Introduction
Rheumatoid arthritis, or RA, is an autoimmune, systemic, and inflammatory disease that primarily affects the joints, causing inflammation, pain, and stiffness. While the exact cause of RA remains mysterious, it is believed to be caused by a combination of environmental and genetic factors.
RA results in the destruction of connective tissue and synovial membrane of the joints. As RA is a systemic disease, it can affect various organs and systems in the body beyond the joints, such as skin, eyes, heart, lungs, and blood vessels.
Exacerbation usually occurs during periods of physical or emotional stress and fatigue. A common characteristic of RA is morning stiffness, lasting for more than an hour. It mostly affects the joint of the hand and feet and other joints of the elbows, shoulders, neck, jaw, ankle, knee, and hip.
Incidence
- RA affects twice the number of women than men. Around 1.5% of the world’s population suffers from RA.
- Based on the self-reported data from NHS 2014-2015 at a population level, the highest incidence of RA is reported in Australia (2%) worldwide.
- Rheumatoid arthritis affects approximately 14 million people worldwide (World Health Organization, 2021).
- More than 1.36 million adults in the U.S. are affected by RA (Rheumatology International, 2017).
Types of Rheumatoid Arthritis
There are mainly two types of RA, seropositive and seronegative RA, which can be distinguished based on the presence or absence of auto-antibody called rheumatoid factor (RF).
Seropositive (Rheumatoid factor positive) RA
More than 80% of the people suffering from RA test positive for RF, but it can be present in other medical conditions such as infection. In addition to RF, a physical manifestation of RA along with a positive test result for Anti-cyclic citrullinated protein peptides (anti-CCP) or anti-citrullinated protein antibodies (ACPAs) confirms the diagnosis of seropositive RA.
Seronegative (Rheumatoid factor negative) RA
Seronegative is reported as negative for antibodies (anti-CCP) or RF in the blood. There is no certainty that a negative for antibodies or RF may have a milder disease. The diagnosis is based on disease manifestations, x-rays, and other investigations.
Juvenile Idiopathic Arthritis (JIA)
JIA mainly affects children aged 16 or younger for a minimum of 6 weeks, causing joint stiffness and swelling in the children. In contrast to adult RA, JIA is acute and often resolves with growing age but can affect bone development in a child. There are different types of JIA. They are systemic onset, oligoarticular, polyarticular, psoriatic, undifferentiated RA, etc.
Stages of Rheumatoid Arthritis
There are mainly four stages of RA.
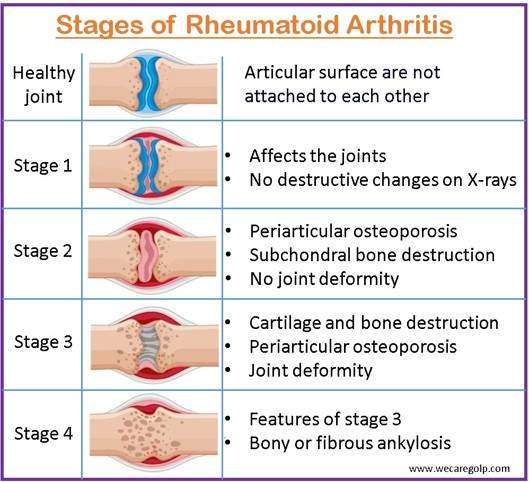
Stage I: Synovitis
In stage I, the immune system starts to affect the joint tissue, synovial membrane becomes hyperemic and edematous. In this stage, it affects the hands, fingers, knees, and ankles. Mild symptoms together with joint pain and stiffness start at this stage.
Steg II: Pannus
In stage II, the cartilage that cushions the bone and helps in joint motion starts to thin. Thinning of the cartilage worsens joint pain and stiffness, which erodes the joint and leads to joint damage.
Stage III: Fibrous ankylosis
Ankylosis refers to the fusion of the bone at a joint, causing immobility. During this phase of RA, the damaged joint begins to fuse with fibrous connective tissue, which makes the joint bent and crooked, limiting daily living activity.
