Introduction
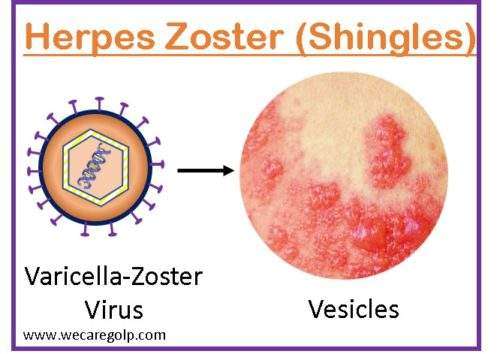
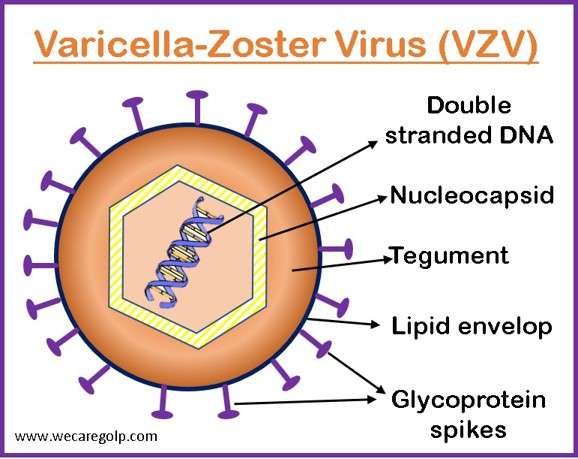
Herpes zoster (HZ), popularly known as shingles, is an infectious disease caused by the varicella-zoster virus (VZV), a ubiquitous DNA virus that belongs to the family of human herpes viruses. VZV is a virus that also causes chickenpox.
The chickenpox virus lies dormant (inactive) after the resolution of chickenpox in the ganglia of the spinal nerve tracts for years or decades. A painful vesicular eruption results from the virus reactivating and moving via the peripheral nerves to the skin, where it multiplies. Herpes zoster is a serious health problem that can affect people of any age. It is more frequently observed in those under the age of 50, in immunocompromised patients, and in people taking immunosuppressive medications.
- A unilateral rash that might encircle the waist or body like a girdle is a typical HZ appearance.
- High VZV concentrations can spread through zoster lesions, most often via the airborne pathway.
- When vulnerable individuals are exposed, it results in a primary varicella infection. Zoster is contagious only after the rash appears and until the lesions crust.
- The immune system’s inability to stop the virus’s latent replication is thought to be the cause of the zoster.
- Herpes zoster incidence and immunological function are closely connected, shingles rarely appear in people who have a high level of immunity.
- Many individuals still experience moderate to severe pain known as postherpetic neuralgia after the herpes zoster has cleared up.
- On the left or right side of the body or face, the rash typically manifests as a single, wide mark.
Incidence
- The prevalence of HZ varies with age and is between 1.2 and 3.4 per 1000 people per year in younger adults and 3.9 to 11.8 per 1000 people per year in older patients (those over 65).
- A comprehensive analysis of studies from 2002 to 2018 estimated the total incidence to be between 2.9 and 19.5 instances per 1000 people, with a predominance of females.
- The death rate for HZ in individuals older than 65 years ranges from 0.0022 to 82.21 per 100,000 people, according to the Global Burden of Disease database.
- Patients with immunosuppression get recurrences the most frequently. Unvaccinated youngsters, the elderly, and those with weakened immune systems are those who face the most risk.
- Before 1995, the number of cases in the US per year was believed to be 3.5 million. Since 1995, when a licensed vaccine became available, there have been thought to be 100,000–200,000 cases of varicella and 300,000 cases of zoster each year.
- In the United States, varicella and its consequences cause about 100 fatalities each year.
Incubation period
- Incubation times for shingles range from 10 to 21 days. From one to four days before the cutaneous rash appears and until all vesicular cutaneous lesions have healed, varicella is infectious.
- This might last longer in immunocompromised individuals or after receiving immunoglobulin as a passive varicella vaccine.
Causes of Herpes Zoster
- The varicella-zoster virus (VZV) is the causative organism of Herpes zoster, the same virus that causes chickenpox.
- Blood, skin, and nerve cells are among the cell types that the virus can infect and spread to in the body.
- In most cases, the reactivation of the VZV is the cause of herpes zoster. If you have already had chickenpox, the virus can reactivate in your body and cause shingles.
