Introduction
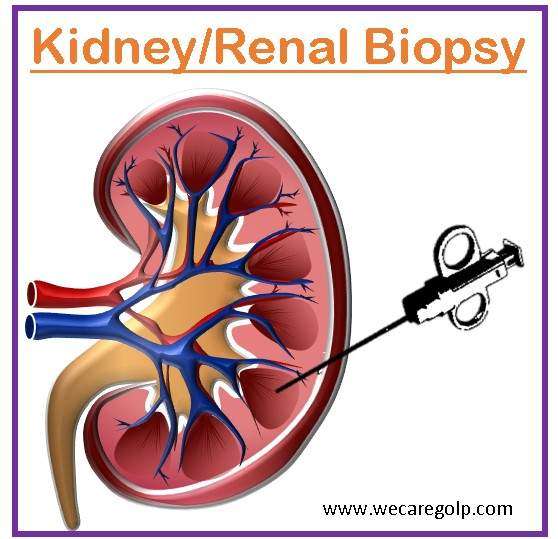
A kidney (renal) biopsy is an invasive diagnostic technique that is performed to collect a segment of renal tissue, generally with the use of a needle or similar surgical tool. In patients with the renal parenchymal disease, kidney biopsy continues to be the gold standard for diagnosis, treatment, and prognosis prediction.
- Usually, a needle is used to puncture the skin and enter the kidney to collect the sample.
- Kidney biopsies are carried out to identify several kidney illnesses, including chronic kidney diseases, kidney cancer, glomerulonephritis, and nephrotic syndrome.
- Percutaneous and laparoscopic/open biopsy are the two basic types of biopsies. When a patient requires a combined liver/kidney biopsy, a transjugular kidney biopsy is usually done.
Indications of Kidney Biopsy
- Proteinuria
- Persistent severe proteinuria, greater than 1 g/1.73 m2 per day (exception – a child with a typical steroid-sensitive nephrotic syndrome)
- Proteinuria accompanied with abnormalities in urine sediment. When proteinuria and abnormalities in the urine sediment are present together, renal biopsy is more likely to be diagnostic than when either proteinuria or hematuria is present alone.
- Reduction in glomerular filtration rate (GFR).
- Renal biopsy is required when the GFR is less than 80 ml/1.73 m2/min.
- In this situation, the GFR needs to be checked again in a month, and if it stays low, a kidney biopsy is necessary.
- The child recuperating from acute glomerulonephritis is the exception (e.g., postinfectious glomerulonephritis).
- Unknown cause of acute kidney injury (AKI)
- Unknown cause of chronic kidney disease (CKD)
- Glomerulonephritis
- Abnormal blood test results
- Persistent low complement component 3 (C3) levels for more than three months. (A biopsy is not necessary if the C3 level is low during the acute stage of postinfectious glomerulonephritis.)
- Unexplained hematuria (the cause cannot be identified by other tests)
- Nephrotic syndrome
- Rapidly declining kidney function
- Kidney transplantation (to see how the transplanted kidney works)
- Kidney transplant rejection (to detect the reason)
- Acute nephritic syndrome
- Renal tumors
- Autoimmune diseases
- Systemic lupus erythematosus (SLE)
- Henoch-Schönlein purpura (IgA vasculitis)
- ANCA-positive vasculitis
Contraindications of Kidney Biopsy
Absolute contraindications
- Uncorrectable bleeding diathesis
- Uncontrollable severe hypertension
- Active urinary tract infection/ renal or perirenal infection
- Skin infection at the biopsy site
- Solitary kidney
- Severe anemia
- Horseshoe kidney (renal fusion)
- Pyelonephritis (kidney infection)
- Hydronephrosis (urine flow obstruction from the kidney)
Relative contraindications
- Advanced age
- Obesity
- Multiple renal cysts
- Retrorenal colon
- Highly vascularized tumors (increased risk of bleeding)
- Pregnancy
- Renal failure
- Uncooperative patient
- Anatomic abnormalities of the kidney that may increase the risk
- Small kidneys (<8 cm on ultrasound)
Types of Kidney Biopsy
Percutaneous renal biopsy
- A required procedure for making a final diagnosis and determining the prognosis of renal parenchymal disorders is a percutaneous renal biopsy (PRB) and histological analysis.
- This sort of renal biopsy, which is the most frequent, entails passing a needle through the skin and into the kidney to collect a tissue sample.
- Often, local anesthetic is used during this process, and ultrasound or CT imaging is used to guide the biopsy needle placement to assure accuracy.