Stage IV: Bony ankylosis
It is the last stage of RA, in which bone fuses with actual bone tissue rather than connective tissue. At this stage of RA, muscle strength will be decreased, and the joint is fused leading to loss of joint mobility. Progression of the RA to this stage may affect the ability to perform daily activities.
Causes of Rheumatoid Arthritis
The exact cause of rheumatoid arthritis remains unknown. In rheumatoid arthritis, the immune system is thought to be triggered by two substances in our bodies, notably the tumor necrosis factor (TNF) and interleukin-1. However, it is believed to result from a combination of genetic and environmental factors.
Risk Factors of Rheumatoid Arthritis
There are several modifiable and non-modifiable risk factors of RA.
- Age: The risk of RA increases with age and is at its maximum in the sixties.
- Sex: The risk of RA is 2-3 times higher in women than in men.
- Genetic traits: Genes called HLA (Human Leukocyte Antigen) class II genotype increases the risk of RA in combination with exposure to environmental factors like smoking or obesity.
- Smoking: Cigarette smoking increases the risk of RA and worsens the disease.
- History of live births: Nulliparous women are at higher risk of RA.
- Early life exposures: Early life exposure to smoking may increase the risk of RA. Also, poverty in childhood may increase the risk of RA as adults.
- Obesity: The risk of RA increases with obesity.
- Stress: Stress increases the risk of RA and worsens the disease.
- Infection: Infections such as UTI with Proteus mirabilis bacteria, Epstein-Barr virus, Mycoplasma genus, and gum diseases increase the risk of RA. Prevotella Copri, a gut bacterium, may also trigger RA and causes inflammation.
- Diet: Diets containing anti-inflammatory and antioxidant properties may help manage RA; however, diets containing animal products or higher amounts of salts or oil trigger or worsen RA.
Sign and Symptoms of Rheumatoid Arthritis
- Inflammation, tenderness, and stiffness of the affected joints
- Moderate to severe pain with morning stiffness for more than 30 minutes
- Joint immobility, muscle atrophy, decrease in range of motion of the joint
- Soft, spongy joints
- Low-grade fever, fatigue
- Anorexia, weight loss, anemia
- Increase ESR (Erythrocyte sedimentation rate) and Positive Rheumatoid factor
- Joint deterioration in radiographic studies
- Inflammation of synovial tissue in biopsy
Pathophysiology of Rheumatoid Arthritis
The pathophysiology of RA involves a complex interaction of three different domains:
- A complex genetic predisposition to the disease and some environmental stimulus;
- A self-perpetuating, self-amplifying, intra-synovial immune response; and
- Tissue injury mediated by pro-inflammatory cells, inflammatory effector molecules, and degradative enzymes.
In RA, a process tending to affect joints, called arthrotropic, produces a characteristic pathologic lesion in the synovium as well as the hallmark erosions of bone and destruction of cartilage at the joint margin. It involves the synovial lining, the interstitium, and the microvasculature. Synovial inflammation begins with the infiltration of immune cells, especially B cells, T cells, and macrophages. Tumor necrosis factor-alpha (TNF-alpha), interleukin-1 (IL-1), and interleukin-6 (IL-6) are examples of pro-inflammatory cytokines released by these cells that contribute to the breakdown of joint tissues and chronic inflammation.
Pannus develops when the inflamed synovium undergoes hyperplasia (an abnormal increase in cell proliferation). Pannus is an invasive, destructive tissue that erodes cartilage, bone, and other joint structures.
Number and mass of the synovial lining increase. A diffuse and nodular inflammatory cell infiltrate is observed in the interstitium. It includes CD4+ and CD8+ lymphocytes, dendritic cells, and other antigen-presenting cells. The synovium of the affected joint resembles a benign tumor. Endothelial cell activation is initially revealed by the microvasculature. Plasma cells and multi-nucleated giant cells appear, and the vascular supply becomes exuberant as the process matures.
Eventually, when the developing synovium reaches the hyaline cartilage near the joint’s edge, it appears as granulation tissue. The characteristic erosion at the bone and cartilage margin is caused locally by degradative enzymes and activated osteoclasts. These enzymes may also have an impact on distant structures like tendons, ligaments, and other musculoskeletal ones. Erosions are produced by bone and matrix protein that resorbs osteoclasts, induced and activated by cytokines released into the inflammatory milieu.