Risk Factors of Herpes Zoster
Those who have experienced chickenpox are more likely to experience shingles, including:
- Age- As you get older, your risk of getting shingles rises. Those over the age of 50 are often affected by shingles. Moreover, those over 60 are more susceptible to more serious consequences.
- Immune-suppressive illnesses– Chances of developing shingles are increased by immune-suppressive illnesses such as cancer, diabetes, and HIV/AIDS.
- Cancer treatment– Treatments for cancer in addition to potentially causing shingles, radiation and chemotherapy can reduce your resistance to illness.
- Certain medications– Immunosuppressants and long-term use of steroids (prednisone) can raise the risk of getting shingles.
- History of previous chickenpox
- Being exhausted
- Experiencing stress or anxiety
- Malnutrition.
Signs and Symptoms of Herpes Zoster
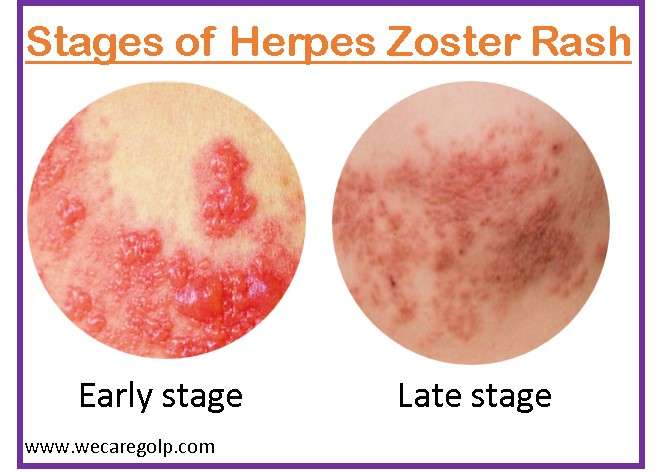
The three stages of clinical symptoms are the pre-eruptive phase, acute eruptive phase, and chronic phase.
Pre-eruptive phase
This stage appears at least 48 hours before any visible lesions.
- Atypical skin sensations or pain
- Photophobia
- An overall malaise
- Headaches
Acute eruptive phase
- Symptoms present in the pre-eruptive phase
- Painful vesicles following macules
- Tingly and itchy rashes
- The vesicles burst, ulcerate, and then crust over
- Although the phase could last 2-4 weeks, the pain continues
- Fever
- Chills
- Upset stomach
Chronic infection
- Recurrent pain (lasts longer than four weeks).
- Paresthesia
- Shock-like sensations
- Dysesthesia.
Mode of Transmission
People who have never had chickenpox or the chickenpox vaccine can contract VZV. When contaminated, they will get chickenpox, not shingles. Shingles may develop later in life.
- Direct skin contacts through skin lesions (direct contact with fluid)
- Airborne droplets (coughing, sneezing)
Pathophysiology of Herpes Zoster
- The herpes zoster virus spreads through either direct skin contact or by inhaling virus-containing droplets. Although the infection is contagious to those who have never been infected with varicella zoster, transmission rates are low.
- The virus begins replicating in the epithelial cells as soon as it enters the body. The virus is then taken up by immune cells and sent to nearby lymph nodes, where it keeps reproducing.
- The VZV enters the skin and spreads by directly infecting one keratinocyte and then another.
- Sometimes, this might lead to the development of enormous multinucleated cells called Tzanck cells.
- The virus also spreads to the trigeminal ganglion in the skull and the dorsal root ganglion in the trunk, infecting sensory neurons in the skin.
- The viral particles are eventually removed from the body by the immune system, but those that penetrate sensory ganglion cells may do so and enter a latent condition.
- The varicella-zoster virus can reactivate, move down the sensory neuron, and infect the skin of a particular dermatome in patients with compromised immune systems, leading to herpes zoster.
Diagnosis of Herpes Zoster
Clinical assessment
- Patients with herpes zoster are thought to have the characteristic rash and, in some cases, even before the rash appears, if they experience typical pain in a dermatomal distribution.
- Typically, the nearly pathognomonic rash is used to make the diagnosis.
Laboratory tests
Polymerase chain reaction (PCR)
- PCR is widely used to detect VZV DNA.
- Swabs of unroofed vesicular lesions and scabs from crusted lesions are reliable samples for PCR.
- To confirm probable HZ-type pain without a rash, PCR is helpful.
Direct fluorescent antibody (DFA)
- The sample for DFA is taken from vesicular fluid or a corneal lesion
Tzanck smears
- Although the Tzanck smear shows the presence of a herpetic lesion, it is unable to distinguish between VZV and other herpes viruses.