- In an outpatient treatment that normally takes less than an hour, a percutaneous renal biopsy can be done.
Open renal biopsy
- An incision must be made in the skin and muscle for this sort of renal biopsy to expose the kidney and collect a tissue sample.
- Typical indications of open renal biopsy are
- No possibility of a percutaneous biopsy
- Requirement for a bigger tissue sample
- In contrast to percutaneous biopsy, this operation is often carried out under general anesthesia and may result in a lengthier hospital stay and recuperation period.
Transjugular renal biopsy
- An appropriate tissue sample for a histopathologic diagnosis of renal dysfunctions can be obtained by transjugular renal biopsy.
- It is often carried out on high-risk individuals when percutaneous kidney biopsy is either impractical or dangerous.
- This is especially helpful in individuals who are extremely obese because a traditional percutaneous kidney biopsy may be challenging in these cases.
- A needle is inserted into the kidney during this type of renal biopsy through the jugular vein in the neck.
Laparoscopic renal biopsy
- If a percutaneous biopsy is not an option for a patient, laparoscopic renal biopsy is a safe and efficient alternative to open renal biopsy.
- A laparoscope, a small, flexible tube with a camera and light, and a biopsy needle are inserted via tiny abdominal incisions during this form of renal biopsy to collect a tissue sample from the kidney.
- Although it is a less invasive process that may be completed as an outpatient procedure, laparoscopic renal biopsy is not frequently employed for renal biopsy.
Procedure
Patient preparation
- Encourage patients to express any questions or worries they may have regarding the biopsy.
- The patient should sign the consent form for the procedure where the risks and benefits of the procedure are explained clearly.
- Ask them to bring a list of all their prescription and over-the-counter medications, as well as any vitamins or other dietary supplements.
- Maintain blood pressure if the patient is hypertensive.
- Inform patients that they might need to temporarily cease (7 days before the procedure) taking aspirin, NSAIDs, and anticoagulants (drugs that thin the blood) to avoid complications.
- Blood tests are done for the safety of the patient
- Renal function test
- Hemoglobin
- Blood grouping
- Complete blood count
- Clotting factors (PT-INR, APTT, bleeding time, and clotting time)
- Patients should fast for eight hours before the biopsy to reduce the risk of aspiration during the procedure.
During the Procedure
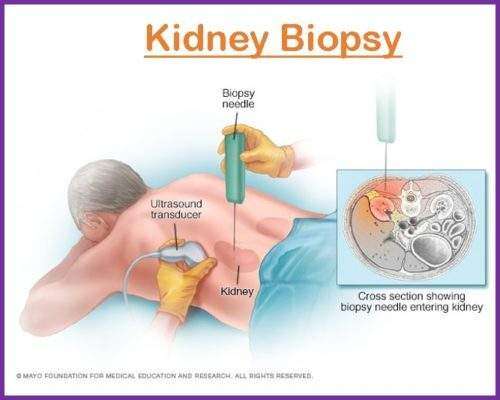
Step 1: Patient Positioning
- The patient is positioned prone, typically with a cushion or towel positioned beneath the abdomen to ensure proper placement.
- The biopsy for the transplant graft is carried out when the patient is supine, depending on whether the kidney is transplanted into the right or left lower quadrant.
- An antiseptic solution is used to clean the biopsy site, and sterile towels are used to cover the area.
Step 2: Administration of Local Anesthesia
- It is conducted with 1% lidocaine under a local anesthetic.
- The skin and subcutaneous tissue surrounding the biopsy site are given local anesthetic.
- Typically, the needle is inserted immediately laterally into the spinous process of the spine, in the lower pole of the kidney.
Step 3: Needle Insertion
- Via the epidermis and subcutaneous tissue, a biopsy needle—typically a 16- or 18-gauge needle—is inserted and moved toward the kidney.
- To guarantee precise placement, the needle is guided by ultrasonography or CT.
- After the needle tip is within the renal cortex, quickly advancing and retreating the needle is required to retrieve a specimen.
Step 4: Specimen Handling
- The tissue is processed and examined in the pathology laboratory after being immersed in a fixative solution.
- If more than one biopsy sample is required, the procedure is repeated.
Step 5: Pressure and bandaging
- Following the completion of the biopsy, the doctor will withdraw the needle, apply pressure to the biopsy site to tamponade any potential bleeding, and then wrap the area in a bandage.
- To aid in halting any bleeding, pressure is administered to the biopsy site. The area is covered with a sterile bandage or dressing.
