Introduction
Vitamin D is a fat-soluble vitamin. It helps the human body absorb and retain calcium and phosphorus essential for bone and teeth health.
- It is known as a ‘sunshine vitamin’ because the human body converts a precursor 7-dehydrocholesterol (a sterol in the skin) to vitamin D with sunlight.
- The body synthesizes adequate amounts through simple exposure to sunlight, even for five minutes per day. It is responsible for maintaining the calcium and phosphate balance in the body.
- It is a unique vitamin as many consider it both a nutrient and a prohormone, a substance that the body can transform into an active hormone.
- Although it is present in food, the body can synthesize it in significant amounts that utilize the compound to produce a hormone.
- Calcitriol is the active form of vitamin D formed in the kidney.
Types and Sources of Vitamin D
Sunlight is the main source of vitamin D (VD). However, The American Academy of Dermatology does not recommend getting it through unprotected sun exposure or tanning beds.
Foods are not a good source of vitamin D. Depending on the food source, it can classify into two types.
Ergocalciferol (Vitamin D2)
- It includes plant-based foods.
- Sources of vitamin D2 are:
- Mushrooms (grown in ultraviolet light)
- fortified foods
- dietary supplements
Cholecalciferol (Vitamin D3)
- Animal-derived foods belong to cholecalciferol.
- It is also the form of vitamin D synthesized by the body.
- Vitamin D3 is twice as effective at raising VD levels in the bloodstream.
- Sources of vitamin D3 are:
- The flesh or fatty fish
- Liver
- Egg yolk
- Butter
- Cheese
- Dietary supplements
Daily requirement
According to the Indian Council of Medical Research (ICMR), the recommended dietary allowances (RDA) for vitamin D is given below.
- Men: 600 IU/d
- Women: 600 IU/d
- Pregnancy and lactation: 600 IU/d
- Infants: 400 IU/d
- Children (1-18 years): 600 IU/d
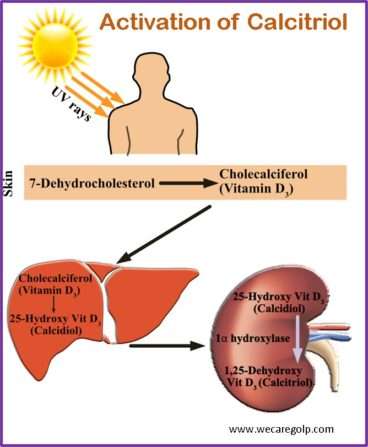
Biosynthesis and activation of vitamin D
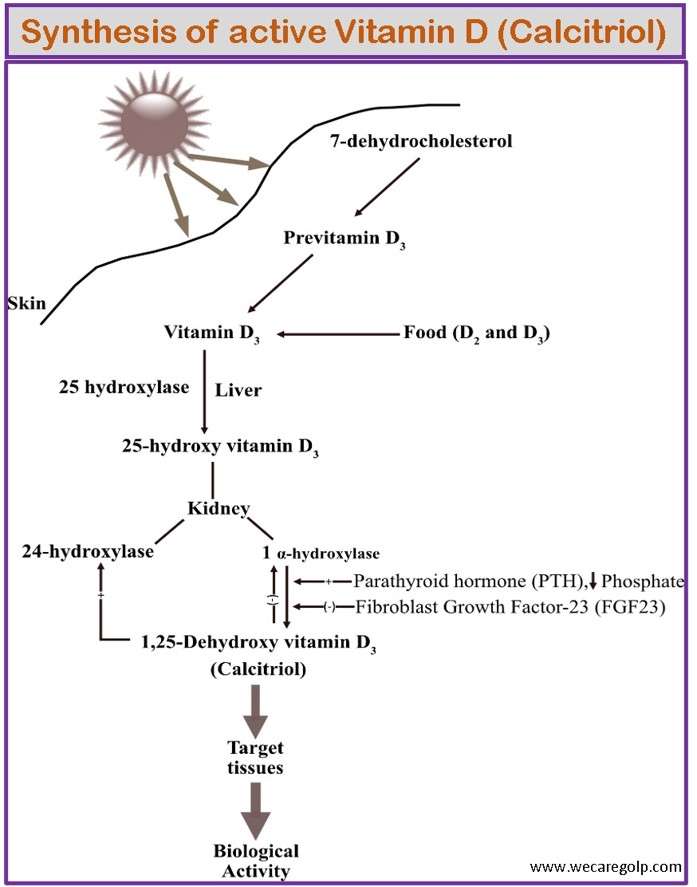
- It is a steroid hormone.
- The precursor molecules of the active form of VD are formed in the skin under the influence of UV radiation (90%) or are absorbed enterally as fat-soluble vitamins (10%).
- Activation occurs in the liver and kidneys.
