Introduction
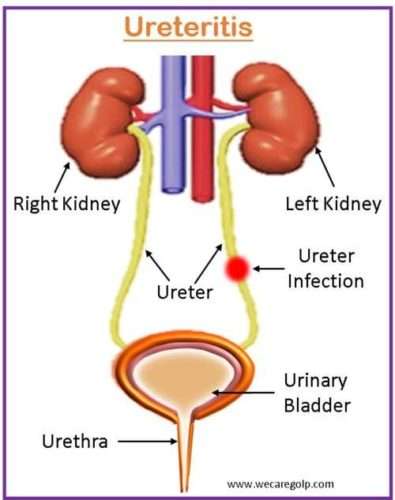
Ureteritis is defined as inflammation of the ureters, which is a tube that connects the kidneys to the bladder. The inflammation or infection of the ureters causes discomfort and various complications.
- One of the most prevalent etiologies of ureteritis is a bacterial infection which can cause inflammation of the ureters though the causes of ureteritis may differ depending on the individual case. The most prevalent cause of ureteritis is infection from concomitant cystitis.
- It is rare and indeed primary; however, it frequently arises from accompanying cystitis, descends from pyelonephritis, or is caused by direct dissemination from a nearby inflammatory disease like appendicitis or salpingitis. Through lymphatic spread, the infection may also enter the ureter, notably from the prostate and seminal vesicles.
- Any concomitant ureter abnormalities, such as stricture, megaloureter, ureterocele, and so on, will predispose to infective ureteritis.
Incidence
- Because of the rarity and the lack of established diagnostic criteria, the epidemiology of ureteritis is poorly understood.
- While data on the incidence and prevalence of ureteritis is lacking, it is thought to be a rather uncommon condition.
- It can occur alone or as part of a larger urinary tract infection (UTI), such as pyelonephritis (kidney infection) or cystitis (infection of the bladder).
Classification of Ureteritis
Based on cause
- Infectious vs non-infectious ureteritis: Bacteria, viruses, fungi, or parasites cause infectious ureteritis, whereas chemical irritants, radiation, or autoimmune diseases can cause non-infectious ureteritis.
- Primary vs secondary ureteritis: While secondary ureteritis can develop from an underlying ailment like bladder cancer, kidney stones, or a ureteral blockage, primary ureteritis is a solitary disorder.
Based on duration
- Acute vs chronic ureteritis: Acute ureteritis typically appears rapidly and fades within a few days or weeks, but chronic ureteritis can persist for months or even years.
Based on location
- Unilateral vs bilateral ureteritis: Bilateral ureteritis involves both ureters, whereas unilateral ureteritis only affects one.
- Obstructive vs non-obstructive ureteritis: Non-obstructive ureteritis develops when there is inflammation without blockage, whereas obstructive ureteritis occurs when there is an obstruction that stops urine from passing freely through the ureter.
Other Types
Eosinophilic ureteritis
- It is an uncommon ureter stenosis disorder.
- Flack discomfort and/or unilateral hydronephrosis can be caused by eosinophilic ureteritis.
- Pathological investigation reveals a significant infiltration of eosinophils into the submucosal layers.
- Eosinophilic ureteritis is an uncommon cause of ureteric stricture, which results in hydroureteronephrosis.
- The specific cause of this ailment is unknown. This disorder has been linked to atopy, hypereosinophilic syndrome, and previous ureteral operations.
Xanthogranulomatous ureteritis
- It is a chronic inflammatory disease in which foamy macrophages, multinucleated giant cells, and lymphocytes produce a benign granulomatous inflammation in the lamina propria.
- It is often misdiagnosed as a malignant tumor on computed tomography (CT) scan images, and the patient may be subjected to surgery, which might lead to difficulties.
Ureteritis cystica (UC)
- It is a benign disorder of the ureter that can resemble various conditions such as
- Transitional cell carcinoma,
- Blood clots,
- Air bubbles,
- Radiolucent stones,
- Fibroepithelial polyps, and
- Sloughed renal papillae.
- UC is distinguished radiographically by several tiny, round, lucent lesions that induce scalloping of the ureteral borders when seen in profile.
- Scalloping is caused by the protrusion of submucosal cysts into the lumen and is an essential distinguishing characteristic of this illness.
Causes of Ureteritis
- Infection
- Bacterial infection, with Escherichia coli.
- Other bacteria include Klebsiella, Proteus, and Pseudomonas.
- UTI is the leading cause.
- Gonorrhea and Chlamydia can also cause ureteritis.
- Obstructions like renal stones can block the ureter and cause inflammation.
- Trauma during catheterization or ureteroscopy
- Autoimmune disorders
- Systemic Lupus Erythematosus (SLE)
- Vasculitis
- Scleroderma
- Radiation therapy indicated for cancer treatment can cause inflammation of the ureters.
- Medications like cyclophosphamide and doxorubicin (Chemotherapy drugs) irritate the lining of ureters
Risk factors of Ureteritis
- Gender: Women are more prone than males to get ureteritis, presumably because of the shorter length of the female urethra and closer to the anus.
