime immunity.
Summary
- Japanese encephalitis is a potentially lethal viral infection of the brain that is typically transmitted through the bite of infected Culex mosquitoes.
- It is frequent in rural areas where rice farming and pig rearing are practiced throughout much of Asia and the Pacific Rim.
- The JEV is spread from pigs and wading birds to humans through the bite of an infected mosquito, and many
- human infections with this virus do not result in symptoms.
- There is a significant mortality rate and a high frequency of neurological sequelae in symptomatic cases needing hospitalization.
- Travelers should receive effective immunization more frequently.
References
- Simon, LV., Sandhu, DS., Goyal, A. (2023, Jan). Japanese Encephalitis. StatPearls Publishing. Retrieved on 2023 April 16 from https://www.ncbi.nlm.nih.gov/books/NBK470423/
- Turtle, L., & Solomon, T. (2018). Japanese encephalitis—the prospects for new treatments. Nature Reviews Neurology, 14(5), 298-313.
- Ajibowo, A. O., Ortiz, J. F., Alli, A., Halan, T., & Kolawole, O. A. (2021). Management of Japanese Encephalitis: A Current Update. Cureus, 13(4), e14579. https://doi.org/10.7759/cureus.14579
- Sewgobind, S., Johnson, N., & Mansfield, K. L. (2022). JMM Profile: Japanese encephalitis virus: an emerging threat. Journal of medical microbiology, 71(12), 10.1099/jmm.0.001620. https://doi.org/10.1099/jmm.0.001620
- Lannes, N., Summerfield, A., & Filgueira, L. (2017). Regulation of inflammation in Japanese encephalitis. Journal of neuroinflammation, 14(1), 158. https://doi.org/10.1186/s12974-017-0931-5
- Sahu, R. C., Suthar, T., Pathak, A., & Jain, K. (2022). Interventions for the Prevention and Treatment of Japanese Encephalitis. Current Infectious Disease Reports, 24(11), 189-204.
- Center for Disease Control and Prevention (2022, Nov 8). Japanese Encephalitis. Retrieved on 2023, April 18 from https://www.cdc.gov/japaneseencephalitis/index.html.