Rheumatoid arthritis is not restricted to joint inflammation. It can cause systemic symptoms affecting other organs and body systems like cardiovascular complications, pulmonary involvement, systemic inflammation, and an increased risk of osteoporosis.
Diagnosis of Rheumatoid Arthritis
- History taking: If you have first-degree relatives who have tested positive for RF, your risk of developing RA is more than four times higher.
- Physical examination: Joint problems like pain, stiffness, inflammation, and tenderness
- Antibody test: Even before any clinical signs appear, over five to ten years, antibodies may be detected in blood testing.
- Rheumatoid factor (RF):
- Anti-cyclic citrullinated peptide (anti-CCP) antibody: Positive test helps to rule out RA.
- Anti-citrullinated protein antibodies (ACPAs)
- Other lab tests
- Erythrocyte sedimentation rate and C-reactive protein: An increase in levels of these tests suggest inflammation in the body.
- Complete blood counts
- Imaging studies: X-ray and MRI scans of the affected joint
- American College of Rheumatology (ACR)/ European League Against Rheumatism (EULAR) criteria: These criteria are used to diagnose RA by considering the number and location of affected joints, blood test results, and duration of symptoms.
Treatment of Rheumatoid Arthritis
Although RA is not a curable disease, supportive treatment can help prevent early mortality. The goals of RA treatment are to
- Reduce inflammation,
- Prevent joint damage, and
- Reduce long-term complications.
Medical management
- Non-steroidal anti-inflammatory drugs (NSAIDS): NSAIDS can reduce inflammation and pain.
- Ibuprofen
- Naproxen
- Steroids: Corticosteroids can reduce inflammation, pain, and joint damage.
- Prednisolone
- Methylprednisolone
- Conventional disease-modifying antirheumatic drugs (DMARDs): DMARDs can lower the progression of RA and prevent permanent joint and tissue damage.
- Methotrexate
- Leflunomide
- Hydroxychloroquine
- Sulfasalazine
- Biological agents: The newer class of DMARDs, also called biological response modifiers, include
- Abatacept
- Adalimumab
- Anakinra
- Certolizumab
- Etanercept
- Golimumab
- Infliximab
- Sarilumab
- Targeted synthetic DMARDs: If conventional and biological agents are ineffective, targeted synthetic DMARDs are used to manage RA.
- Baricitinib
- Tofacitinib
- Upadacitinib
Surgical Management
- Synovectomy: Removing the inflamed synovium helps to reduce pain and improve joint flexibility.
- Joint fusion: Joint is fused surgically to stabilize or realign a joint and helps to reduce the joint pain.
- Total joint replacement: During the procedure, damaged parts of the joint are removed and metal or plastic prostheses are placed.
- Tendon repair surgery: It is a surgery to repair torn or damaged tendons.
Physical or Occupational therapy
- Exercise helps to keep the joint flexible and helps in the Activity of daily living.
- Assistive devices can help to prevent stress on affected joints.
Prevention of Rheumatoid Arthritis
There is no assurance that RA can be prevented. However, modifying lifestyles and certain behaviors can help reduce RA and its complications.
- Cessation of smoking and alcohol
- Maintaining a healthy weight
- Diet rich in omega-3, vit. D, vegetables, fruit, olive oil, nuts, and vegetables
- Regular exercise 20-30 minutes a day
- Avoid high salt and sugar in the diet
- Maintaining good oral hygiene, treating any gum or tooth disease
Complications of Rheumatoid Arthritis
Rheumatoid arthritis (RA) can lead to complications within the joints and other body parts. Here are some common complications associated with RA:
- Chronic joint inflammation: RA may lead to joint destruction, erosion of bone and cartilage, and loss of function which may lead to impaired mobility.
- Rheumatoid Nodules: Rheumatoid nodules are firm, non-tender lumps found in about 20-30% of individuals with RA and can occur in the lungs as well. While they are typically benign, they can sometimes cause pain or become infected.
