What is gestational diabetes (GD)?
Gestational diabetes is a disorder of carbohydrate metabolism that occurs or recognizes for the first-time during pregnancy. With an incidence of around 5%, it is one of the most common diseases in pregnancy.
- In gestational diabetes, blood glucose levels elevate.
- It slightly increases the risk for certain rare birth complications.
- However, the risk can usually normalize again just by changing the diet.
- Most women with gestational diabetes have an otherwise normal pregnancy and give birth to a healthy baby.
- Gestational diabetes does not mean you permanently have diabetes (type 1 or type 2 diabetes).
What are the causes of GD?
- The causes of GD are usually unclear.
- It could be the various pregnancy hormones that lead to raised blood glucose levels (e.g., oestrogen, human placental lactogen etc.) and often malnutrition.
- Insulin secretion tends to be reduced at the beginning of pregnancy but then increases significantly.
- As in type 2 diabetes (also known as adult-onset diabetes), the organ cells do not respond sufficiently to insulin and produced insulin is too low to bring blood glucose levels to expect.
Who are at risks of GD?
Any woman can get gestational diabetes during her pregnancy. Some women have a greater risk of gestational diabetes. A woman is more likely to develop gestational diabetes if she:
- Is overweight (Her body mass index (BMI) is above 30) and obesity
- Had gestational diabetes in a previous pregnancy
- Previously delivering a baby weighing more than 9 pounds (4.1 kilograms).
- Has a history of diabetes in her family
- Has an ethnic group of South Asian, Black, African-Caribbean or Middle Eastern origin
- Has prediabetes (blood sugar levels are higher than they should be but not high enough to be diabetes)
- Has polycystic ovary syndrome (PCOS) or another health condition linked to problems with Insulin
- Has high blood pressure, heart disease, high cholesterol, or other medical complications.
- Is older than 30.
If you have any of these conditions, you should inform your doctor. It helps to do screening earlier for gestational diabetes during your pregnancy.
What are the symptoms of GD?
- As a rule, gestational diabetes does not cause any noticeable symptoms.
- However, if the blood glucose level rises sharply, the symptoms such as fatigue, weakness, need to pee more often as usual or more thirst may occur. It is similar to other forms of diabetes.
- Usually, the symptoms are mild and interpreted as typical pregnancy complaints.
