Recirculation
Recirculation in hemodialysis occurs when blood that has already been dialyzed is fed back into the dialyzer.
- During recirculation, dialyzed blood, or part of it flows back into the extracorporeal circuit.
- This amount of blood can no longer participate in the exchange of substances or loading in the systemic circulatory areas.
- The recirculation therefore mixes with blood that has not yet been dialyzed and reduces the diffusive gradient of the blood in the dialyzer.
- This leads to a loss of effectiveness.
Causes of Recirculation in Hemodialysis
- Various factors can affect dialysis recirculation.
- However, it may sometimes cause due to only one reason and sometimes, more factors play role together.
- Inadequate arterial blood flow, the presence of high-grade venous stenosis and improper vascular cannulation by dialysis staff during dialysis are the most common causes of access recirculation.
- The different reason for recirculation in hemodialysis are described below.
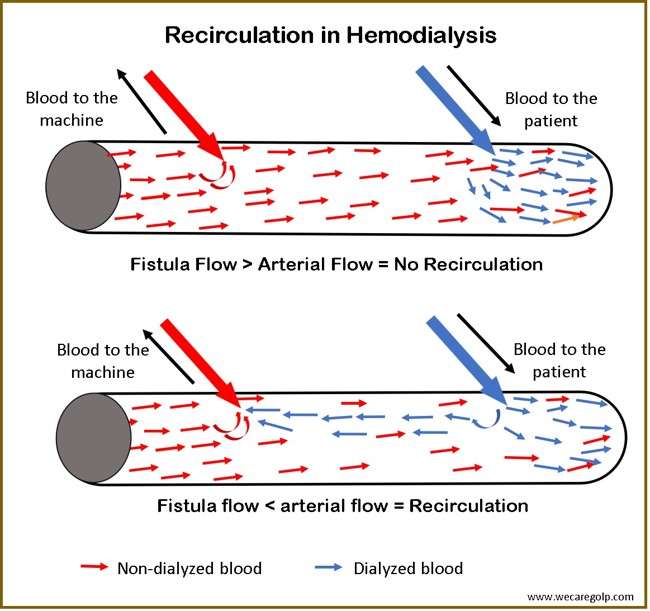
Fistula-Related Recirculation
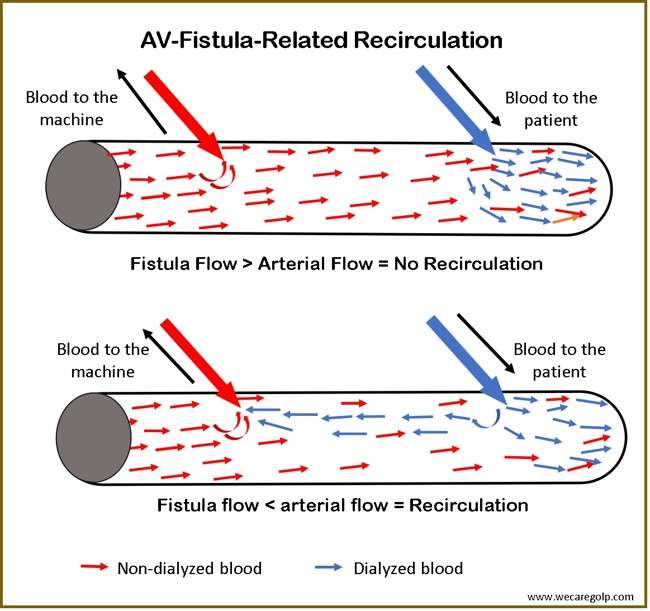
- The recirculation caused by the fistula always depends on the altered fistula conditions.
- The recirculating blood volume has no opportunity to be loaded again with uremic toxins and liquid in the body’s circulation system.
- As a result, the quality of dialysis will reduce, and the risk of thrombosis increases in the extracorporeal system.
- Blood that has already dialyzed is pumped back into the extracorporeal blood circuit if the fistula flow is less than the blood flow.
- Disturbed blood outflow can also transport the dialyzed blood to the dialyzer again during the withdrawal phase.
- Furthermore, a flow disturbance in the vascular system, e.g., stenosis, can lead to increased recirculation.
- In practice, the blood pump should adapt to the fistula conditions and, if necessary, need to intervene to improve this condition (fistula consultation, etc.).
Cardiopulmonary Recirculation
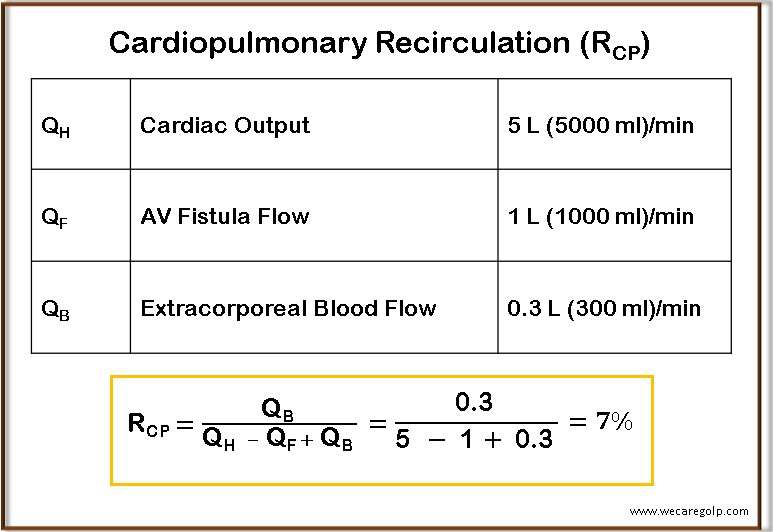
- Cardiopulmonary recirculation arises in the arteriovenous fistula.
