Introduction
Polycystic ovarian syndrome (PCOS) is one of the most common endocrine disorders of reproductive-age women caused by hormonal imbalances produced by the ovary.
- Without the specific underlying disease of the adrenal or pituitary glands, two of the following three features help diagnose PCOS.
- Irregular menstrual cycle
- High androgen levels
- Multiple ovarian cysts
- Women with PCOS may experience infertility, a higher risk of miscarriage, hirsutism, amenorrhea or oligomenorrhea, anovulation, and excess androgen production which leads to deviations from the societal standards of femininity.
- Androgens are male sex hormones that women typically only produce in small quantities.
- Thus, PCOS is highly stigmatized and may be regarded as the theft of womanhood.
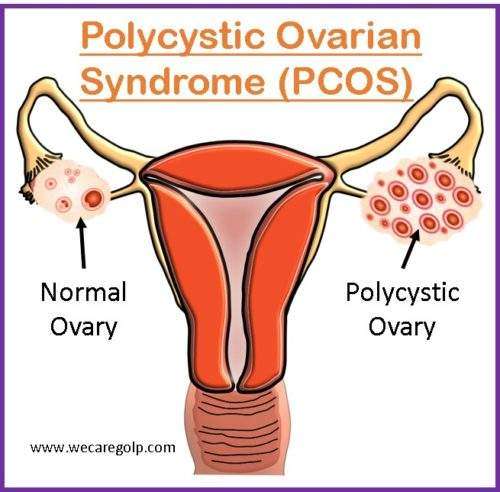
- A polycystic ovary is defined as (on ultrasonography) an ovary containing:
- ≥12 follicle cysts (small fluid-filled sacs with immature eggs) in an ovary.
- 2 to 9 mm in diameter or,
- Ovary with volume > 10 cm3.
Incidence
- Globally, the polycystic ovarian syndrome affects 1 in 15 women.
- The 1990 National Institutes of Health (NIH) criteria defined polycystic ovarian syndrome in unselected populations of women of reproductive age had a prevalence between 6.5 and 8%.
- Polycystic Ovarian Syndrome is the most common cause of anovulation and up to 30% cause of infertility in couples seeking treatment.
Signs and Symptoms of Polycystic Ovarian Syndrome
- Irregular menstrual periods
- Oligomenorrhea: Irregular and inconsistent menstrual flow with less than 8 cycles of menstrual period per year or menstrual cycles longer than 35 days.
- Amenorrhea: The absence of menstruation cycles for more than 3 months duration without pregnancy.
- Anovulation (bleeding but no ovulation)
- Menorrhagia (heavy menstrual bleeding)
- Infertility
- Pelvic pain
- Hirsutism (excess hair growth on the face, chest, stomach, or thighs)
- Weight gain (trouble losing weight)
- Severe and persistent acne (no response to usual treatments)
- Acanthosis nigricans (darkening and thickening of the skin)
- Thinning hair
- Headache
Causes of Polycystic Ovarian Syndrome
- The exact cause of PCOS is unknown. However, insulin resistance and faulty feedback mechanisms on the hypothalamic-pituitary-ovarian axis are believed to be the cause of PCOS.
- It may be caused due to environmental insults as well as genetic predisposition.
Risk Factors
- Obesity
- Family history of diabetes type 2
- PCOS insulin resistance genes
- Family history of PCOS
Pathophysiology
- The exact etiology and pathophysiology of polycystic ovary syndrome (PCOS) are largely unknown.
- The key feature of PCOS, hyperandrogenism, has a synergistic effect with insulin resistance.
- However, the contribution of hyperandrogenism and insulin resistance differs from patient-to-patient accounting for the heterogenous nature of PCOS and its presentation which makes it further difficult to understand the pathophysiology.
- Besides insulin resistance and hyperandrogenemia, anti-müllerian hormone (AMH) and vascular endothelial growth factor (VEGF) have been regarded as causative factors of PCOS.
- Normally, the ovaries of the female reproductive system produce trace amounts of androgens.
- In polycystic ovary syndrome, the ovaries produce an abnormal amount of androgens, and numerous small cysts are found in the ovaries.
- The women do not produce adequate hormones required for ovulation resulting in oligomenorrhea and chronic anovulation.