- The vitamin from sunlight (previtamin D3) and foods (ergocalciferol and cholecalciferol) enter the blood circulation.
- The first hydroxylation step then takes place in the liver and is converted to calcidiol. The synonyms of calcidiol are 25- hydroxycholecalciferol (25-(OH)-cholecalciferol) or 25-hydroxyvitamin D (25-(OH)D).
- Calcidiol can be inactive in the liver under the influence of alcohol, barbiturates, or phenytoin. Determining the plasma concentration of calcidiol provides information about the VD reserves. Its activity is about 1% compared to the active form of VD.
- Calcidiol circulates in the bloodstream. When there is a lack of calcium or phosphate in the plasma, an enzyme 1-α-hydroxylase converts 25-(OH)D into 1.25 dihydroxy vitamin D3 in the kidney. It is an active form of Vitamin D called calcitriol. The synonyms of calcitriol are 1.25 dihydroxy vitamin D (1.25-(OH)2D), 1.25 hydroxycholecalciferol.
- The enzyme 1-α-hydroxylase is stimulated by an increase in plasma parathormone and a drop in plasma calcium and phosphate concentration as well as a decrease in FGF23 (fibroblast growth factor 23).
- The increase in calcitriol in the plasma leads to a “downregulation” of the VD receptors on cell surfaces and promotes the activity of 24-hydroxylase, which produces ineffective metabolites from calcidiol and calcitriol.
Functions of vitamin D
The effects of vitamin D serve to maintain normal plasma calcium and phosphate concentrations (calcium and phosphate regulation).
- Stimulates the absorption of calcium and phosphate in the small intestine
- Inhibits of parathormone (PTH) secretion
- Reduces the renal excretion of calcium in interaction with PTH
- Regulation of osteoblast function
- Promotion of parathormone effects (osteoclast activation and bone resorption), so-called “permissive effect”
- Regulation of hematopoietic cells and presumably also muscle cell functions
- Immunomodulatory functions
Health benefits
Vitamin D, a fat-soluble vitamin has both physical and mental health benefits. These benefits are:
- Builds strong bones and teeth.
- Strengthens the immune system.
- Supports a healthy heart. It helps regulate heart function and reduce blood pressure.
- Helps to reduce the risk of depression.
- Reduces the risk of multiple sclerosis. Studies revealed that people who receive more sunlight exposure and vitamin D from their diet have less risk of multiple sclerosis.
- Might prevent certain types of cancer.
- May improve brain function.
- Regulates insulin levels and supports diabetes management.
- Might support weight loss.
Vitamin D Deficiencies
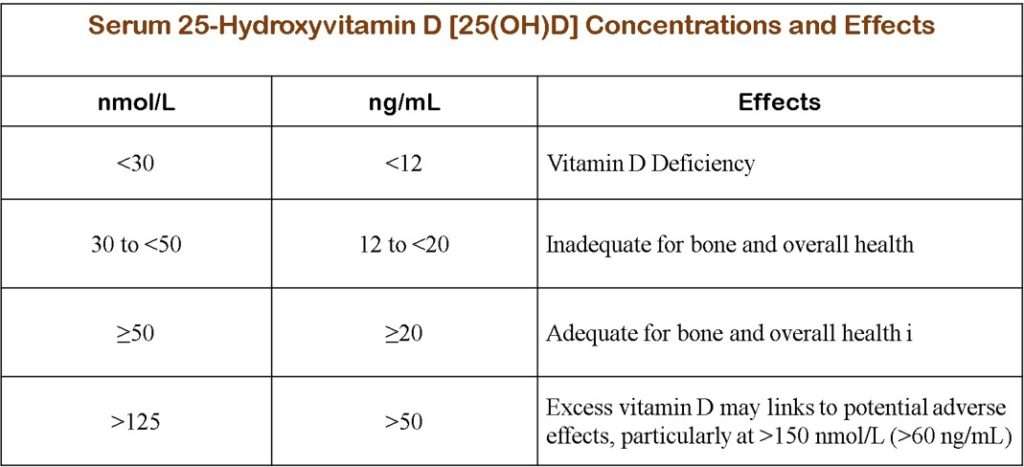
According to the Food and Nutrition Board (FNB) at the National Academies of Sciences, Engineering, and Medicine (NASEM), serum vitamin D (25(OH)D) concentrations less than 30 nmol/L (12 ng/mL) indicate vitamin D deficiency. The deficiency may occur due to several reasons, such as inadequate sunlight exposure, lack of VD in the diet, poor absorption, or higher metabolic rate. Lack of enough vitamin D impacts the formation of healthy and rigid bones. Vitamin D deficits in the long term may result in different health conditions in adults and children.
- Secondary hyperparathyroidism: Patients with long-term VD deficiency can experience symptoms associated with secondary hyperparathyroidism, such as bone pain, arthralgias, myalgias, fatigue, muscle twitching, and weakness.
