Definition of stroke
In 1970, World Health Organization (WHO) defined stroke as “rapidly developing clinical signs of focal (or global) disturbance of cerebral function, lasting more than 24 hours or leading to death, with no apparent cause other than that of vascular origin”.
Definition of stroke according to American heart association 2013
- CNS infarction is the brain, spinal cord, or retinal cell death due to ischemia, based on
- Pathological, imaging, or other objective evidence of cerebral, spinal, or retinal focal ischemic injury in a defined vascular distribution; or
- Clinical evidence of cerebral, spinal, or retinal focal ischemic injury based on symptoms persisting at least 24 hours or until death and other etiologies excluded.
- Silent CNS infarction is imaging or neuropathologic evidence of CNS infarction without a history of acute neurological dysfunction attributable to the lesion.
- Ischemic stroke is an episode of neurological dysfunction caused by focal cerebral, spinal, or retinal infractions.
- Stroke due to Intracerebral Hemorrhage is rapidly developing clinical signs of neurologic dysfunction due to a focal collection of blood within the brain parenchyma or ventricular system, which is not due to trauma.
- Silent cerebral Hemorrhage is a focal collection of chronic blood products within the brain parenchyma, subarachnoid space, or ventricular system on neuroimaging or neuropathological examination which is not due to trauma, without a history of acute neurological dysfunction attributable to the lesion.
- Stroke due to subarachnoid hemorrhage is rapidly developing signs of neurological dysfunction and/or headache due to bleeding into the subarachnoid space, not due to trauma.
Pathophysiology
- The blood flow to the brain is managed by two internal carotids anteriorly and two vertebral arteries posteriorly, also known as the circle of Willis.
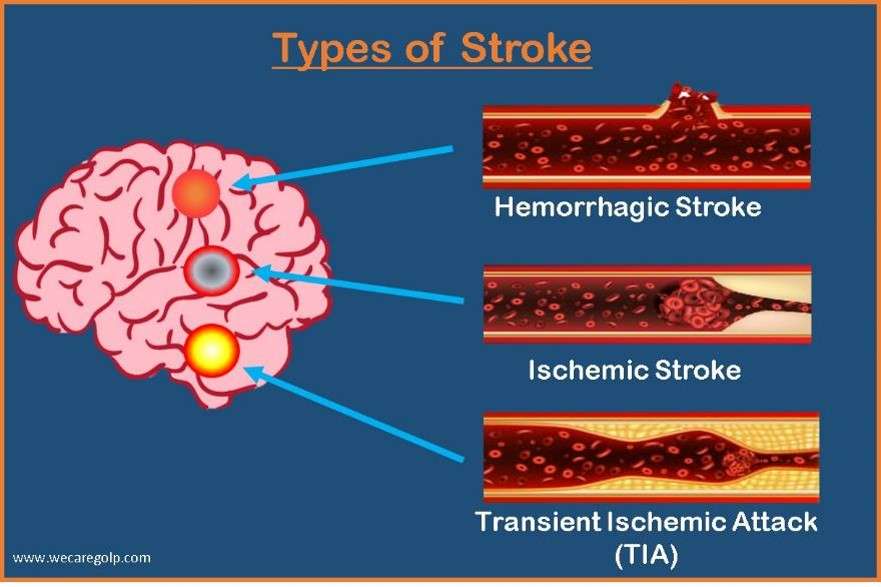
- The cause of ischemic stroke is a deficiency of blood and oxygen supply to the brain, whereas hemorrhagic stroke is because by bleeding or leaky blood vessels.
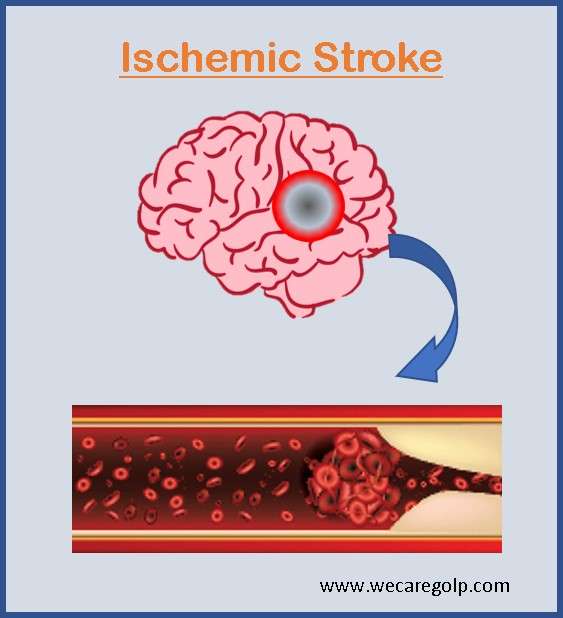
Ischemic stroke
- Blood occlusion generates thrombotic and embolic conditions in the brain.
