Introduction
- Meningococcal disease is a serious illness caused by the Gram-negative bacterium Neisseria meningitidis and can cause inflammation of lining of brain and spinal cord (meningitis) and septicemia (blood poisoning), or a combination of these diseases.
- N. meningitidis can be classified into 13 different serogroups based on its capsular polysaccharide: A, B, C, D, H, I, K, L, X, Y, Z, 29E and W135. Serogroups A, B, C, W135, X, and Y account for Meningococcal disease worldwide.
- It is a contagious disease, transmitted from person to person by upper-respiratory tract secretions (droplet infection), associated with high case fatality rates and long-term sequelae among survivors.
- Despite treatment, at least 5-10% of patients with meningococcal die within 1 or 2 days of onset and 10-20% of survivors develop neurological sequelae.
Incidence
- According to the Centers for Disease Control and Prevention (CDC), meningococcal disease has the highest incidence in the meningitis belt of sub-Saharan Africa (stretching from Senegal in the west to Ethiopia in the east). Epidemics occur every 5 to 12 years, with incidence rates reaching 1000 cases per 100,000 population.
- The annual incidence rate in other regions of the world experience averages around 0.3 to 3 per 100,000 population. The rate of disease is higher in children younger than one year old.
Types of Meningococcal Disease
Meningitis
- Meningococcal meningitis is a form of bacterial meningitis.
- It results from inflammation and irritation of the meninges and the membranes surrounding the brain and spinal cord.
- The bacteria invade the cerebrospinal fluid and circulate through the central nervous system.
- Meningococcal bacteria can multiply freely in CSF and release poisons causing inflammation and swelling of the meninges and brain tissue itself.
- This inflammation can begin suddenly (acute) or may develop gradually (subacute).
- Meningococcal meningitis is associated with a high mortality rate and persistent neurological defects, mostly among infants and young children.
Meningococcemia (Meningococcal septicemia)
- It is an infection that affects the blood and may involve other parts of the body.
- When meningococcal bacteria invade blood stream it starts producing poisons, and poison begins to attack the lining of blood vessels.
- It can cause disseminated intravascular coagulation (DIC), inappropriate blood clotting within the vessels.
- Ischemic tissue damage occurs because of DIC, and upstream thrombi obstruct blood flow.
- Small bleeds occur on the skin causing rashes that appear star-like shape.
Other types
Meningococcal pneumonia
- It can appear during influenza in military camps.
- It is rapidly evolving pneumonia sometimes associated with septic shock.
- Prognosis is excellent with prompt treatment.
Signs and symptoms of Meningococcal Disease
Patient with meningococcal meningitis presents with following symptoms
- High fever
- Nuchal rigidity (stiff neck)
- Kernig’s sign (stiffness of the hamstrings muscle)
- Severe headache
- Vomiting
- Purpura
- Photophobia
- Sometimes altered mental status or seizure may occur
Patient with meningococcemia presents with following symptoms
Initial symptoms include
- Fever
- Nausea
- Myalgia
- Headache
- Arthralgia
- Chills
- Diarrhea
- Stiff neck and malaise
Later symptoms include
- Septic shock
- Purpura
- Hypotension
- Cyanosis
- Petechial rash-star like shape
- Seizure
- Anxiety
- Multiple organ dysfunction
- Acute respiratory distress syndrome
- Altered mental status
Risk factors
Anyone can get meningococcal disease but certain people are at risk, including
- Infants younger than 1 year of age
- Adolescence and young adult age (16-23 years)
- People with certain medical conditions that affect immune system such as HIV.
- Microbiologist who routinely works with isolates of Neisseria meningitides.
- Sudden outbreak in the community.
- People travelling to a country where meningococcal disease is epidemic or highly endemic.
- College students who stay in residence halls.
- Military recruits.
- Anyone who has skipped routine recommended vaccinations.