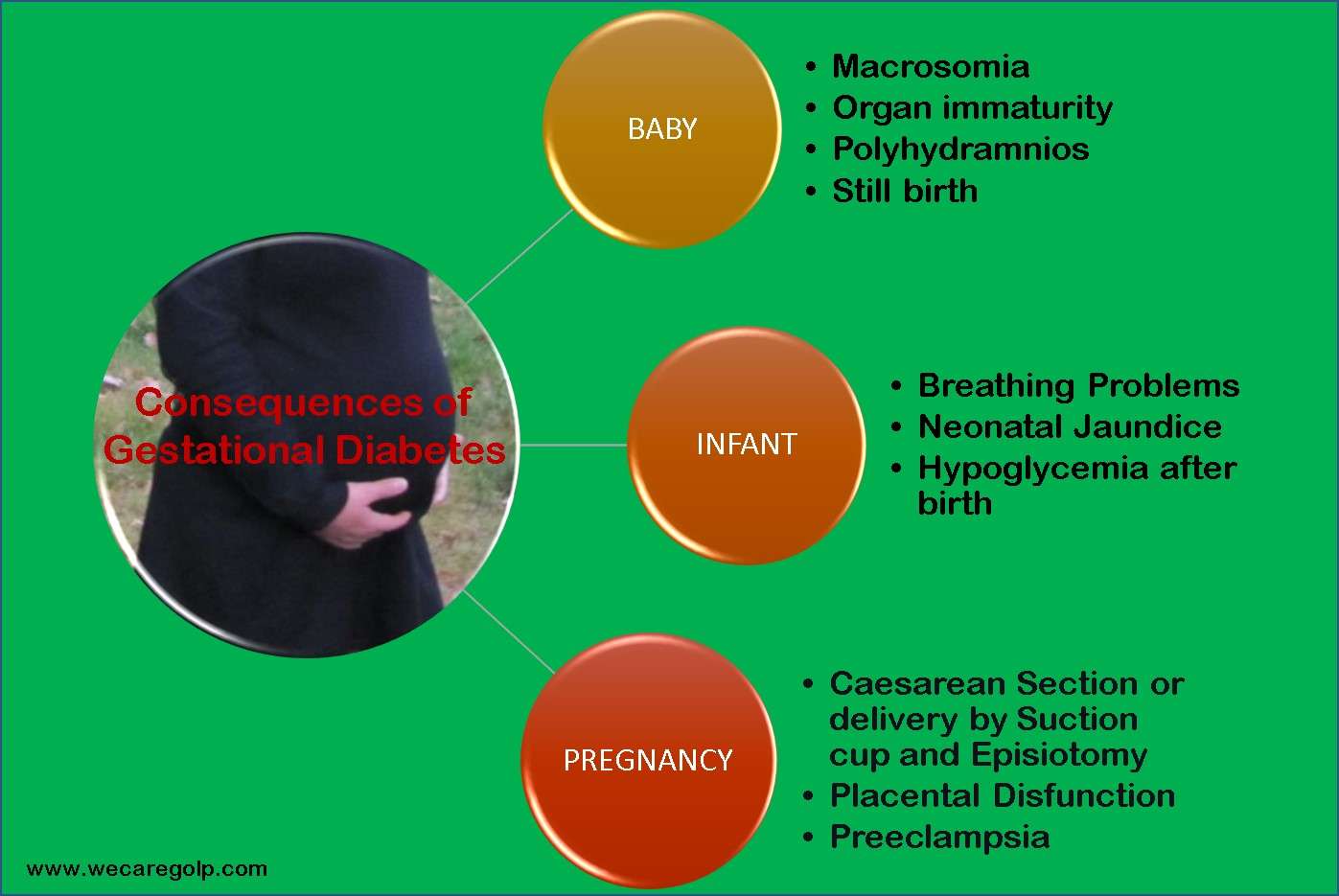
What consequences can gestational diabetes have?
Probably every pregnant woman wishes for a normal pregnancy and birth. Most children have average growth and development when their mothers have gestational diabetes.
However, there are women for whom treatment has advantages.

How can gestational diabetes affect your baby?
- The high blood sugar concentrations eventually pass to the child via the placenta and the umbilical cord.
- The child reacts to the high blood sugar levels with its increased insulin production and incorporates the sugar into its body as fat. High blood sugar makes the child fatter and larger (macrosomia).
- The organs of the child are unfortunately often functionally immature.
- At the same time, the child produces more urine, which increases the amount of amniotic fluid (called polyhydramnios).
- Stillbirth is rare (baby’s death either before or shortly after birth).
These are risk factors for premature birth.
In addition, the birth of large children is more complicated than that of normal-weight children.
How can gestational diabetes affect your infant?
- They often have breathing problems and high blood pigment levels, and as a result, they are more likely to suffer from neonatal jaundice (icterus).
- They also suffer more often from hypoglycaemia after birth because the child’s organism initially continues to produce more insulin than necessary.
However, these complications can avoid because gestational diabetes can treat exceptionally well.
How can gestational diabetes affect your pregnancy?
- Because of big babies, patients with gestational diabetes more often require a caesarean section or delivery by suction cup and episiotomy.
- Blood flow in the placenta may also be disturbed and needs to check.
- Elevated blood glucose also increases the risk of another rare pregnancy condition: preeclampsia. This pregnancy disorder is associated with increased protein excretion in the urine, raised blood pressure, and water retention in the body. Without treatment, preeclampsia can harm mother and child.
How is gestational diabetes diagnosed?
- The best way to detect GD is a sugar test (oral glucose tolerance test, oGTT).
- An oral glucose tolerance test measures elevated blood glucose levels.
- It measures how the body reacts to a large amount of glucose.
- The test poses no risks to the mother or baby, but some women find the sweet liquid unpleasant.
- The sugar test offers in the 6th or 7th month (or 24 – 28 Weeks) of pregnancy.