- The blood flow is affected in thrombosis by the narrowing of vessels due to atherosclerosis.
- Plaque builds up which eventually constrict the vascular chamber and form clots, causing a thrombotic stroke.
- Decreased blood flow to the brain region causes an embolism leading to an embolic stroke causing severe stress and untimely cell death (necrosis).
- Disruption of the plasma membrane, organelle swelling and leaking of cellular contents into extracellular space, and loss of neuronal function are followed by necrosis.
- Other key events leading to stroke pathology are inflammation, loss of homeostasis, acidosis, excitotoxicity, energy failure, increased intracellular calcium levels, free radical-mediated toxicity, cytokine-mediated cytotoxicity, complement activation, impairment of the blood-brain barrier, activation of glial cells, oxidative stress and infiltration of leukocytes.
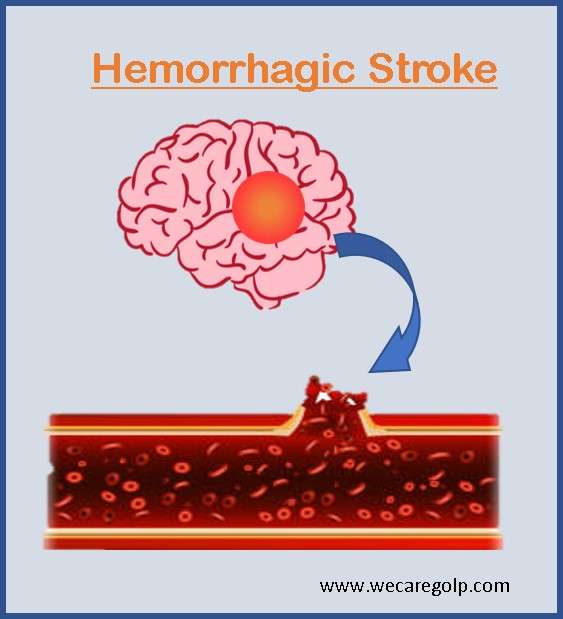
Hemorrhagic stroke
- Blood vessels in the brain rupture due to stress in the brain tissue and internal injury.
- It produces toxic effects in the vascular system, causing infarction.
- In ICH (intracerebral hemorrhage), blood vessels lead to the accumulation of blood within the brain.
- Blood accumulates in the subarachnoid space of the brain due to a head injury or cerebral aneurysm in SAH (subarachnoid hemorrhage).
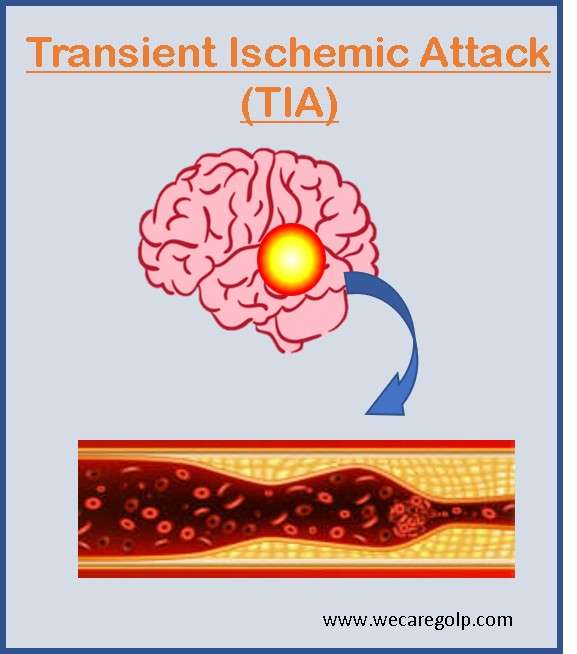
Transient ischemic attack (TIA)
- A TIA is a warning sign of a stroke.
- It often refers to as a mini-stroke, where the blood flow of the brain is blocked for a couple of minutes and does not cause lasting damage.
- You cannot distinguish from the symptoms whether it is a TIA or stroke.
- It is also a medical emergency.
- Therefore, the treatment must start as soon as possible.
Incidence
- According to American Heart Association: Globally, stroke remained the second-leading cause of death (11·6% of total deaths) and the third-leading cause of death and disability combined (5·7% of total Disability-adjusted Life Years (DALYs)) in 2019.
