Introduction
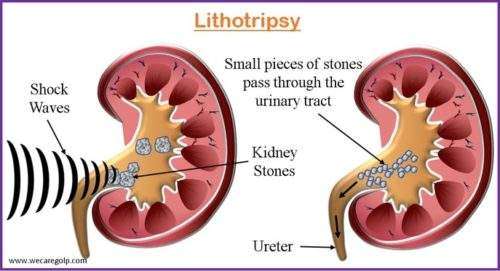
Lithotripsy is a medical procedure used to break up kidney stones and other stones in the urinary tract into smaller fragments so that they can be more easily passed out of the body.
- The term “lithotripsy” comes from the Greek words “lithos” (stone) and “tripsis” (friction or rubbing).
- The procedure is usually done using shock waves generated outside the body, which are focused on the stone using imaging techniques such as ultrasound or X-ray. Lithotripsy is considered a safe and effective treatment for many types of urinary tract stones.
- Lithotripsy is often used as a non-invasive alternative to surgery for the treatment of kidney stones and other urinary tract stones.
Types of Lithotripsy
Extracorporeal Shock Wave Lithotripsy (ESWL)
- It was introduced in the early 1980s and revolutionized the treatment of patients with kidneys, ureters (the conduit between the kidney and the bladder), pancreatic duct, and bile duct stones.
- ESWL is a non-invasive therapy that dissolves stones in the urinary system, pancreas, and bile ducts.
- It employs shock waves that are directed toward stones using X-rays or ultrasound.
- Stones in the kidneys and ureter frequently pass on their own following EWSL.
- Some stones, such as those in the pancreatic duct, may need the use of an endoscope (a hollow tube with a light and equipment that may capture and remove stones).
Intracorporeal Lithotripsy
- This form of lithotripsy involves lasers or other devices introduced into the body to break down stones or masses that are located inside the body.
- It is the process of seeing a calculus in the urinary system and simultaneously using energy to break it up into smaller, more manageable pieces.
- This can be accomplished using ureteroscopy, percutaneous nephrolithotomy (PCNL), or flexible ureterorenoscopy (FURS).
Electrohydraulic Lithotripsy (EHL)
- EHL is a procedure that employs focused shockwaves to break up pancreatic, gallstones, or renal stones.
- The shockwaves created by this type of extracorporeal lithotripsy are produced by a vaporization bubble expanding and contracting repeatedly, causing a pressure wave.
- Because the method is non-invasive and has a 90% success rate, it is recommended as first-line therapy for minor kidney stones.
- Electrical discharges are used to produce shock waves that break down the stones or masses.
Laser Lithotripsy
- Laser lithotripsy is a technique used to break up kidney stones in the urinary system.
- It is performed with a scope that may be inserted into the urinary tract tubes.
- No incisions are required. The laser fragments the kidney stones, allowing them to be removed by the surgeon or flow through the body in the urine.
- The laser energy is administered by a fiber optic cable introduced through a tiny incision in the body.
Ultrasound Lithotripsy
- Ultrasonic lithotripsy is a safe and effective method for controlled stone disintegration and quick evacuation of the resulting pieces under endoscopic supervision.
- It uses a mechanical vibration to shatter stones into smaller particles that may then be inhaled using specialized probes.
- This method requires direct contact between the probe and the stone.
Indications of Lithotripsy
Lithotripsy is utilized for the treatment of urinary tract stones, particularly stones in the kidney and the ureter. Patients with the following situations are candidates for lithotripsy.
- People who work in professions where unexpected symptoms of stone passage might lead to perilous circumstances (for example, pilots, military personnel, and physicians) (In such individuals, definitive management is preferred to prevent adverse outcomes.)
- People with solitary kidneys who have tried conservative therapy and spontaneous stone passage may develop anuria.
- Individuals who have hypertension, diabetes, or other medical disorders that put them at risk for renal insufficiency
- For effective treatment options for kidney, gallbladder, salivary, pancreatic, and urinary bladder stones, particularly those that are larger than 4 mm in size.
- Other therapies, such as surgery or medication, may not be appropriate for some people owing to their medical history, anatomy, or other considerations. Lithotripsy may be a better and safer choice for these individuals.
Contraindications of Lithotripsy
- Pregnancy: Lithotripsy is not suggested for pregnant women because the shock waves employed in the technique may affect the growing fetus.
- Blood Clotting Disorders: Individuals who have blood clotting abnormalities or are on blood-thinning medication may experience severe bleeding during or after the treatment.
- Infection: Lithotripsy is not advised if the patient has a current urinary tract infection (UTI) since it increases the chance of the infection spreading.
- Obesity: Individuals who are severely obese may not be candidates for lithotripsy because the apparatus may not be able to enter the body sufficiently to target the stone.
- Pacemaker or Implantable Defibrillator: Patients with pacemakers or implanted defibrillators may be ineligible for lithotripsy since the shock waves utilized in the operation can interfere with their devices.
- Abnormal Anatomy: Individuals with abnormal anatomy of the urinary system or other organs in the vicinity may be unsuitable for lithotripsy because the shock waves may not be able to target the stone efficiently.
