Introduction
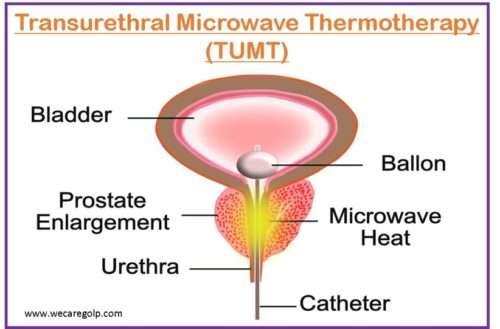
Transurethral microwave thermotherapy (TUMT) is one of the minimally invasive procedures that use microwave radiation to produce coagulation necrosis in prostatic tissue.
- TUMT involves inserting a specially designed urinary catheter into the bladder, enabling a microwave antenna to be positioned into the prostate, where it heats and removes hyperplastic prostate tissue.
- The purpose of TUMT is to give a one-time effective treatment for lower urinary tract symptoms (LUTS) caused by benign prostatic hyperplasia (BPH) as an alternative to medication, transurethral resection of the prostate (TURP), transurethral needle aspiration (TUNA), photoselective vaporization of the prostate (PVP), open prostatic enucleation, or other surgical procedures.
- In comparison to the long-established surgical gold standard, TURP, a growing body of research shows that TUMT is somewhat inferior in terms of symptom reduction and retreatment rate, but superior in terms of major perioperative adverse events.
Indications of TUMT
Persons with moderate to severe voiding symptoms due to BPH, those experiencing side effects from medical therapy, those who have failed medical therapy, and those who choose not to be treated medically are all candidates for TUMT.
Absolute indications
- Urinary retention unresponsive to medical therapy
- Detrusor decompensation
- Chronic retention of urine
Relative indications
- Repeated acute retention of urine
- Bladder stones
- Recurrent urinary infections
- Recurrent or persistent gross hematuria
Contraindications of TUMT
- Active urinary tract infections (UTIs)
- Known or suspected prostate or urothelial cancer
- Neurogenic bladder voiding dysfunction
- History of TURP or pelvic trauma (may cause potential alterations in pelvic anatomy)
- Metallic implants
- Penile prosthesis
- Severe urethral stricture disease
- Leriche syndrome
- Severe peripheral vascular disease,
- A pacemaker or defibrillator
Procedure
Transurethral microwave thermotherapy is a non-surgical, minimally invasive therapy that may be administered as an outpatient under local anesthesia.
Patient’s Preparation
- All patients who are candidates for TUMT must undergo a complete history and physical assessment. The existence, start, progression, and severity of LUTS should be included in the current disease history.
- The patient’s urologic history (including sexually transmitted illnesses, stones, trauma, and bladder function) should be included in the prior medical history, as well as any other concurrent medical conditions (e.g., diabetes).
- Patients should be advised about the risks, advantages, alternatives, and expected outcomes before undergoing TUMT. Specific procedures and manufacturer instructions vary for each TUMT equipment and must be strictly adhered to.
- Medicines containing alpha sympathomimetics, such as cold medicines, may produce symptoms of bladder outlet blockage and should be avoided wherever feasible.
- The patient should be checked for dilated bladder, urethral meatal stenosis, and nodularity in particular. Rectal tone, prostatic size, consistency, and landmarks should all be evaluated.
- Lab tests like urinalysis, BUN level, renal function test, prostate-specific antigen, transrectal USG, renal USG, voiding velocity, post residual volume, and cystourethroscopy should be performed before the procedure.
- The patient should avoid food and drink for six hours prior to the procedure to prepare for anesthesia.
During Procedure
- All patients get proper antibiotic therapy prior to surgery, and an analgesic (e.g., ibuprofen, ketorolac, morphine) and anxiolytic (e.g., benzodiazepine) may be offered.
- An antiseptic solution is used to clean the penis, and 10-20 mL of 1-2% lidocaine gel is used to anesthetize the urethra.
- The treatment catheter is then correctly positioned following the standards.
- TUMT involves inserting a tool (called an antenna) that emits microwave radiation via the urethra to a site inside the prostate. The interior of the prostate is then heated using microwave radiation.
- To prevent heat from injuring the urethral wall, a cooling fluid is pumped around the microwave antenna.
- During the procedure, a temperature sensor is put into the patient’s rectum to prevent the temperature from rising too high outside the prostate. If the temperature in the rectum becomes too high, the therapy is immediately shut off until the temperature falls.
- The temperature inside the prostate rises to the point that some of the tissue is killed. As this region of the prostate recovers, it shrinks, minimizing urine flow obstruction.
- Patients may suffer minor perineal warmth, discomfort, and urine urgency during any TUMT operation. Pain is rarely severe enough to necessitate discontinuing treatment.
Aftercare
- The prostate and urethra will need to heal for a few days before voluntary urination may be resumed. The patient may be catheterized during this period to allow the urinary system and prostate to recover.
- The body will need time to reabsorb the treated prostatic tissue, and it normally takes six to twelve weeks for BPH symptoms to improve. The ultimate objective of TUMT is to provide long-term relief from BPH symptoms while minimizing adverse effects.
- The International Prostate Symptom Score, which includes a quality-of-life assessment, is frequently used to quantify symptoms and track therapy progress. Convalescence is generally quick, with most patients able to urinate and a typical recovery period at the home of fewer than five days.
- However, prostatic edema is to be expected during microwave treatment, which might increase the risk of urinary retention.
- When compared to a Foley catheter, the stent is worn for 30 days and allows the patient to have volitional voiding with enhanced quality of life.