- Osteoporosis: Chronic VD deficiency weakens the bones and may result in bone fractures in adults.
- Hypocalcemia, Hyperphosphatemia: Low blood calcium (hypocalcemia) and low blood phosphate (hypophosphatemia) may occur
- Osteomalacia (softening of the bones in adults) is the most severe effect of VD deficiency.
- Rickets: It may result softening of bones in children.
Risk group of vitamin D deficiency
- Anyone, including infants, toddlers, and adults.
- People who habitually cover themselves in clothing (such as Muslim women) and have darker skin (higher melanin content), especially in Middle Eastern countries.
- According to The National Institute of Health (NIH), people who work 9 to 5 office jobs are likely to suffer from it as they are less exposed to sunlight.
- Vegans and vegetarians are also prone to vitamin D deficiency as animal-derived foods are the major source of it.
Effects of excess vitamin D
- Intake of too much supplements might result excess VD in the body. The FNB defines excess VD, when serum 25(OH)D is >125 nmol/l (>50 ng/ml).
- Hypercalcemia (total calcium >11.1 mg/dl): It leads to nausea, vomiting, dehydration, loss of appetite, muscle weakness, pain, polyuria, excessive thirst, kidney stones and neuropsychiatric disturbances.
- Hypercalciuria (excess calcium in the urine): It leads to impairment of renal function.
- In extreme cases calcification, cardiac arrhythmias, and renal failure may occur.
- Even a dose of 1000 international units (25 mcg), when administered over an extended period of time, has been found to have toxic adverse effects.
Supplementations
The recommended doses rely on the nature and severity of the deficiency. The recommended daily amount:
- Children up to age of 1 year: 400 international units (IU)
- Between 1 to 70 years: 600 IU
- Over 70 years: 800 IU
- Pregnant and lactating women: 600 IU
Interactions with medicines
- Aluminum: People with renal failure who take VD along with aluminum-containing phosphate binders may lead to aluminum toxicity. VD absorbs essential minerals including aluminum. Reciprocally, aluminum and other minerals can interfere with the renal synthesis of 1.25-dihydroxy VD.
- Anticonvulsants: Phenobarbital and phenytoin (Dilantin, Phenytek) cause an increase in VD breakdown and a decrease in calcium absorption.
- Atorvastatin: The processing of atorvastatin in the body may affect VD intake.
- Calcipotriene: Its combination with calcipotriene increases the risk of hypercalcemia (too much calcium in the blood).
- Digoxin: Avoid taking high doses of VD with digoxin. It may cause hypercalcemia.
- Thiazide diuretics: The risk of hypercalcemia increases when thiazide diuretics are taken with it.
- Steroids: Steroids may reduce calcium absorption and interfere with the body’s utilization of VD.
- Stimulant laxatives: High doses of stimulant laxatives taken over an extended period of time can decrease calcium and VD absorption.
Summary
- Vitamin D is a fat-soluble vitamin which is needed to develop and maintain strong bones.
- Body can only absorb calcium, which is the main building block of bone, in the presence of it.
- Numerous other biological processes in the body are regulated by it.
- Very few foods naturally contain VD. Fatty fish, such as salmon, mackerel, and sardines, fortified milk, and fortified cereals are sources.
- It has numerous benefits. It may aid in weight control, mood improvement, and easing depression symptoms.
- Although much of the UVA radiation will pass through the window glass and may be harmful, the window glass completely blocks UVB rays. VD levels cannot be increased by sitting in front of a sunny window.
References
- https://www.healthline.com/nutrition/vitamin-d2-vs-d3#TOC_TITLE_HDR_4
- https://www.uptodate.com/contents/vitamin-d-deficiency-beyond-the-basics#H13
- https://reference.medscape.com/drug/drisdol-calciferol-vitamind-344417
- https://www.healthline.com/nutrition/vitamin-d-and-vitamin-k#TOC_TITLE_HDR_3
- https://www.mayoclinic.org/drugs-supplements-vitamin-d/art-20363792
- https://my.clevelandclinic.org/health/diseases/15050-vitamin-d-vitamin-d-deficiency
- https://www.livescience.com/benefits-of-vitamin-d
- https://www.msdmanuals.com/home/disorders-of-nutrition/vitamins/vitamin-d-excess https://www.uptodate.com/contents/vitamin-d-deficiency-beyond-the-basics#H2
- https://medlineplus.gov/vitaminddeficiency.html
- https://www.hsph.harvard.edu/nutritionsource/vitamin-d/
- Institute of Medicine; Food and Nutrition Board; Committee to Review Dietary Reference Intakes for Vitamin D and Calcium; A. Catharine Ross, Christine L. Taylor, Ann L. Yaktine, and Heather B. Del Valle, Editors, 2011, https://pubmed.ncbi.nlm.nih.gov/21796828/