- From 1990 to 2019, the absolute number of incident strokes increased by 70%, the prevalence of strokes increased by 85%, deaths from stroke increased by 43%, and DALYs due to stroke increased by 32%.
Risk factors
Modifiable
- High blood pressure or cholesterol
- Smoking
- Diabetes
- Heart disease
- History of mini-strokes (transient ischemic attacks)
- Obesity
- Excessive alcohol or drug use
Non-modifiable
- Genetics: Family history of strokes
- Race: African Americans have a higher risk of stroke than other races.
- Age: Chance of having a stroke more than doubles for each decade of life after 55.
- Gender: Men have strokes more often, but women are more likely to die from a stroke.
Signs and symptoms
The signs and symptoms vary from person to person but usually begin suddenly. Depending on the part of the brain affected and the extent of the damage, the symptoms will vary.
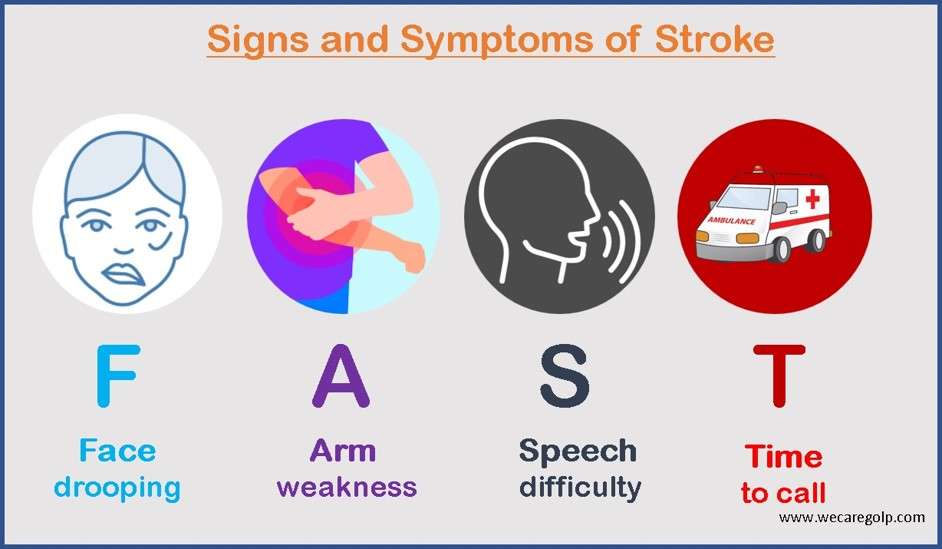
The symptoms of stroke can remember with the word FAST.
- Face – The face may have dropped on one side, the person may not be able to smile, or the mouth or eye may have drooped.
- Arms – The person may not be able to lift both arms and keep them there because of weakness or numbness in one arm.
- Speech – Their speech may be slurred or garbled, or the person may not be able to talk at all despite appearing to be awake; they may also have problems understanding what you are saying to them.
- Time – It is time to seek medical help immediately if we notice any of these signs or symptoms.
Other signs and symptoms
- Difficulty understanding what others are saying
- Sudden loss or blurring of vision
- Difficulty swallowing (dysphagia)
- Complete paralysis of one side of the body
- Being or feeling sick, dizziness, confusion
- Problems with balance and coordination
- A severe and sudden headache resulting in a blinding pain unlike anything experienced before the loss of consciousness, etc.
Diagnostic evaluation
Blood tests
- To determine blood sugar levels, evidence of infection, platelet counts, clotting factors, cholesterol levels, etc.
Magnetic Resonance Imaging (MRI) and Computerized Tomographic (CT) scan
- MRI can help see the damaged brain tissue or cells.
- CT scan can provide a detailed and clear picture of the brain that can show any bleeding or damage and other brain conditions that could be causing the symptoms.
Electrocardiogram (ECG)
- Electrocardiogram (ECG) records the electrical activity in the heart, measuring its rhythm and rate that determine the presence of any heart conditions that may have led to a stroke, such as a prior heart attack or atrial fibrillation.
- It helps to find sources of clots in the heart that may have traveled to the brain and caused a stroke.
Cerebral angiogram
- A cerebral angiogram gives a detailed picture of the arteries in the neck and brain which can show blockages or clots that may have caused symptoms.
Carotid ultrasound
- Carotid ultrasound can show fatty deposits (plaque, blockage, or narrowing in carotid arteries, which supply blood to the face, neck, and brain.