Pathophysiology
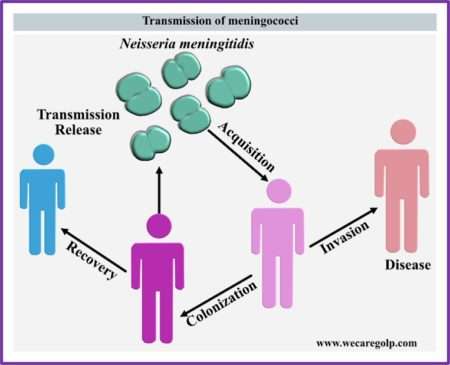
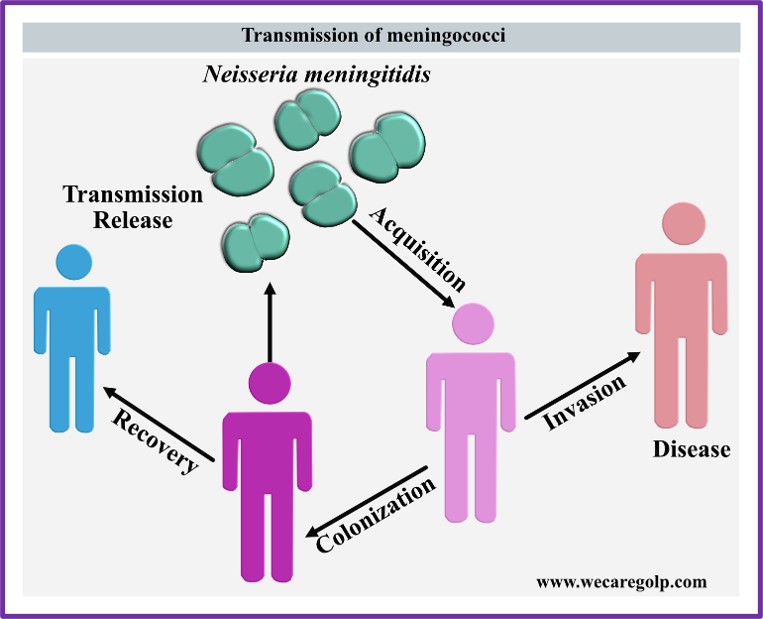
- Meningococci are transmitted from person to person through direct contact with large respiratory droplets or secretions.
- 10% of the human population harbors meningococci in the nasopharyngeal mucosa.
- Invasive disease (relatively rare) occurs when people come in contact with a virulent strain, followed by colonization by that strain, penetration of the bacterium through the mucosa, survival, and outgrowth of the meningococcus in the bloodstream.
- Once the meningococcus reaches the bloodstream, its outgrowth depends on the absence of specific antibodies. Then, the bacteria can spread through the blood to cause systemic disease and cross the blood-brain barrier into the cerebrospinal fluid (CSF) to cause meningitis.
Transmission of Meningococcal Disease
- Meningococcal disease is transmitted by contact with spit, phlegm or other fluid from nose and mouth from the affected person.
- Kissing, mouth to mouth resuscitation
- Living in crowd place
- Sneezing or coughing
- Sharing eating or drinking utensils used by affected person.
Diagnosis of Meningococcal Disease
Besides, careful medical history, physical examination and tests, other common tests include:
Blood culture
- Growth of bacteria from specimens of blood or cerebrospinal fluid.
Imaging
- CT scan or MRI of the head is the most sensitive modality.
- Microscopic examination of cerebrospinal fluid (CSF) gives prompt diagnosis of meningococcal disease.
- Fluid of infected person usually shows a low sugar level, increased white blood cells count and increased protein.
Treatment of Meningococcal Disease
- Because of its severe risks of morbidity and dealth, the suspected patients need immediate treatment.
- Treatment in primary care include intramuscular administration of benzylpenicillin and then urgent transfer to hospitals.
- In hospital, Intravenous (IV) broad spectrum 3rd generations antibiotics (cefotaxime, Benzylpenicillin, Chloramphenicol) are administered.
- Supportive measures are also provided and it include
- IV fluid administration
- Oxygen therapy
- Inotropic support- e.g. dopamine or dobutamine and management of increased intracranial pressure.
