Introduction
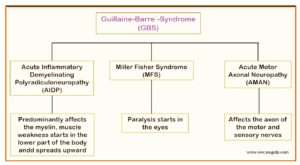
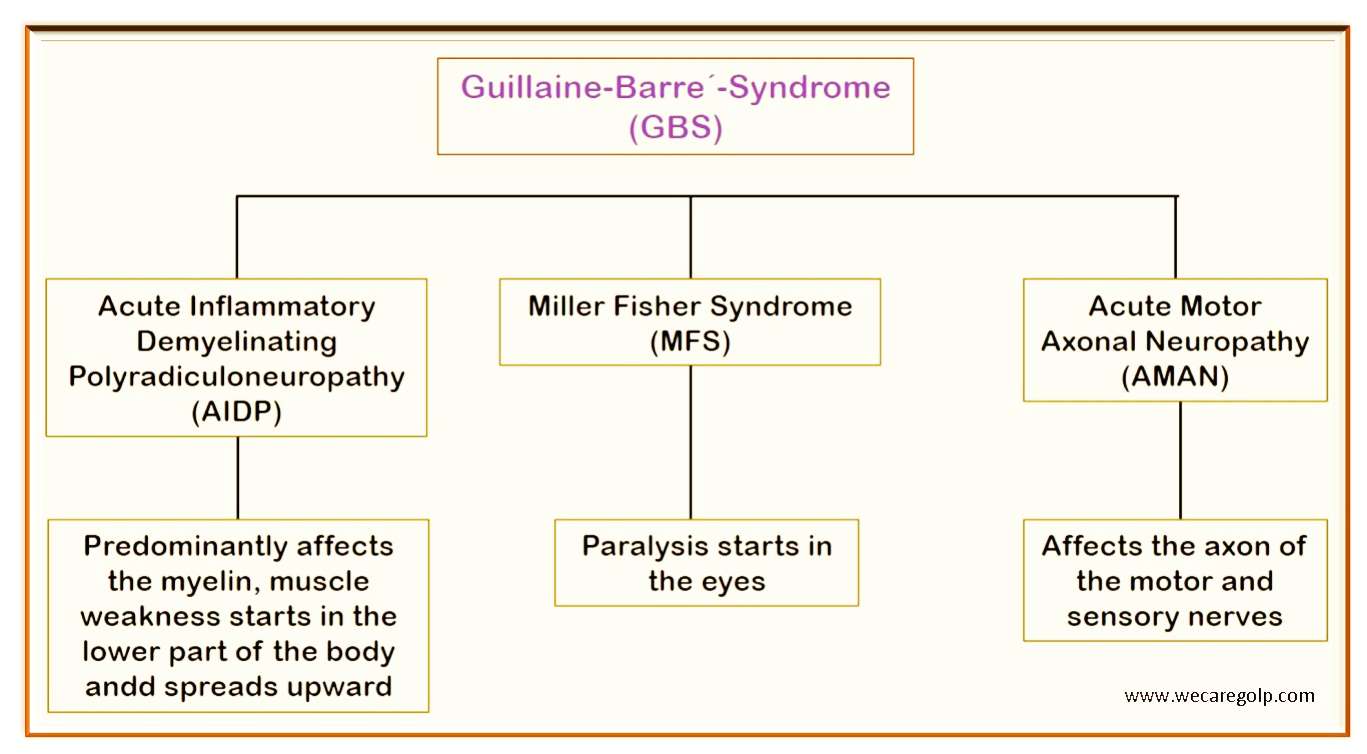
Guillain-Barré syndrome (GBS) is a type of polyneuropathy, affects many peripheral nerves throughout the body that causes muscle weakness. This weakness usually gets worse over a few days to weeks. If the disorder is treated, it will usually heal more quickly.
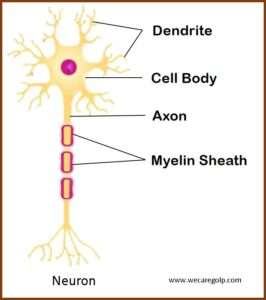
- It is an autoimmune reaction in which the body´s own immune defense system (antibody) attacks the patient´s nerves.
- The body´s immune system attacks either the myelin sheath (which surrounds the nerves and enables the rapid transmission of nerve signals) or sometimes even the axon (the inner covered part of the nerve), causing paralysis and muscular weakness as well as strange sensations.
- The first symptoms of weakness usually appear in both legs and spread upwards onto the body.
- The weakness caused by Guillain-Barré syndrome (GBS) usually increases within 3 or 4 weeks, then stays the same or goes back until it is completely gone. If this weakness increases for more than eight weeks, it is not a sign of GBS, but a chronic inflammatory demyelinating polyneuropathy (CIDP).
- GBS can affect all age groups. But the risk increases as you age. It´s also more common in males than females.