- Progesterone is a GnRH inhibitor that exhibits a negative feedback mechanism on gonadotropin-releasing hormone (GnRH) from the hypothalamus.
- Increased frequency of GnRH pulses results in LH rise.
- In PCOS, follicles do not ovulate due to an increased LH/FSH ratio.
- FSH helps in follicle maturation for further ovulation.
- In PCOS, LH is relatively higher and FSH is relatively lower. Thus, lower levels of FSH results in follicles not maturing enough to become functional graafian follicle that can ovulate.
- Thus, the follicles do not mature and becomes a cyst.
- Multiple cysts represent past failed ovulation.
- Excess LH also stimulates the thecal cells to produce higher amounts of androgens.
- Furthermore, insulin released from the pancreas can stimulate steroidogenesis in the thecal cells of the ovary.
- Androgens show a negative feedback effect on the hypothalamus and pituitary gland.
- It results in increased hormonal imbalance and reduced insulin sensitivity that results in insulin resistance.
Diagnosis of Polycystic Ovarian Syndrome
History taking
- Family history of diabetes mellitus, cardiovascular disease, and hyperlipidemia.
- Lifestyle including the history of diet and exercise
- Reproductive history including the onset of menstruation, duration of menstruation, amount of bleeding
Physical Examination
- BMI calculation
- Waist-to-hip ratio
- Presence of characteristic features of PCOS like:
- Excessive acne
- Androgenic alopecia
- Hirsutism
Investigations
- Serum lipids (cholesterol, triglycerides, HDL level)
- Blood glucose levels with a two-hour oral glucose tolerance test
- Serum testosterone (total, free, bioavailable)
- Serum dehydroepiandrosterone sulfate (DHEAS)
- Serum FSH
- Serum LH
- Serum estradiol
- Ovarian ultrasonography
Since the manifestations of PCOS may resemble other morbidities, various tests may be performed to rule out the diagnosis of PCOS which are:
- Pregnancy test
- Serum TSH
- Prolactin
- 17-hydroxyprogesterone
- Prolactin levels
- Salivary/ urinary cortisol
- Dexamethasone suppression test
- MRI of adrenals
- Depression screening
- Obstructive sleep apnea in overweight and obese patients.
Management of Polycystic Ovarian Syndrome
The management of polycystic ovarian syndrome depends on the patient’s clinical manifestations and the desire for pregnancy. Since, PCOS affects multiple organ systems and has significant metabolic and reproductive manifestations, a wide range of therapy may be done.
Anovulation and Infertility Management
Lifestyle modification
- A calorie-restricted diet
- Physical exercise
- Weight reduction
- Cessation of smoking
Induction of Ovulation
The treatment of choice for women with infertility is the induction of ovulation.
- The commonly used medicines for ovulation induction are
- Clomiphene
- Letrozole
- Gonadotropins (injection)
- Other drugs used for the induction of ovulation are:
- Anti-estrogen, most commonly clomiphene citrate
- Low dose gonadotropins
- Oral contraceptives
- Anti-progestins
- However, progestins that have intrinsic androgenic activity should be avoided.
- Metformin is the drug of choice for managing insulin resistance in PCOS.
- Besides medicines, the following treatment options may help a woman to be pregnant.
- Surgery: Removal of the tissue from the ovaries that produce androgen hormones.
- In vitro fertilization (IVF): Fertilization takes place in a lab before transferring it to the woman’s uterus.
Hirsutism Management
- Moderate and localized symptoms of hirsutism can be managed by the removal of hair.
- If severe clinical forms are present, anti-androgen therapy can be done. Anti-androgenic drugs are:
- Spironolactone (Mineralocorticoid antagonist)
- Cyproterone acetate
- Flutamide
- The side effects should be monitored while using anti-androgens.
- Lethargy
- Mood changes
- Loss of libido
Menstrual Irregularity Management
- Hormonal contraception (oral contraceptive, dermal patch, or vaginal ring) can be used.
- Chronic anovulation may cause endometrial hyperplasia which may be prevented by
- Progesterone derivative
- Progestin-containing oral contraceptives
- The levonorgestrel-releasing intrauterine system.
Acne Management
- The first course of treatment is hormonal contraception.