- Large stones: Individuals with particularly large stones may be ineligible for lithotripsy because the therapy maynot efficiently break down the stone into tiny enough pieces for it to pass naturally.
Procedure of Lithotripsy
Patient Preparation
- Patients may be requested to submit information about their medical history, including past surgeries, allergies, drugs they are presently taking, and any underlying medical concerns.
- Blood and urine tests may be conducted to assess the patient’s kidney function as well as to detect any underlying infections or other medical disorders that might interfere with the treatment.
- Patients may be required to fast for a period before the surgery, often 4-6 hours, to ensure that their stomach is empty and to limit the risk of vomiting or aspiration during the treatment.
- Patients may need to change their prescriptions or discontinue specific drugs before the treatment, especially if they are using blood thinners or other medications that are contraindicated.
- Hydration: Patients may be urged to consume plenty of fluids before the treatment to achieve a high urine output, which can aid in the passage of tiny stone pieces during lithotripsy.
During Procedure
Extracorporeal shock wave lithotripsy
- Preparation: The patient is given a local anesthetic or sedative to help them relax. Participants lie down on a cushioned table or sofa, with their backs to the ESWL machine, which is a big, doughnut-shaped device that creates shock waves.
- Imaging: To find the kidney stone and establish its size and position, the healthcare professional employs imaging techniques such as X-rays, ultrasound, or a CT scan.
- Shock wave generation: The ESWL machine sends shock waves via the patient’s skin and body tissues to the kidney stone. They are high-energy sound waves that pass through the skin and soft tissues to reach the kidney stone.
- Shock wave delivery: Shock waves are administered to the kidney stone in a sequence of pulses or bursts that typically last 30-60 minutes. Once the shock waves impact the stone, the patient may experience a tapping or breaking feeling.
- Stone fragmentation: Shock waves generate pressure waves that travel through the kidney stone, breaking it up into smaller fragments. These tiny fragments can subsequently be excreted from the body via urine.
- Monitoring: Throughout the process, the patient’s vital signs and pain levels are checked to ensure that they are comfortable and safe. Further imaging may be required to determine the extent of stone fragmentation.
Intracorporeal shock wave lithotripsy
- Often, the patient is put under general anesthesia or local anesthetic with sedation. The skin over the kidney or ureter is disinfected and cleansed.
- An X-ray or ultrasound-guided ureteroscope is put into the urethra and directed up to the position of the stone.
- The lithotripter is introduced through the ureteroscope and placed near the stone.
- The lithotripter generates high-energy shockwaves that cause the stone to shatter into smaller shards.
- The shockwaves break up the stone into tiny bits, which can then be removed with a basket-like device or a suction tube.
Laser lithotripsy
- The laser is focused by inserting a laser fiber via the ureteroscope and positioning it near the stone.
- The laser energy is directed toward the stone to shatter it into smaller fragments.
- The laser is triggered, releasing high-energy pulses that shatter the stone into tiny fragments.
- To ensure that the stone is thoroughly broken up, the surgeon may utilize several laser settings and procedures.
Electrohydraulic lithotripsy
- An electrode is inserted through the ureteroscope and positioned close to the stone.
- The electrode delivers a high-voltage electric spark that creates a shock wave to break up the stone.
- The electric spark is activated, creating a shock wave that breaks up the stone into smaller pieces.
- The surgeon may use different electrode settings and techniques to ensure that the stone is completely broken up.
- Repeated procedure: Depending on the size of the stone, the lithotripter may need to be repositioned and the shockwaves delivered again to break up the stone further.
- Completion: The procedure is complete when all the stone fragments have been removed.
Ultrasound lithotripsy
- The conversion of electrical energy into ultrasonic energy is the basic principle of ultrasonic lithotripsy.
- The transducer receives the current from the generator and measures the excitation of the piezoelectric crystal.
- An acoustic wave with a frequency of 23–25 kHz is created while vibrating the crystal.
- Under operational frequencies, which vary depending on the aspirated liquid and the sonotrode’s pressure gradient on the stone, high metallic sounds of various tones can be heard.
Care after Procedure
- Following the procedure, the patient is closely followed for a short period of time to ensure that they are stable and that their vital signs are normal.
- It is suggested that the patient should rest for the first 24 hours after surgery since they may still be affected by the anesthetic.
- After 24 hours, the patient can resume all usual activities.
- Drinking lots of water may be suggested to help wash out any residual stone particles.
- With more rigorous activity, the patient may notice an increase in blood in the urine (hematuria). If this happens, the patient should minimize the exercise and increase water until the blood level drops. It is usual for blood to be seen in the urine for up to four weeks after the procedure. This is especially true if a ureteral stent has been inserted. After rest and water, blood in the urine should resolve.
- Do not restart any aspirin or anticoagulant drugs without first visiting a doctor.
Internal ureteral stents
- Internal ureteral stents are frequently implanted during intracorporal lithotripsy to aid healing and assure drainage, especially if aggressive therapeutic procedures were used.