- It is less sensitive and selective than polymerase chain reaction (PCR) or direct fluorescent antibody (DFA).
Specific IgM antibody
- During chickenpox or shingles infection, varicella-zoster virus-specific IgM antibody in the blood is detectable, but not when the virus is latent.
- When there is ocular involvement, vesicular fluid or corneal fluid can be tested directly using fluorescent antibodies.
Treatment/Management of Herpes Zoster
Herpes zoster outbreaks typically subside on their own without medical attention.
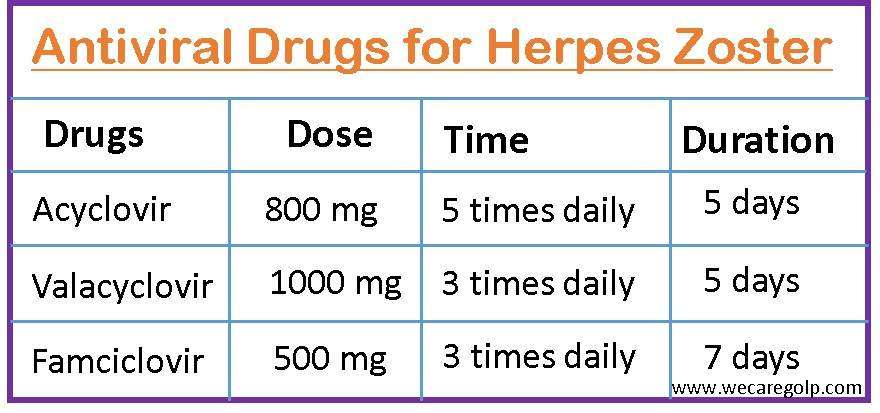
- Particularly in senior individuals, antiviral medication speeds up the healing of lesions, reduces acute pain, and helps to prevent post-herpetic neuralgia.
- Antiviral therapy can assist with decreasing the intensity and length of symptoms, preventing complications, and decreasing the likelihood that the rash will return.
- Antibiotic creams applied topically, such as mupirocin or soframycin, aid in preventing subsequent bacterial infections
- Parenteral foscarnet should be used to treat infections brought on by acyclovir-resistant VZV strains, which are often limited to immunocompromised hosts.
- Analgesics or in some cases narcotics may require to relieve pain.
- The CDC advises using calamine lotion, having a warm oatmeal bath, and applying a cool, damp washcloth to the blisters to reduce irritation.
Other supportive measures to relieve symptoms without medications are:
- Reducing stress as much as possible
- Eating regular, nutritious meals
- Engaging in some light exercise
- Dressing comfortably in loose-fitting clothing
- Partaking in relaxing activities that will lower stress and distract one from discomfort, such as reading, watching television, talking to friends, participating in hobbies, or participating in social activities.
Complications of Herpes Zoster
The complication may occur to any person, especially in those with weakened immune systems.
Postherpetic neuralgia
- After the blisters have healed, patients still experience pain which is called postherpetic neuralgia.
- It happens when injured nerve fibers cause pain signals to travel from your skin to your brain in a jumbled, excessive manner.
- It is the most common complication of shingles and can range from weeks to months, or even years.
Neurological conditions
- Encephalitis
- Hearing loss
- Facial paralysis
- Balance problems
Postherpetic itch
- It appears in the skin that has a substantial sensory loss.
- Scratching the afflicted region might cause more skin damage and a bacterial superinfection of the sores.
- Some relief can be obtained by using topical local anesthetics that numb the skin.
Herpes zoster ophthalmicus
- Up to 20% of cases of shingles have herpes zoster ophthalmicus (HZO). It affects the eyes or the area around them.
- Up to 70% of people with HZO who go untreated experience major side effects, such as
- Light sensitivity
- Eyelid swelling
- Glaucoma
- Corneal inflammation and scarring
- Vision impairment and blindness
Herpes zoster oticus (Ramsay Hunt syndrome)
- Hearing and balance issues
- Facial weakness on the affected side
Visceral involvement
- Acute retinal necrosis
- Pneumonitis
- Hepatitis
- Meningoencephalitis.
Prevention of Herpes Zoster
The goal of HZ prevention is to stop the latent VZV virus from reactivating and spreading. Stimulating VZV immunity is one of the methods used to prevent HZ in the general population, particularly in older and high-risk individuals.