Symptoms of GBS
The clinical picture is very diverse. The severity depends mainly on which nerves are affected. Typically, the symptoms often begin in the legs and appear symmetrically on both halves of the body. Common complaints include:
- General weakness, especially muscle weakness
- Unsteady walking, numbness or tingling sensation in the feet
- Severe pain that may be worse at night
- Sensory disturbances, coordination problems and symptoms of paralysis in the legs
- Numb feeling in hands and arms without loss of mobility, but sometimes with uncontrolled movements
- Visual disturbances, double vision and impaired eye mobility (e.g., inability to close the eyelid, failure of the blink reflex with the risk of dehydration)
- Difficulty speaking, chewing and swallowing
- Rapid heart rate
- Low or high blood pressure
- Breathing disorders
Causes of GBS
The causes are still unknown. Many cases occur within a few days to weeks after an infectious disease such as a common cold, sore throat or gastrointestinal infection with diarrhea. Insect bites and operations are also suspected to be triggers. GBS is not contagious.
- In about two-thirds of affected patients, symptoms of GBS begin within about five days to three weeks of a mild infection (such as a campylobacter infection, mononucleosis, or other viral infection), surgery or vaccination.
- Some patients develop GBS after being infected with the Zika virus or as a result of COVID-19.
Risk Factors
- Campylobacter infection is most common (food poisoning)
- Zika virus and dengue
- Cytomegalovirus (may cause no symptoms)
- Epstein-Barr virus, which causes infectious mononucleosis, or glandular fever
- Influenza virus
- COVID-19 virus
- Hepatitis A, Hepatitis B, Hepatitis C, and Hepatitis and E
- HIV
- Mycoplasma pneumonia (can infect respiratory tract)
- Surgery
- Trauma
- Hodgkin’s lymphoma
- Influenza vaccinations or childhood vaccinations (rare)
- COVID-19 Johnson & Johnson vaccine
Diagnosis of GBS
There are several diseases with similar symptoms. Therefore, it is quite difficult to diagnose. With signs and symptoms, the doctor can take a medical history and do a physical examination.
Diagnostics findings include:
- Lumbar Puncture (LP): A lumbar puncture is a procedure to draw some fluid around the spinal cord (the nerves running up the spine) using a needle inserted into the lower part of the spine. A high protein content with a simultaneous deficiency of lack of white blood cells (WBCs) in the cerebrospinal fluid suggests Guillain-Barre´-Syndrome.
- Electromyography (EMG): Tiny needles insert into muscles, electrical recordings take to see how they react when nearby nerves are activated.
- Nerve conduction studies: Small discs (electrodes) are stuck on the skin, minor electric shocks use to activate the nerves and measure how quickly these signals travel along with them.
Treatment of GBS
There is no exact cure for GBS. But the supportive treatment can help manage it. These treatments shorten the hospitalization period, speed up the healing process and reduce the risk of permanent disability and death. The options of treatment include:
Intravenous Immunoglobulin (IVIG)
- Immunoglobulins are proteins that develop from healthy donor antibodies. When patients with GBS treat with IVIG, the result can be a lessening of the immune attack on the nervous system. IVIG infusion administers early and intravenously, usually every day for five days.
- If treatment with immunoglobulin is ineffective, plasma exchange is performed.
Plasmapheresis
- Plasmapheresis (plasma exchange) is a procedure that removes and replaces plasma.
- Plasma exchange will perform as soon as possible if the patient’s condition is deteriorating rapidly.
- It is an alternative to IVIG where plasma removes from the blood cells through a plasma separation machine. The separated plasma through away, the blood cells return to the body with new fresh frozen plasma. It allows the body to regenerate its plasma.
Management
The disease can progress very quickly. There is a risk of respiratory failure and heart failure, sometimes within a few hours. It is therefore essential that the treatment is carried out in an intensive care unit (ICU) for the first few days.
- Painkillers and blood clots preventing medications may need while the patient is immobile.
- When symptoms are severe, a person may need help with breathing, a heart monitor, and help prevent saliva or food from entering their airways.
- Patients with weak facial and swallowing muscles must be fed artificially intravenously (intravenous feeding) or using a tube (PEG tube).
- Fluid can be administered intravenously.
- In order to prevent bedsores and pressure sores, the patients are therefore placed on special mattresses and the severely affected is moved to a different position every two hours.
- Physiotherapy is performed to prevent contractures and to maintain joint and muscle function and mobility.
References
- Guillain-Barré syndrome – Better Health Channel
- Guillain-Barré syndrome: Symptoms, causes, diagnosis, and treatment (medicalnewstoday.com)
- Guillain-Barre Syndrome: What It Is and How It’s Treated (webmd.com)
- Guillain-Barré Syndrome: Symptoms, Vaccine, Treatment & More (healthline.com)
- Guillain-Barré syndrome – NHS (www.nhs.uk)
- Guillain-Barré Syndrome Fact Sheet | National Institute of Neurological Disorders and Stroke (nih.gov)
- Guillain-Barre syndrome – Symptoms and causes – Mayo Clinic
- Guillain-Barré Syndrome | Campylobacter | CDC

Thanks for your blog, nice to read. Do not stop.