- Urinary system abnormalities: Any structural anomaly in the urinary tract, such as a small ureter or vesicoureteral reflux, might increase the chance of developing ureteritis.
- Weakened immune system: Individuals with compromised immune systems, such as those with HIV or undergoing chemotherapy, are more likely to develop ureteritis.
- Catheterization: Individuals with indwelling urinary catheters are more likely to develop ureteritis due to the introduction of germs into the urinary system.
- Previous UTI: Those who have previously had a UTI are more prone to develop ureteritis.
Signs and Symptoms of Ureteritis
- Flank pain
- Burning micturition
- Dysuria
- Urinary urgency
- Hematuria
- Fever and chills
- Nausea and vomiting
- UTI
Pathophysiology of Ureteritis
- An inflammatory reaction brought on by infection is characterized by the production of inflammatory mediators and the activation of numerous immune cells.
- Immune cells such as neutrophils, macrophages, and lymphocytes are drawn to the site of inflammation in response to an infection or damage. Pro-inflammatory cytokines, chemokines, and other mediators are released by these immune cells, which heighten the inflammatory response.
- Inflammation mediators like cytokines and chemokines activate immune cells and harm the ureteral epithelium, disrupting its barrier function.
- Key mediators in ureteritis include
- IL-6,
- IL-8,
- TNF-alpha, and
- Prostaglandins.
- The ureteral epithelium is important for separating urine and underlying tissues, but in ureteritis it becomes inflamed and damaged, making it less effective as a barrier.
- Bacteria and pathogens can enter the ureteral wall, causing inflammation.
- If untreated, complications include kidney damage, pyelonephritis, sepsis, scarring, and narrowing of the ureters. Chronic ureteritis can lead to hydronephrosis and renal failure.
Diagnosis of Ureteritis
Urinalysis
- For the detection of bacteria, the following tests in the urine are done which are possibly the signs of ureteral infection.
- White blood cells (WBCs)
- Red blood cells (RBCs)
Urine culture
- To determine the precise type of bacteria causing the infection, urine cultures require culturing any bacteria discovered in the urine in a lab.
- Making treatment decisions can be aided by this test.
Imaging tests
- For identifying signs of inflammation and other abnormalities, the following imaging tests can be indicated.
Cystoscopy
- In particular, the bladder, urethra, and ureteral apertures can be seen by the doctor during a technique called a cystoscopy, which allows them to examine the urinary system.
- Urinary tract problems might be discovered with the use of cystoscopy.
- This might involve early indications of
- Bleeding,
- Infection,
- Narrowing, or
- Malignancy.
Ureteroscopy (or ureterorenoscopy)
- It is the examination of the ureter and kidney’s interior (lumen).
- It is used to treat and analyze stones, tumors, and obstructions such as ureter constriction.
- It can also be used to investigate symptoms like
- Blood in the urine,
- Discomfort, or
- Abnormal cells in the urine.
Biopsy
- In certain circumstances, a biopsy of the ureter tissue may be required to determine the source of the inflammation.
- This entails extracting a tiny sample of tissue for laboratory examination.
- A surgical technique is required for ureteral retrograde brush biopsy.
- During the procedure, the surgeon will extract a tiny sample of tissue from the kidney or ureter lining.
Treatment of Ureteritis
Inflammation must be reduced, symptoms must be alleviated, and complications must be avoided as part of ureteritis therapy. Ureteritis is normally treated with a combination of medical and supportive interventions, which may include entailing pharmaceutical medication.
Medical Management
- Antibiotics: Depending on the type of bacteria implicated, an antibiotic may be prescribed, including amoxicillin, ciprofloxacin, or trimethoprim-sulfamethoxazole. Depending on the severity of the infection, antibiotics are normally administered for 7–14 days and can be taken orally or intravenously.
- Analgesics: Ureteritis frequently causes pain, which can be treated with analgesics such as acetaminophen or ibuprofen. Opioids are used if these analgesics are ineffective for the pain.
- Anti-inflammatory drugs: Corticosteroids administered intravenously/orally are used to reduce inflammation and relieve pain.
- Supportive measures:
- Bed rest,
- Hydration, and
- Avoiding activities that may exacerbate pain or discomfort.
Surgical Management
It is often treatable with medication and lifestyle modifications. In some cases, surgical management is required which are:
Ureteroscopy
- This minimally invasive treatment looks into the ureter and removes any stones or blockages that may be the source of the inflammation.
- It employs a tiny, flexible tube called a ureteroscope.
- The ureteroscope is placed into the ureter after passing through the bladder and urethra.
- After the scope is in position, the surgeon can use tiny tools inserted via the scope to remove the impediment or stone.
Ureteral stenting
- To aid in the movement of urine from the kidney to the bladder, a thin, flexible tube known as a ureteral stent is inserted into the ureter.