Vaccination
- The Centers for Disease Control and Prevention (CDC) advise persons aged 50 and older to receive two doses of the recombinant zoster vaccine (RZV) (Shingrix), 2–6 months apart, regardless of prior herpes zoster episodes or previous administration of the live zoster vaccine (ZVL) (Zostavax).
- Due to a higher risk to get shingles and its complication, immune-weakened patients over the age of 19 should also take two doses of Shingrix.
- Live shingles vaccine may be utilized in some situations like
- When a patient is allergic to RZV,
- When a patient prefers live shingles vaccine or
- When recombinant shingles vaccine is unavailable.
- Those who had previously gotten Zostavax, should still be vaccinated with Shingrix.
Varicella-Zoster Immunoglobulin (VZIG)
- The CDC advises giving VZIG to susceptible or immunocompromised individuals who have been exposed to varicella or herpes zoster to prevent or reduce clinical disease.
- It should be used only in people who are at high risk of serious illness or complications, such as newborns, immunocompromised patients, and pregnant women.
- VZIG is most beneficial when given as soon as possible after the alleged exposure, but it can still be useful if given up to 96 hours later.
- The CDC estimates that protection following VZIG therapy lasts for 3 weeks on average.
Other Preventive Measures
- Cover the rash.
- Avoid touching or scratching the rash.
- Wash your hands frequently.
- Avoid using immune system-suppressing drugs if possible.
- Personnel with zoster may not be allowed to work in some healthcare facilities until their lesions have crusted over and dried.
- Until lesions are crusted, people with localized zoster should avoid contact with vulnerable people who are at high risk for developing severe varicella at home and work.
Prognosis
- The rash normally resolves within 10–15 days.
- For patients who are younger and otherwise healthy, the prognosis is very good.
- Most sufferers fully recover from shingles in 3–5 weeks, but some have serious side effects. Complications are much more likely to occur in the elderly.
- In immune-competent people, it rarely results in death, but in critically weakened or immunocompromised patients, it can be lethal.
- In immunocompromised patients, diffuse zoster might result in encephalitis, hepatitis, or pneumonitis, which can be fatal.
- The mortality rate from widespread herpes zoster ranges from 5% to 15%.
- Most of the time, morbidity is limited to the painful dermatome, which can be uncomfortable or incapacitating.
Summary
- Herpes zoster (HZ, shingles, zoster) is a condition marked by dermatomal rashes, pain, and unilaterality that results from the persistent varicella-zoster virus (VVZ) reactivating and multiplying after a previous varicella infection.
- Thoracic, trigeminal, lumbar, and cervical dermatomes are the ones most frequently involved in HZ lesions.
- The initial lesion is typically an erythematous macule or papule, which then develops into a vesicle, pustule, and crust for two to three weeks.
- The primary clinical symptoms, such as dermatomal discomfort and the eruption of clustered vesicles in the same dermatome, are used to make the diagnosis.
- In HZ patients, antiviral therapy’s primary objective is to lessen the size, length, and intensity of rashes and pain.
- The use of the varicella-zoster virus vaccine, whether it is a live or recombinant vaccine, is one of the preventative measures for HZ in elderly and high-risk patients.
References
- Patil, A., Goldust, M., Wollina, U. (2022). Herpes zoster: A Review of Clinical Manifestations and Management. Viruses, 14(2):192. https://doi.org/10.3390/v14020192
- Nair, PA., Patel, BC., (2022 Sep 5). Herpes Zoster. StatPearls Publishing. Retriveed on 2023, Feb 20 from https://www.ncbi.nlm.nih.gov/books/NBK441824/#!po=57.6923
- Cadogan, S.L., Mindell, J.S., Breuer, J. et al. (2022). Prevalence of and factors associated with herpes zoster in England: a cross-sectional analysis of the Health Survey for England. BMC Infect Dis 22, 513. https://doi.org/10.1186/s12879-022-07479-z
- Koshy, E., Mengting, L., (2018, Mar 8). Epidemiology, treatment, and prevention of herpes zoster. Indian J Dermato, 84, 251-262. doi: 10.4103/ijdvl.IJDVL_1021_16
- Marra, Y., Lali, F. (2022). Prevention of Herpes Zoster: A Focus on the Effectiveness and Safety of Herpes Zoster Vaccines. Viruses, 14(12), 2667. https://doi.org/10.3390/v14122667
- Center for Disease Control and prevention. (2022, Feb 3). Shingles (Herpes zoster). Retrieved on 2023 Feb 23 from https://www.cdc.gov/shingles/index.html