- Some patients may require steroid therapy.
Complications
Early complication
- Raised intracranial pressure
- Seizure
- Disseminated intravascular coagulation
- Circulatory collapse
- Organ failure.
Later complications
- Deafness
- Blindness
- Lasting neurological deficits
- Reduced IQ
- Gangrene leading to amputation
Prevention of Meningococcal Disease
- Vaccination-Many licensed vaccines are available for meningococcal disease. The highest age specific incidence is prevalent in children under one year. Vaccination will be most effective when it can be given in infancy, ideally with other childhood vaccines. Anyone suffering from an acute illness requiring treatment should not be vaccinated. Likewise, anyone suffering from sensitivity to component of the vaccine should not be vaccinated.
- Chemoprophylaxis- Regardless of immunization status, antimicrobial chemoprophylaxis should be given to people who come in close contact of patients with meningococcal disease. Close contacts include: those living in the same house, childcare center contacts, person directly exposed to an infected patient’s oral secretion in a week before symptom onset.
Types of vaccines
There are three types of vaccine available:
1.Meningococcal Polysaccharide vaccine
- Meningococcal vaccines are bivalent (A and C), trivalent (A, C, W) or tetravalent (A, C, W, Y) and composed of purified heat stable lyophilized capsular polysaccharide.
- Polysaccharide vaccines are good option to control epidemic outbreaks produced by the specific serogroups.
- Given in a single dose, starting at 2 years of age.
- Adults (including older adults 56 years and above) can get this vaccine.
2.Meningococcal Conjugate vaccine (Menactra®, Menveo®, and MenQuadfi®)
- Conjugate vaccines are available as monovalent vaccines (serogroup A or C), bivalent vaccines (serogroups A, and C) and tetravalent vaccines (serogroups A, C, W, and Y).
- Conjugate vaccines compose of conjugating the diphtheria toxoid or a non-toxic mutant of diphtheria toxin or tetanus toxoid protein.
- This conjugation allows the immune system of children under 2 years to identify the protein and produce a long-lasting antibody response.
- Given in two doses starting at 2 months of age and given 2 months apart.
- A booster dose is needed after 1 year of age.
- Teenagers and adult receive one dose of the conjugate meningococcal vaccine.
- For the meningococcal vaccine combined with the haemophilus B vaccine, three doses are recommended at 2, 4, and 6 months.
- A booster dose is also recommended between 12 and 15 months of age.
3.Serogroup B meningococcal or MenB vaccines (Bexsero® and Trumenba®)
- Meningococcal B vaccines are recommended for people 10 years or older who are at risk for serogroup B meningococcal disease.
- The vaccine may also be given to anyone 16 through 23 years old to provide short-term protection against most strains of serogroup B meningococcal disease.
- The preferred age for vaccination is 16 through 18 years.
Summary
- Meningococcal disease is a serious contagious bacterial infection between people to people through mucus that can result in organ damage or death.
- Once a meningococcal patient is identified, it is essential to control the transmission of meningococcus by administering chemoprophylaxis to close contact of patient.
- The treatment should be started as soon as disease is diagnosed because the sooner people receive treatment, the less damage the disease may cause because it is an unpredictable infection that can progress very rapidly despite of best treatment.
- It has high mortality rate if untreated but preventable with vaccines.
- Immunization against meningococcal disease prevent it.
References
- World Health Organization. Control of epidemic meningococcal disease: WHO practical guidelines. World Health Organization;
- CDC Traveler’s Health: Meningococcal disease.
- Rosenstein NE, Perkins BA, Stephens DS, Popovic T, Hughes JM. Meningococcal disease. New England journal of medicine. 2001 May 3;344(18):1378-88. DOI: 10.1056/NEJM200105033441807
- Presa J, Serra L, Weil-Olivier C, York L. Preventing invasive meningococcal disease in early infancy. Human Vaccines & Immunotherapeutics. 2022 Nov 30;18(5):1979846.