- Cardiovascular Complications: People with RA have an increased risk of developing cardiovascular diseases such as heart attacks, strokes, pericarditis, and peripheral vascular disease.
- Lung Involvement: Rheumatoid arthritis can cause inflammation and scarring of the lungs. Breathing difficulties and reduced lung function may result from conditions like pleurisy (inflammation of the lining around the lungs), pulmonary fibrosis (scarring of lung tissue), and rheumatoid lung nodules.
- Eye Problems: RA-related inflammation can affect the eyes, leading to scleritis (inflammation of the white part of the eye), uveitis (inflammation of the middle layer of the eye), Sjogren’s syndrome, and corneal damage. Regular eye exams are recommended for individuals with RA to monitor and manage any eye-related complications.
- Felty’s Syndrome: The rare complication of RA is characterized by the presence of an enlarged spleen and a low white blood cell count (neutropenia), leading to recurrent infections and anemia.
- Cervical myelopathy: It is a rare condition that affects mobility and can lead to permanent spinal cord damage if left untreated.
- Osteoporosis: Chronic inflammation and the use of corticosteroids for RA treatment can lead to the development of osteoporosis which increases the risk of fractures.
- Carpal tunnel syndrome: It is common in people with rheumatoid arthritis. It can cause aching, numbness, and tingling in the thumb, fingers, and part of the hand as a result of compressions of the median nerve.
- Risk for infection: People with RA may have a higher susceptibility to infections due to the disease itself and the immunosuppressive effects of certain medications used to manage RA. It is important to maintain a balance between managing inflammation and reducing infection risks.
- Depression and Anxiety: Chronic pain, disability, and the impact of RA on daily life can lead to mental health challenges such as depression and anxiety. Proper emotional support, counseling, and, if necessary, treatment can help address these issues.
Prognosis
The prognosis of rheumatoid arthritis can vary widely from person to person, and it depends on several factors. RA leads to damage affected joints in around 80-85% of people within two years of the disease. If left untreated, mortality is twice that of people without RA.
Prognosis may be widely affected by the following factors.
- Disease progression: RA is a progressive disease, which worsens over time, and the rate of progression can differ among individuals. Some people may experience mild symptoms and slow disease progression, while others may have more severe symptoms and rapid progression.
- Early diagnosis and treatment: Early diagnosis and appropriate treatment can significantly improve the long-term prognosis of RA. Prompt intervention with DMARDs and other medications can help control inflammation, reduce joint damage, and improve overall outcomes.
- Disease activity: The level of disease activity plays a crucial role in determining the prognosis. People with low disease activity or remission have a better prognosis compared to those with high disease activity. Regular monitoring, treatment adjustments, and adherence to medication regimens are essential in managing disease activity.
- Joint damage: Joint damage is a major concern in RA and can lead to functional impairment and disability. However, early and effective treatment can help slow down or prevent joint damage. Joint protection measures, physical therapy, and assistive devices can also contribute to preserving joint function.
- Extra-articular manifestations: Rheumatoid arthritis can affect various organs and systems outside the joints, leading to complications such as cardiovascular problems, lung disease, and systemic inflammation. The presence and severity of these extra-articular manifestations can influence the prognosis.
- Lifestyle factors: Lifestyle factors, including regular exercise, maintaining a healthy weight, and avoiding smoking, can positively impact the prognosis. A balanced diet and stress management techniques may also help manage symptoms and improve overall well-being.
- Treatment advances: The prognosis of RA has significantly improved over the years with the development of more effective medications, such as biologic agents and targeted therapies. These advancements have provided better disease control and improved outcomes for many individuals with RA.
It is important to note that while rheumatoid arthritis is a chronic condition, with proper management and care, people with RA can maintain a good quality of life. Working closely with healthcare professionals, following treatment plans, and adopting a proactive approach to managing the disease can make a significant difference in the prognosis.
Summary
- Rheumatoid arthritis (RA) is a systemic inflammatory disease primarily affecting the joints, causing pain, inflammation, and stiffness.
- It is one of the most common types of arthritis, with a higher incidence in women.