Preventive Guideline
Many risk factors are modifiable. Thus, lifestyle modification is essential to reduce the primary and secondary attacks of stroke. Lifestyle modification or a healthy lifestyle can lead to improvements in blood pressure, cholesterol level, obesity, and glucose metabolism which eventually decreases the risk for stroke. Some of the measures for a healthy lifestyle are as follows.
Physical exercise
- Maintain body mass index (BMI) below 25 kg/m2.
- Progressively increase physical activity such as brisk walking at least 30 minutes per day, on five days of the week.
- Perform Aerobic activity 20 to 60-minute sessions, 3-5 days per week. Multiple short sessions (e.g., 10 minutes) are encouraged to build tolerance and endurance.
- Strength training: perform 1 to 3 sets of 10-15 repetitions targeting large muscle groups, 2-3 days a week.
- Non-exercise physical activity: Reduce sedentary time by standing, frequent walking, using stairs, and reducing time for watching TV and mobile more often.
Healthy diet
- Restrict salt to less than 5 grams (1 teaspoon) per day.
- Limit processed and fast foods.
- Limit fatty meat, dairy fat, and cooking oil to less than two tablespoons per day. Replace palm and coconut oil with olive, soya, corn, rapeseed, or sunflower oil.
- Replace other meat with chicken (without skin)
- Consume fruits and vegetables
- 5 servings (400–500 g) of fruits and vegetables per day
- 1 serving is equivalent to 1 orange, apple, mango, banana or 3 tablespoons of cooked vegetables.
- Eat fish at least 3 times per week.
Stop tobacco and alcohol
Stress management
- Deep breathing exercises, Yoga, meditation, stretching and relaxation exercises, a healthy balanced diet, etc. are helpful in stress reduction.
Treatment and Management
According to the American Heart Association and American Stroke Association, “Time lost is brain lost.” Stroke treatment depends on the type of stroke.
Ischemic stroke and TIA
Since a blood clot or blockage in the brain causes these stroke types, they treat largely with similar techniques that may include.
- Thrombolytic drug: Tissue plasminogen activator (tPA), or Alteplase IV r-tPA, is considered as the gold standard which dissolves the clot and will stop the stroke. It reduces damage to the brain. Patients are also less likely to have any lasting disability because of the stroke.
- Mechanical thrombectomy: This surgery is most successful if it is performed 6 to 24 hours after the stroke begins.
- Stent: A stent inflates the narrowed/ weakened artery and supports the wall of arteries.
- Surgery: In the rare instances that other treatments do not work, surgery can remove a blood clot and plaque from the arteries.
Hemorrhagic stroke
- Medications: The treatment goal is to enhance the blood clot. The drugs reduce blood pressure, lower the pressure in the brain, prevent seizures and constrict blood vessels.
- Coiling: During this procedure, a long coil-like device installs in the area of the hemorrhage, or weakened blood vessels that block blood flow to the bleeding area and reduce bleeding.
- Clamping: A tiny clamp is placed at the base of the aneurysm to prevent additional bleeding. It cuts off the blood supply and prevents a possible broken blood vessel or new bleeding.
- Surgery: Craniotomy may be needed to relieve the pressure on the brain after a large stroke.
Stroke medications
Several medications use to treat strokes that depend largely on the type of stroke the patient had. Among them, some medications prevent a stroke for the first time, and some uses to prevent a second stroke episode. Direct-acting oral anticoagulants: Tissue plasminogen activator (tPA) must be given within 3 to 4.5 hours after symptoms of a stroke begin.
- Anticoagulants: The most common anticoagulant is warfarin.
- Antiplatelet drugs: The most common antiplatelet drugs include aspirin and clopidogrel. This drugs can prevent secondary ischemic strokes.
- Statins: Statins help lower high blood cholesterol levels. Common statins include rosuvastatin, simvastatin, and atorvastatin.
- Antihypertensive drugs.
Complications
- Cerebral edema: After a stroke, cerebral edema occurs as the body’s natural response to injury. It restricts the blood supply to the brain, resulting in the death of brain tissue.
- Seizures: Brain injury after stroke results in scar tissue. The scar tissue interrupts the electrical activity in the brain which can cause a seizure.
- Pneumonia and other chest infections: Trouble swallowing can cause aspiration, or food or liquids being ingested into the airway, which can lead to chest infection or pneumonia. This is one of the major causes of morbidity and mortality after stroke.
- Bladder problems: Increased frequency of micturition, functional incontinence, reflex incontinence, and urine retention may result after stroke.
- Shoulder pain: Shoulder pain occurs in around 80% of stroke patients who have little or no voluntary movement of the affected limb. Spasticity, tendonitis, Subluxation, partial dislocation of the shoulder, and rotator cuff tears are all possible causes of shoulder pain.