After the Procedure
- Immediately following the surgery, the patient should normally spend 6 to 8 hours in a supine position in bed. The patient should prepare to stay in the hospital for a minimum of 12 hours and maybe for one night following the surgery.
- At this time, the patient will get the appropriate pain medication, have his or her urine tested for blood, and have their blood counts and vital signs/complications (infection and bleeding) monitored throughout their hospital stay.
- After the biopsy, patients should drink a lot of fluids to help flush out any leftover contrast dye and lower the risk of problems.
- For a few days following the surgery, patients should refrain from intense exercise and heavy lifting. Also, they shouldn’t drive for at least 24 hours following the biopsy.
Advantage of Kidney Biopsy
- A kidney biopsy can assist in the identification of several renal conditions, including glomerulonephritis, nephrotic syndrome, and lupus nephritis. For the right kind of treatment, an accurate diagnosis is required.
- The outcomes of a kidney biopsy can inform decisions about therapy, such as selecting the best drug or figuring out if a patient qualifies for a kidney transplant.
- It can be done to track the development of the illness over time and evaluate the efficacy of therapy. It carries a minimal risk of significant consequences, and the majority of patients only feel minor discomfort or pain while undergoing the surgery. useful for patients with kidney disease.
- It may be used to assess the degree and amount of kidney damage, which can be useful for patients with kidney disease, especially for chronic kidney disease.
Complications of Kidney Biopsy
- Bleeding: With a reported frequency of 1-6%, bleeding is the one of the major and common complication of kidney biopsy. People who have an increased risk of bleeding are
- Those with bleeding problems
- Uncontrolled hypertension
- Those on blood thinners
- Pain: The location of the biopsy frequently experiences pain, which typically lasts a few days. Pain can be treated with analgesics, but it may also necessitate a few days of rest and reduced activity.
- Hematoma: Hematoma can be present in the location of the biopsy and result in
- Bruising,
- Discomfort, and
- Edema.
- Infection: An infection is uncommon. It may require antibiotic treatment. Indications of infection are
- Fever
- Chills
- Escalating pain
- Redness at the biopsy site
- Arteriovenous fistula: This uncommon problem occurs when an artery and vein join improperly. High blood pressure and heart failure can result from blood bypassing the capillaries. Quick medical intervention is necessary for this problem.
- Allergic reaction: A small number of individuals might experience an allergic response to the local anesthetic or other drugs used in the treatment. Immediate medical intervention is necessary when an allergic reaction arises. Symptoms of an allergic response are
- Itching
- Redness
- Breathing issues
Methods for Kidney Biopsy Tissue Examination
Gross examination
- It is the initial step in interpreting a kidney biopsy.
- To determine the size, color, consistency, and presence of any aberrant lesions, the biopsy tissue is inspected macroscopically.
Light microscopy
- After processing and staining, the tissue sample is examined using a light microscope.
- This method evaluates the architecture of the renal tissue as a whole and identifies any aberrant formations.
- Light microscopy analysis can detect the presence of fibrosis, inflammation, and abnormalities in the glomeruli or tubules.
Immunofluorescence
- In immunofluorescence, certain antibodies are used to bind to particular proteins in the kidney tissue.
- This method aids in determining the precise form of kidney illnesses such as glomerulonephritis.
- Moreover, immunofluorescence can show up where immune complexes and complement elements have been deposited in kidney tissue.
Electron microscopy
- The kidney tissue is examined in more detail using electron microscopy.
- This method aids in locating ultrastructural irregularities in kidney tissue.
- The glomerular basement membrane, podocyte foot processes, and endothelial cells can all be observed under electron microscopy for changes.
Integrated approach
- The analysis of the kidney biopsy results goes beyond only looking at its constituent parts.
- To provide a final diagnosis, the integrative technique considers the results from light microscopy, immunofluorescence, and electron microscopy together.
- This method aids in identifying the precise form of glomerulonephritis or other renal illnesses and in directing the proper course of action.
Interpretation of Kidney Biopsy
The Banff Classification
- It is a method for analyzing the findings of kidney biopsies. It is used for native kidney biopsies as well as for the diagnosis and classification of rejection following kidney transplantation.
- Kidney biopsy sample interpretation is standardized by the Banff Classification, which aids in the determination of a diagnosis, prognosis, and course of therapy. It is employed by pathologists and physicians all over the world to guarantee precision and consistency in the interpretation of kidney biopsy data.