- A cystoscope or ureteroscope is used to place the stent via the urethra, bladder, and into ureter.
- The stent permits urine to flow and relieves any blockage or irritation.
Pyeloplasty
- This surgical technique is used to treat a ureteropelvic junction that is obstructed or damaged.
- The damaged part of the ureter is removed during a pyeloplasty, and the junction is then rebuilt to facilitate the free passage of urine.
Nephrectomy
- In some instances, a severely damaged or inflamed kidney may be the cause of ureteritis.
- Nephrectomy, a surgical operation, may be required in certain situations to remove the damaged kidney.
- Typically, laparoscopic surgery or robotically assisted methods are used for this procedure.
Ureteroureterostomy
- This operation involves joining two ureter segments together.
- When a section of the ureter has been removed because of an accident, illness, or blockage, this surgery is indicated.
Complications of Ureteritis
- UTIs: Ureteritis can result in a buildup of germs in the ureter, which can cause a UTI. Untreated UTIs can spread to the kidneys and result in more severe consequences.
- Renal failure: Ureteritis may result in kidney inflammation and damage. This can result in scarring, decreased kidney function, and possibly renal failure if left untreated.
- Hydronephrosis: This disorder causes urine to build up in the kidneys as a result of an obstruction in the ureter. The kidney may get swollen and suffer harm as a result. Ureteritis is one of several diseases that can lead to hydronephrosis.
- Kidney stones: Ureteritis can result in the production of urine crystals, which can result in kidney stones.
- Sepsis-causing septicemia: Untreated ureteritis can result in septicemia which can result in organ failure, shock, and even death.
Prevention
- Maintaining good hygiene helps to lower the risk of bacterial infections. This entails often washing hands, particularly before and after using the restroom, and after touching any possibly contaminated surfaces.
- Stay hydrated, drinking plenty of water will reduce the risk of stone formation. Avoid caffeinated drinks and alcohol.
- Maintain a healthy diet by including fruits, lean proteins, and whole grains in the diet and limiting the intake of processed food, and saturated fats.
- Exercising frequently can help avoid infection as well as other health issues including kidney stones.
- Holding in urine might raise the risk of ureteritis and UTIs. Instead of prolonging toilet breaks, people should aim to urinate as soon as they feel the desire.
Prognosis
- Usually, the prognosis is favorable with early diagnosis and treatment.
- Most cases can be treated effectively with antibiotics within a few days to weeks.
- However, if the infection is not treated or if it spreads to the kidneys, it may result in more serious complications like kidney infection (pyelonephritis) or even damage to the kidneys.
- The prognosis may depend on addressing the underlying cause and managing related symptoms if it is caused by other factors, such as chemical irritability, radiation, or other underlying conditions.
Summary
- Ureteritis is a rare condition that involves inflammation of the ureters.
- It can be caused by a variety of factors, including bacterial or viral infections, autoimmune disorders, and radiation therapy.
- Symptoms include pain in the abdomen or lower back, fever, and changes in urinary patterns (increased frequency or urgency to urinate).
- Diagnosis involves physical examination, imaging tests such as CT scans or ultrasounds, and urine or blood tests to identify potential infections or underlying conditions.
- Treatment includes supportive, medical, and pharmaceutical interventions (antibiotics, analgesics, corticosteroids). In rare cases, surgical interventions may be indicated.
References
- Bajracharya, U. B., Sah, A. K., Baral, H., Sigdel, G., Shrestha, G. K., & Adhikari, R. (2021). Eosinophilic Ureteritis Causing Ureterohydronephrosis: A Case Report. Medical Journal of Shree Birendra Hospital, 20(2), 170-172. https://doi.org/10.3126/mjsbh.v20i2.36632
- El-Reshaid, K., Abdelhafez, A. A., & Hussein, S. (2022). Recurrent and Extensive Idiopathic Granulomatous Ureteritis: A Localized Hyperimmune Disease with Genetic Predisposition. Open Journal of Nephrology, 12(1), 87-92. 10.4236/ojneph.2022.121008
- Giambroni, L., Monticelli, L., Simeone, C., & Frego, E. (1993). Ureteritis. Archivio Urological, Nephrological, and Andrological Sciences, 65(1), 31-33. https://europepmc.org/article/med/8475390
- Nagamura, N., & Sugitani, T. (2022). A case of ureteral stenosis due to ureteritis probably associated with rheumatoid arthritis. Modern Rheumatology Case Reports, rxac071. https://doi.org/10.1093/mrcr/rxac071
- Neretljak, I., Orešković, J., Šktrić, A., Kavur, L., & Sučić, M. (2019). Ureteritis cystica-a rare urological condition. Urology Case Reports, 24, 100866. https://doi.org/10.1016/j.eucr.2019.100866
- Remigio, P., Ramos, C., & Basirico, P. (1975). Xanthogranulomatous ureteritis. The Journal of Urology, 114(4), 621-623. https://doi.org/10.1016/S0022-5347(17)67101-5