- Normally, arterial blood uses for dialysis via the fistula and passes through the extracorporeal circuit.
- After the blood purifies through the dialyzer, it no longer returns to the arterial system but is fed into the venous system. It means it is supplied directly to the cardiopulmonary system.
- As a result, approximately 3-15% of the purified blood return to the extracorporeal dialysis circuit without take part in the transport or exchange of substances in the capillary system.
- Undoubtedly, cardiopulmonary recirculation is always present in a fistula.
- On the contrary, central venous catheters (or atrial catheters) do not have cardiopulmonary recirculation. Here, the blood for dialysis withdraws from the venous system (atrium) and returns to the same vein. Therefore, the dialyzed blood can fully participate in the exchange of substances in the body systems.
Blood Tubing System-Related (extracorporeal circuit) Recirculation
- Blood tubing system-related recirculation occurs in single-needle (SN) dialysis.
- There is always the withdrawal phase (arterial phase) and return phase (venous phase) with the help of a blood pump in standard hemodialysis, where there is no possibility to mix the dialyzed and non-dialyzed blood in the tubing system.
- But in SN dialysis, on the other hand, only one cannula is used.
- Therefore, the chance of mixing blood is certainly there.
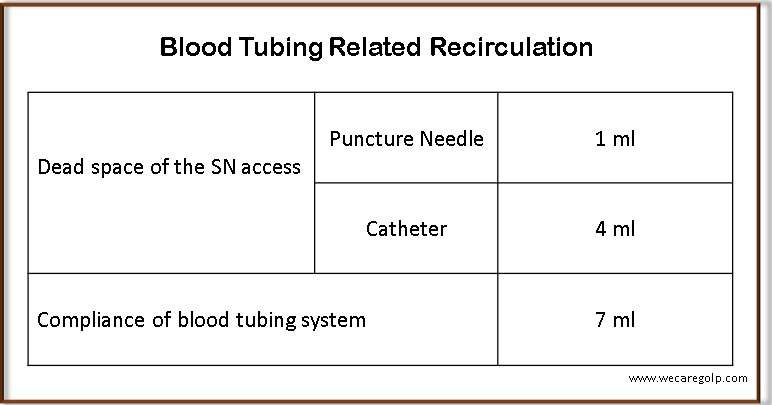
The Vascular Access
- After a venous phase (return phase), dialyzed blood remains in the needle or catheter.
- It is called the dead space of access.
- This blood is drawn back into the extracorporeal system during the arterial phase.
- The amount varies depending on vascular access.
The Blood Tubing System
- Furthermore, the blood tubing system also contributes to recirculation. It is also called compliance.
- Since the diameter of the puncture cannula or catheter is considerably smaller than that of the blood tubing system, the blood pumped by the venous pump in the return phase cannot flow directly back into the vascular access.
- It causes a certain backflow of blood into the arterial tubing system and returns to the dialyzer in the arterial phase (withdrawal phase).
Recognizing Recirculation during Hemodialysis
- The arterial blood becomes light in color due to dilution with saline, and the extracorporeal blood darkens due to thickening of blood during dialysis.
- In the bedside laboratory, abnormally low potassium or elevated ACT values may be present.
- Unusual values for the Arterial negative pressure or the venous return pressure also suggest recirculation.
- If one presses the fistula-vein between the arterial and venous cannula with a pencil or ballpoint pen, the pressures should not change significantly if the fistula conditions are correct. If the venous pressure rises, indicating proximal outflow stenosis (after the venous needle). If the Arterial negative pressure drops, it indicates inflow stenosis (before the arterial needle).
- Latest dialysis machines offer the possibility to measure recirculation during treatment. Blood Temperature Monitoring (BTM) module from FMC (Fresenius Medical Care) works with the principle of thermodilution. The Transonic device uses ultrasound method along with saline bolus.
Measuring Method of Recirculation in Hemodialysis
Urea based
- P – A / P – V × 100
- P = the systemic urea concentrations in the peripheral blood,
- A = blood entering the arterial line, and
- V = post-dialyzer venous circuit
Non-urea based
- Blood Temperature Monitoring (BTM) – Thermodilution method
- Transonic – Ultrasound
The K/DOQI (2006) guideline suggests that in an arterio-venous fistula, urea-based recirculation of greater than 10% requires further investigation. However, the non-urea-based techniques are preferred.
Prevention of Recirculation in Hemodialysis
- The needles need to place 5 -7 cm apart
- An effective blood pump
- Correct cannulation
- Do not exchange the arterial and venous needles while connecting with the extracorporeal system
- Find the fistula-related problems (e.g., stenosis) timely
- Monitor the access recirculation regularly
- Blood flow should be less than fistula flow
Complications of Recirculation in Hemodialysis
- Inadequate dialysis (low effectiveness of hemodialysis)
- Thrombosis
- Cardiac problems