- Internal stents may reduce the likelihood of urinomas (urinary collections outside the urinary collecting system) and/or ureteral strictures during traumatic endoscopy.
- Internal ureteral stents are usually associated with lower urinary tract symptoms such as frequency, urgency, and mild-to-moderate transitory hematuria.
- The ureteral stents are removed after a time of recovery that might range from a few days to 6-8 weeks, depending on the treatment’s intricacy.
- To alleviate symptoms associated with the ureteral stent, patients are released on oral antibiotics, analgesics, and, on occasion, anticholinergic medicine. When all tubes have been removed, antibiotics are generally administered to eradicate any bacteriuria.
- Follow-up consultations may be made to monitor the patient’s recovery and verify that no issues arise.
Complications of Lithotripsy
- Extravasation and pooling of blood
- Focal hemorrhage
- Urinary tract infections
- Necrosis in the vascular wall
- In certain circumstances, the stone shards may not have been entirely broken down and may require further treatment.
- All kinds of lithotripsy can result in incomplete and/or insufficient stone pulverization. The remaining pieces might cause renal or ureteral colic as well as subsequent treatments.
- Mucosal injuries
- Perforation
- Guidewire breakage, and stones dropping into the retroperitoneum.
Advantages of Lithotripsy
- Lithotripsy is a non-invasive technique that does not necessitate incisions or surgery. No general anesthetic is required, and the patient can generally return home the same day.
- Recovery time is lower than for other surgical procedures. It has a high success rate in breaking up kidney stones and allowing them to flow out of the body; patients may typically resume regular activities within a few days following the surgery.
- Lithotripsy is a generally painless therapy that causes only little discomfort during or after the process.
- If the first lithotripsy treatment fails, the surgery can be repeated without posing any substantial hazards to the patient.
- Lithotripsy is frequently less costly than other surgical techniques for kidney stone removal. This is because it is conducted as an outpatient procedure and does not necessitate an overnight hospital stay.
Summary
- Lithotripsy is a non-invasive or minimally invasive medical procedure that employs shock waves or a laser to dissolve stones in the kidney, gallbladder, or ureters or to break up kidney or ureteral stones into smaller pieces that can be passed out of the body more easily.
- There are several types of lithotripsies, including extracorporeal shockwave lithotripsy (ESWL), which uses high-energy shockwaves to break up stones, and laser lithotripsy, which uses a laser beam to break up stones. Another type of lithotripsy is electrohydraulic lithotripsy (EHL), which uses an electrically-generated shockwave to break up stones. The process typically lasts 30 minutes to 2 hours.
- The method of lithotripsy used is determined by the stone’s size, location, and composition, as well as the patient’s overall health and medical history.
- After lithotripsy, the patient may be administered pain medicine and antibiotics, as well as a specific diet or increased fluid intake to assist flush out any residual stone particles.
References
- Aboumarzouk, O. M., Kata, S. G., Keeley, F. X., & Nabi, G. (2011). Extracorporeal shock wave lithotripsy (ESWL) versus ureteroscopic management for ureteric calculi. Cochrane Database of Systematic Reviews, (12). https://doi.org/10.1002/14651858.CD006029.pub3
- Cleveland, R. O., & McAteer, J. A. (2012). Physics of shock‐wave lithotripsy. Smith’s textbook of endourology, 527-558. https://doi.org/10.1002/9781444345148.ch49
- Grasso, M. (2018). Intracorporeal lithotripsy. Medscape. Retrieved on 2023, March 28 from https://emedicine.medscape.com/article/445341-overview#a6
- Grasso, M. (2022). Extracorporeal shockwave lithotripsy. Medscape. Retrieved on 2023, March 28 from https://emedicine.medscape.com/article/444554-overview
- Kroczak, T., Scotland, K. B., Chew, B., & Pace, K. T. (2017). Shockwave lithotripsy: techniques for improving outcomes. World journal of urology, 35, 1341-1346. https://link.springer.com/article/10.1007/s00345-017-2056-y
- Leighton, T. G., & Cleveland, R. O. (2010). Lithotripsy. Proceedings of the Institution of Mechanical Engineers, Part H: Journal of Engineering in Medicine, 224(2), 317-342. https://doi.org/10.1243/09544119JEIM
- Reynolds, L. F., Kroczak, T., & Pace, K. T. (2018). Indications and contraindications for shock wave lithotripsy and how to improve outcomes. Asian journal of urology, 5(4), 256-263. https://doi.org/10.1016/j.ajur.2018.08.006
- Ventimiglia, E., Villa, L., Doizi, S., Briganti, A., Proietti, S., Giusti, G., … & Salonia, A. (2021). Laser lithotripsy: the importance of peak power and pulse modulation. European Urology Focus, 7(1), 22-25. https://doi.org/10.1016/j.euf.2021.01.012
- Zhong, P. (2013). Shock wave lithotripsy. Bubble dynamics and shock waves, 291-338. https://link.springer.com/chapter/10.1007/978-3-642-34297-4_10