- Falls and Accidents: stroke results in common impairments like imbalance, sensory impairment, weakness, visual problems, and lack of coordination will naturally increase the risk of falls and accidents
- Other complications of immobility: Due to impaired mobility after stroke, many complications like Deep vein thrombosis, pressure sore, contractures, Urinary tract infections, etc. may be seen in patients.
- Social isolation and Clinical depression: Change of role in the family and society may result in social isolation. As stroke is a major health crisis leading to depression resulting in difficulty concentrating, sadness, irritability, hopelessness, changes in appetite and sleep patterns, apathy, and sometimes even suicidal thoughts.
Rehabilitation
Approximately two-thirds of stroke survivors require rehabilitation. The goals of rehabilitation are to optimize the functions of the patient after a stroke and the level of independence to achieve the best possible quality of life.
Stroke recovery typically focuses on four main areas:
Speech Therapy
- Stroke survivors may experience aphasia, word-finding difficulty, dyslexia, dysgraphia, dysarthria, dyspraxia, etc. Speech and language therapy helps patients to manage the communication and swallowing difficulty they may face after a stroke.
Cognitive Therapy
- Following a stroke, many people may have changes in their thinking and reasoning skills.
- It can cause behavioral and mood changes.
- An occupational therapist can help patients to regain their former patterns of thinking and behavior and manage their emotional responses.
Relearning Sensory Skills
- If the part of the brain that relays sensory signals is affected during the stroke, the patient may find that the senses are “dulled” or no longer working such as temperature, pressure, or pain.
- An occupational therapist can help the patient to adjust to this lack of sensation.
Physical Therapy
- Muscle tone and strength may weaken by a stroke, and the patient may be unable to move the body as well as they could use before.
- A physical therapist will work with them to regain their strength and balance and find ways to adjust to their limitations.
Rehabilitation may take place in a clinic, skilled nursing home, or in patient’s own home.
Summary
- A stroke is a serious life-threatening medical condition that happens when the blood supply to part of the brain cuts off. There are two major causes of strokes: ischemic and hemorrhagic.
- There is also a related condition called a transient ischemic attack (TIA), where the blood supply to the brain is temporarily interrupted.
- The main symptom of stroke can remember the word FAST (Face, Arm, Speech, and Time to act).
- Stoke can diagnose with a blood test, CT MRI, Carotid ultrasound, cerebral angiogram, etc. some of the complications are cerebral edema, seizures, immobility-related complications, etc.
- A healthy lifestyle is crucial in preventing and managing stroke. Medical and surgical management is done in the treatment phase.
- Rehabilitation is very important to maintain the quality of life of a patient.
References
- Fonseca AC, Merwick Á, Dennis M, et al. European Stroke Organisation (ESO) guidelines on management of transient ischaemic attack. European Stroke Journal. 2021;6(2): CLXIII-CLXXXVI. doi:10.1177/2396987321992905
- Quinn, T. J., Richard, E., Teuschl, Y., Gattringer, T., Hafdi, M., O’Brien, J. T., … & Markus, H. S. (2021). European Stroke Organisation and European Academy of Neurology joint guidelines on post-stroke cognitive impairment. European stroke journal, 6(3), I-XXXVIII.
- Virani, S. S., Alonso, A., Aparicio, H. J., Benjamin, E. J., Bittencourt, M. S., Callaway, C. W., … & American Heart Association Council on Epidemiology and Prevention Statistics Committee and Stroke Statistics Subcommittee. (2021). Heart disease and stroke statistics—2021 update: a report from the American Heart Association. Circulation, 143(8), e254-e743.
- GBD 2019 Stroke Collaborators (2021). Global, regional, and national burden of stroke and its risk factors, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. The Lancet. Neurology, 20(10), 795–820. https://doi.org/10.1016/S1474-4422(21)00252-0
- Cho, J. H., Rhee, E. J., Park, S. E., Kwon, H., Jung, J. H., Han, K. D., Park, Y. G., Yoo, S. J., Kim, Y. H., Lee, W. Y., & Taskforce Team of the Obesity Fact Sheet of the Korean Society for the Study of Obesity (2019). Maintenance of body weight is an important determinant for the risk of ischemic stroke: A nationwide population-based cohort study. PloS one, 14(1), e0210153. https://doi.org/10.1371/journal.pone.0210153
- https://www.nhs.uk/conditions/stroke/symptoms
- WHO package of essential noncommunicable (PEN) disease interventions for primary health care 2020