- If you decide to take it, you will get two diagnostic tests.
Oral Glucose Tolerance Test (oGTT)
First Pre-Test:
- You will first do a pre-test where you drink a glass of water with 50 grams of sugar.
- You do not have to be fasting for this pre-test.
- After one hour, blood will draw from a vein in your arm, and the blood sugar will determine.
- If the value is below 7.5 millimoles per liter (mmol/l, which corresponds to 135 mg/dl), the result is unremarkable, and the test is over.
- If an elevated value finds in the pre-test, this is not yet a diagnosis.
Second Test:
- The pre-test serves to identify women who will offer a second, decisive sugar test.
- This second test is more complex. For this “diagnostic test”, the pregnant woman must be fasting, i.e., not have eaten, or drunk anything for at least twelve hours; only water is allowed.
- The test begins by drawing blood from the woman while she is fasting.
- Only then does she drink a sugar solution containing 75 grams of glucose.
- After one and after two hours, blood draws again from a vein in the arm.
- If one of the following three blood glucose values is reached or exceeded, she will diagnose with “gestational diabetes”:
– Fasting: 5.1 mmol/l (92 mg/dl),
– After one hour: 10.0 mmol/l (180 mg/dl),
– After two hours: 8.5 mmol/l (153 mg/dl).
- The result will document in the maternity record.
What are the target blood sugar levels for woman with GD?
American Diabetes Association (ADA) suggests the following target for women testing blood sugar levels during pregnancy:
- Before a meal: 95 mg/dl or less
- One hour after a meal: 140 mg/dl or less
- Two hours after a meal: 120 mg/dl or less
Always remember that GD is treatable, and a healthy pregnancy can help ensure working with your health care team.
How can gestational diabetes be treated?
- In most cases, elevated blood sugar can be sufficiently lowered simply by changing the diet and increasing exercise. Affected women receive special counselling on this.
- The blood sugar should be checked regularly to maintain a normal range.
- Only a few women with gestational diabetes have such persistently high sugar levels that they should inject insulin. If she gets insulin therapy, she should be measured her blood sugar more times a day (like more than four times a day)
- Other diabetes medications are not approved for pregnant women.
- Your doctor will check your baby’s growth and development via ultrasound.
- After giving birth, women with gestational diabetes will offer a repeat sugar test to be sure that blood sugar levels have returned to normal.
- No further treatment is then required.
- However, women with GD are more likely to develop type 2 diabetes later in life.
What are the preventive measures for gestational diabetes?
Prevention against GD consists of a healthy lifestyle. No specific, targeted measures are directed solely against GD.
- Prenatal care:You can lower your risk by eating a healthy diet before a woman gets pregnant, staying active and losing extra weight.
- Checking blood glucose: Pregnant women should take advantage of the tests for elevations in blood glucose. If risk factors are present, it recommends that the test will do at the first antenatal check-ups. Women without risk factors should take place between the 24th and 28th weeks of pregnancy.
- Nutrition: Being pregnant does not mean “eating for two”! However, experts do not advise pregnant women to fast. The risk of missing out on the necessary nutrients is too big. But pregnant women should only eat enough to avoid gaining excessive weight. Experts recommend cutting back on fatty foods and sweets and avoiding raw meat. On the other hand, fruits, vegetables, whole grains, and fish, which do not contaminate harmful substances, are beneficial.
- Excess weight: Too much padding on the abdomen increases the risk of GDM. During pregnancy, they should not gain weight beyond the usual limits. A suitable diet and exercise will help.
- Exercise: Physical activity stimulates circulation and improves oxygen supply and other bodily functions. There is evidence from studies that the frequency of complaints during pregnancy (e.g., back pain, constipation, varicose veins, mood swings) also decreases. The risk of premature birth is also said to reduce.
References
- Gestational Diabetes – Symptoms, Treatments | ADA
- Gestational diabetes – NHS (www.nhs.uk)
- Gestational Diabetes: Symptoms, Causes, Diet, Diagnosis, and Treatment (webmd.com)
- Gestational Diabetes | CDC
- Gestational diabetes – Symptoms and causes – Mayo Clinic