- Most patients can be discharged the same day, but they must be catheterized for at least 1-3 days, or until the swelling in the urethra has subsided. While some procedures recommend retaining a Foley catheter in all patients for up to two weeks, other urologists prefer to put in a temporary prostatic stent after the first week of therapy.
- Some frequent TUMT side effects that disappear on their own after a few days are:
- Urine with blood or blood clots
- Irritation or burning feeling at the penile tip
- Urinary control is temporarily lost.
- Infections of the urinary tract
Over the next several weeks, the body absorbs the enlarged prostate tissue that was killed during the treatment, and the urine symptoms cure themselves.
Benefits of TUMT
- Even individuals with bleeding/clotting issues can safely have the operation done because there are no incisions made.
- The patient does not need to stay in the hospital for even one day because it is an outpatient treatment.
- TUMT has a decreased risk of inducing dry orgasms or retrograde ejaculation because it is less likely to result in urethral scarring or stricture development.
- The likelihood of bleeding or other comparable problems following TUMT surgery is also decreased.
- TUMT is generally considered a safe procedure with a low risk of side effects.
Risks of TUMT
Prostatitis
- TUMT can sometimes cause persistent inflammation inside the prostate called prostatitis.
- Inflammation can induce symptoms such as frequent or urgent urine, as well as painful urination.
Urination difficulties
- As the bladder and urethral muscles adjust to the reduced quantity of prostate tissue, the patient may have certain urination difficulties, such as difficulty regulating urine flow, continual dribbling of urine, and so on.
- Catheterization is used to treat these symptoms, which usually go away within a few days.
Urinary tract infections (UTIs)
- UTIs are typical consequences of urinary surgeries, especially if the patient requires extended catheterization.
Re-treatment
- TUMT has lower efficacy in treating urinary symptoms, particularly in individuals with large prostate glands.
- The patient may require re-treatment with another BPH therapy.
Summary
- TUMT is a non-ablative minimally invasive therapeutic option that may be conducted in an outpatient clinic without the need for anesthesia or the additional difficulties associated with traditional surgical treatments such as transurethral electro-resection of the prostate (TURP).
- TUMT is used to treat the symptoms of benign prostatic hyperplasia. It is an alternative for men who desire more than just medications to alleviate their issues.
- TUMT involves inserting a tool (called an antenna) that emits microwave radiation via the urethra to a site inside the prostate. The interior of the prostate is then heated using microwave radiation. The temperature inside the prostate rises to the point that some of the tissue is killed. As this region of the prostate recovers, it decreases, minimizing urine flow obstruction.
- This procedure is completed in a single session. It normally does not necessitate an overnight hospital stay.
- It lowers the risk of retrograde ejaculations and the risk of bleeding.
- Risks of surgery include UTIs, dysuria, urgency, and the need for retreatment.
- Contraindications of TUMT are a penile implant, urethral stricture, metal implants in the pelvic area, a pacemaker, etc.
References
- Franco, J. V. A., Garegnani, L., Liquitay, C. M. E., Borofsky, M., & Dahm, P. (2022, Jan). Transurethral Microwave Thermotherapy for Benign Prostatic Hyperplasia: An Updated Cochrane Review. The World Journal of Men’s Health, 40(1), 127-138. doi: 10.5534/wjmh.210115
- Blute, M. L., Tomera, K. M., Hellerstein, D. K., Atkinson, E. J., Patterson, D. E., & Segura, J. W. (1992, May 1). Transurethral microwave thermotherapy for prostatism: early Mayo Foundation experience. Mayo Clinic Proceedings, 67(5), 417-421. Elsevier. https://doi.org/10.1016/S0025-6196(12)60386-3
- Devonec, M., Tomera, K., & Perrin, P. (1993). Review: Transurethral microwave thermotherapy in benign prostatic hyperplasia. Journal of endourology, 7(3), 255-259. https://doi.org/10.1089/end.1993.7.255
- Hoffman, R. M., Monga, M., MacDonald, R., & Wilt, T. J. (2003, Jan). Microwave thermotherapy for benign prostatic obstruction. Cochrane Database of Systematic Reviews, (1). https://doi.org/10.1002/14651858.CD004135
- Rubenstein, J. (2021, Jan 15). Transurethral Microwave Thermotherapy of the Prostate (TUMT). Medscape. Retrieved 2023, Jan 3 from https://emedicine.medscape.com/article/1950546-overview
- McNicholas, T., & Kirby, R. (2011, Aug 26). Benign prostatic hyperplasia and male lower urinary tract symptoms (LUTS). BMJ Clinical Evidence, 2011, 1801. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3217770/
- Mulvin, D., Creagh, T., Kelly, D., Smith, J., Quinlan, D., & Fitzpatrick, J. (1994). Transurethral microwave thermotherapy versus transurethral catheter therapy for benign prostatic hyperplasia. European urology, 26(1), 6-9. doi: 10.1159/000475334
- Ogden, C. W., Reddy, P., Johnson, H., Ramsay, J. W. A., & Carter, C. (1993, Jan 2). Sham versus transurethral microwave thermotherapy in patients with symptoms of benign prostatic bladder outflow obstruction. The Lancet, 341(8836), 14-17. https://doi.org/10.1016/0140-6736(93)92482-9
- Rubenstein, J. N., & McVary, K. T. (2004). Transurethral Microwave Thermotherapy. Management of Benign Prostatic Hypertrophy,109-124. Humana Press, Totowa, NJ. https://link.springer.com/chapter/10.1007/978-1-59259-644-7_8