- When grading renal biopsies, the Banff system takes into account many variables, such as the kind and intensity of inflammation, damage to the kidney tissue, and the existence of additional abnormalities. The following are the primary divisions of the Banff system:
- T Cell-Mediated Rejection (TCMR): This group includes biopsies that exhibit signs of immune cells (T cells) attacking kidney tissue.
- Antibody-Mediated Rejection (ABMR): Biopsies that exhibit signs of antibodies attacking kidney tissue fall under this category.
- Interstitial Fibrosis and Tubular Atrophy (IFTA): IFTA includes biopsies that exhibit signs of scarring and damage to the kidney tissue.
- Glomerular Lesions: Biopsies that demonstrate injury to the small blood arteries (glomeruli) in the kidney are included in this group.
- Vascular Lesions: Biopsies that reveal injury to the major blood arteries in the kidney fall under this group.
- Additional Findings: Biopsies that reveal further abnormalities, such as tumors or infections, go under this category.
| Categories | Findings |
| Category 1 | Normal biopsy or nonspecific changes |
| Category 2 | Antibody-mediated changes |
| Category 3 | Borderline/suspicious for acute T cell-mediated rejection |
| Category 4 | T-cell mediated rejection |
| Category 5 | Interstitial fibrosis and tubular atrophy |
| Category 6 | Other non-rejection changes |
Grades are used to further differentiate each category, with higher grades denoting more serious illnesses. The Banff method is widely applied in clinical practice and scientific investigation to direct treatment choices and standardize kidney biopsy reporting.
Summary
- A kidney or renal biopsy is a medical procedure in which a tiny sample of kidney tissue is removed for microscopic analysis. Typically, it is done to identify kidney disease, quantify how bad the problem is, and inform therapy choices.
- A needle is often injected through the skin into the kidney to do the biopsy while under local anesthetic. Ultrasound or CT imaging is used to guide the needle to ensure accuracy and lower the chance of problems.
- A pathologist examines the tissue sample after it has been taken to look for any abnormalities or kidney damage under a microscope. The outcomes of the biopsy can be used to identify glomerulonephritis, lupus nephritis, or diabetic nephropathy as the primary causes of kidney illness.
- Renal biopsy complications are uncommon but might include bleeding, infection, and disruption to adjacent tissue. Following the surgery, patients are often closely watched and may need to spend the night in the hospital for observation.
- Overall, renal biopsy is a useful technique for identifying and treating kidney illness and may assist medical professionals in creating individualized treatment schedules that are catered to the unique requirements of each patient.
References
- Charbel, C. E. (2020). Renal Biopsy. Medscape. Retrieved on 2023, Feb 22 from https://emedicine.medscape.com/article/2093338-overview
- Fogo, A. B. (2003). Approach to renal biopsy. American Journal of Kidney Diseases, 42(4), 826-836. https://www.ajkd.org/action/showPdf?pii=S0272-6386%2803%2901054-0
- Ghimire, M., Pahari, B., Paudel, N., Das, G., Das, G. C., & Sharma, S. K. (2014). Kidney biopsy: An experience from tertiary hospital. Journal of Nepal Medical Association, 52(193), 707-12. https://pdfs.semanticscholar.org/6f27/73e5e4d0252505d95224539a9661dc89ed56.pdf
- Korbet, S. M. (2002, May). Percutaneous renal biopsy. In Seminars in nephrology, 22(3), pp. 254-267. WB Saunders. https://doi.org/10.1053/snep.2002.31713
- Lefaucheur, C., Nochy, D., & Bariety, J. (2009). Renal biopsy: procedures, contraindications, complications. Néphrologie & Thérapeutique, 5(4), 331-339. Doi: 10.1016/j.nephro.2009.02.005
- National Kidney Foundation. (2022). Kidney biopsy. https://www.kidney.org/atoz/content/kidney-biopsy
- Visconti, L., Cernaro, V., Ricciardi, C. A., Lacava, V., Pellicanò, V., Lacquaniti, A., … & Santoro, D. (2016). Renal biopsy: Still a landmark for the nephrologist. World journal of nephrology, 5(4), 321. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4936339/pdf/WJN-5-321.pdf
- Walker, P. D. (2009). The renal biopsy. Archives of pathology & laboratory medicine, 133(2), 181-188. https://www.arkanalabs.com/wp-content/uploads/05/23/The-Renal-Biopsy.pdf
- Walker, P. D., Cavallo, T., & Bonsib, S. M. (2004). Practice guidelines for the renal biopsy. Modern Pathology, 17(12), 1555-1563. https://www.nature.com/articles/3800239