- Other drugs used in topical acne therapy are:
- Retinoids
- Antibiotics
- Benzoyl peroxide.
Complications of Polycystic Ovarian Syndrome
Polycystic ovary disease is mostly associated with hyperinsulinism and insulin resistance, which increases the risk of getting type 2 diabetes mellitus and cardiovascular disease. Various body systems are also affected by polycystic ovary syndrome resulting in several health complications. Some of them are:
- Menstrual dysfunction
- Infertility (inability to become pregnant)
- Hirsutism (excessive hair growth on parts of the body)
- Metabolic syndrome
- Type 2 Diabetes Mellitus
- High blood pressure
- Cholesterol problems (low HDL, high LDL)
- Endometrial cancer
- Obstetrical complications
- Cardiovascular disease
- Stroke
- Sleep apnea (stop breathing during sleep)
- Mood disorder, depression
- Eating disorder
Complications associated with the infertility treatment
- Multiple pregnancies
- Ovarian hyperstimulation
- IVF cycle cancellation
- Early pregnancy loss
- Gestational diabetes
- Pre-eclampsia
- Perinatal mortality
- Premature delivery
Prevention of Polycystic Ovarian Syndrome
- PCOS is not a preventable disease. But symptoms can be reduced by taking small steps.
- However, early identification and management of risk factors like poor diet, obesity, lack of exercise, and stress can be done.
- Bariatric surgery may be considered for the treatment in women with PCOS with severe obesity (BMI>/= 40) or moderate obesity (BMI>/= 35) with comorbid conditions.
Prognosis
- PCOS is not a single disease but encompasses a cluster of them.
- Almost 80% of anovulatory infertility cases are related to polycystic ovarian syndrome.
- PCOS most commonly leads to anovulatory infertility, miscarriage, pregnancy-related complications, and symptoms related to elevated androgen levels.
- Women with PCOS are prone to significant health problems related to hyperinsulinemia with an increased risk of diabetes and cardiovascular risk factors.
Summary
- Polycystic ovary syndrome is caused by an imbalance of reproductive hormones, mostly androgens.
- The clinical features of PCOS are hyperandrogenism, chronic anovulation, and polycystic ovaries.
- However, it is unknown what exactly causes PCOS.
- The abnormal LSH/FH ratio leads to the clinical manifestations of hyperandrogenism like excess hair growth, irregular, absent, or disrupted periods, and infertility.
- Management of PCOS includes the management of anovulation and infertility, hirsutism, acne, and menstrual irregularity.
- The absence of menstruation and men-like physical features leads to psychosocial issues in women with PCOS.
References
- Norman, R. J., Dewailly, D., Legro, R. S., & Hickey, T. E. (2007). Polycystic ovary syndrome. The Lancet, 370(9588), 685-697. https://doi.org/10.1016/S0140-6736(07)61345-2
- Homburg, R. (2008). Polycystic ovary syndrome. Best Practice & Research Clinical Obstetrics & Gynaecology, 22(2), 261-274. https://doi.org/10.1016/j.bpobgyn.2007.07.009
- Franks, S. (1995). Polycystic Ovary Syndrome. The New England Journal of Medicine, 333,853-861. DOI: 10.1056/NEJM199509283331307
- Kitzinger, C. & Willmott, J. (2002). “The thief of womanhood”: women’s experience of polycystic ovarian syndrome. Social Science & Medicine, 54(3),349-361. doi: 10.1016/s0277-9536(01)00034-x
- Bates, G. W., & Legro, R. S. (2013). Long-term management of Polycystic Ovarian Syndrome (PCOS). Molecular and Cellular Endocrinology, 373(1-2), 91-97. doi:10.106/j.mce.2012.10.029
- Harada, M. (October 2022). Pathophysiology of polycystic vary syndrome Revisited: Current understanding and perspectives regarding future research. Reproductive medicine and biology. Reproductive Medicine and Biology, 21(1), e12487. https://doi.org/10.1002/rmb2.12487
- Hart, R., & Norman, R. (2006). Polycystic ovarian syndrome-prognosis and outcomes. Best Practice & Research Clinical Obstetrics & Gynaecology, 20(5), 751-778. doi: 10.016/j.bpobgyn.2006.04.006