- RA can also affect organs and systems beyond the joints, leading to complications.
- Diagnosis is based on clinical symptoms, physical examination, and laboratory tests.
- Early detection and treatment play a crucial role in managing the disease and preventing joint damage.
- Treatment options include medications, physical therapy, and surgery.
- The prognosis varies but can be improved with timely intervention, disease management, and lifestyle modifications. RA requires ongoing care and support to maintain a good quality of life.
Other Autoimmune Disorders
- Multiple Sclerosis (MS)
- Guillain-Barré syndrome (GBS)
- Goodpasture Syndrome (GS)
- Myasthenia Gravis (MG)
- Vasculitis
- Type 1 Diabetes
- Systemic Lupus Erythematosus (SLE)
- Inflammatory Bowel Disease (IBD)
- Hashimoto’s Thyroiditis
References
- Almutairi, K., Nossent, J., Preen, D., Keen, H., & Inderjeeth, C. (2021). The global prevalence of rheumatoid arthritis: A meta-analysis based on a systematic review. Rheumatology International, 41, 863–877. https://doi.org/10.1007/s00296-020-04731-0
- Aletaha, D., & Smolen, J. S. (2018). Diagnosis and Management of Rheumatoid Arthritis: A Review. JAMA, 320(13), 1360-1372. doi:10.1001/jama.2018.13103
- Chauhan, K., Jandu, J.S., Lawrence H. Brent, L.H., Al-Dhahir, M.A. (2023) Rheumatoid Arthritis. .StatPearls Publishing. Retrieved on 2023, May 25 from https://www.ncbi.nlm.nih.gov/books/NBK441999/
- Silvestri, A.L., & Silvestri, E.A. (2020). Saunders comprehensive review for the NCLEX-RN examination: Rheumatoid arthritis (3rd ed.). ELSEVIER.
- National Institute of Arthritis and Musculoskeletal and Skin Diseases. (2022). Rheumatoid arthritis. Retrieved on 2023, May 25 from https://www.niams.nih.gov/health-topics/rheumatoid-arthritis
- MedlinePlus. (2018, May 2). Rheumatoid Arthritis. Retrieved on 2023, may 25 from https://medlineplus.gov/rheumatoidarthritis.html
- Illinois Department of Public Health. (n.d.). Rheumatoid Arthritis. Retrieved on 2023, May 25 from https://idph.illinois.gov/public/hb/hbrheu_arth.htm
- Centers for Disease Control and Prevention. (2022, April 7). Rheumatoid Arthritis. Retrieved on 2023, may 26 from https://www.cdc.gov/arthritis/types/rheumatoid-arthritis.html
- Global Rheumatology Alliance. (2017). Burden of Rheumatoid Arthritis. Retrieved on 2023, may 26 from https://globalranetwork.org/project/disease.
- Illinois Bone & Joint Institute. (2016, Feb 11). Types of Rheumatoid Arthritis: Seropositive or Seronegative RA. Retrieved on 2023, May 26 fromhttps://www.ibji.com/blog/rheumatology-autoimmune-care/types-of-rheumatoid-arthritis-seropositive-or-seronegative-ra/
- Arthritis Foundation. (2022). Juvenile Arthritis. Retrieved on 2023, May 25 from https://www.arthritis.org/juvenile-arthritis
- Johns Hopkins Medicine. (2023). Juvenile Idiopathic Arthritis. Retrieved on 2023, May 26 from https://www.hopkinsmedicine.org/health/conditions-and-diseases/arthritis/juvenile-idiopathic-arthritis
- Smith, L. (2021, Oct 12). Rheumatoid Arthritis Stages. GoodRx. Retrieved on 2023, may 25 from https://www.goodrx.com/conditions/rheumatoid-arthritis/rheumatoid-arthritis-stages
- Donvito, T. (2018, Nov 14). The 4 Stges of Rheumatoid Arthritis Stages Progression. CreakyJoints. Retrieved on 2023, May 25 from https://creakyjoints.org/about-arthritis/rheumatoid-arthritis/ra-overview/rheumatoid-arthritis-stages-progression/

