Introduction
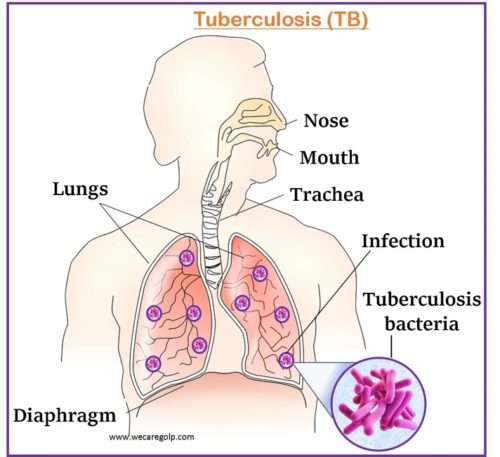
Tuberculosis (TB) is a potentially fatal contagious disease primarily affecting lung parenchyma. In most cases, an acid-fast bacillus (AFB), Mycobacterium tuberculosis causes TB. TB, a multi-systemic disease with a wide range of manifestations and presentations, is the leading cause of infectious disease-related mortality worldwide. Approximately 30% of people worldwide are infected with this pathogen, with the vast majority carrying a dormant infection.
- M. tuberculosis is an acid-fast, slowly growing bacteria that can survive in macrophages, allowing for a latent infection that can remain asymptomatic for decades.
- The bacteria usually attack the lungs, but they may spread to any part of the body including meninges, kidney, bones, lymph nodes, etc.
- As one of the most common human infections, it has a significant global impact on sickness and mortality.
- When an infected individual coughs or sneezes, tiny droplets of saliva are inhaled, which spread the disease.
- It is a persistent, granulomatous bacterial illness that spreads slowly and is characterized by weight loss.
- After HIV/AIDS, TB is the second most prevalent infectious disease-related cause of mortality worldwide.
Incidence
- According to the WHO, 1.6 million individuals worldwide passed away from TB in 2021 (including 187, 000 people with HIV). Following COVID-19 (behind HIV/AIDS), TB is the second-leading infectious killer in the world and the 13th-leading cause of death overall.
- In 2021, there were 10.6 million cases of tuberculosis (TB) reported worldwide. TB affects 6,400,000 men, 3,400,000 women, and 1.2,000,000 children worldwide.
- Globally, 1.2 million children will have contracted TB in 2021. It is difficult to identify and treat TB in children and adolescent due to ignorance from health personals
- In 2021, 87% of all new cases of TB occurred in the 30 countries with the highest TB burden
- TB incidence is decreasing at a rate of 2% per year worldwide, and between 2015 and 2020, there was an overall 11% decrease. This was close to the 20 percent reduction target set by the End TB Strategy between 2015 and 2020.
- Between 2000 and 2020, the detection and treatment of TB is predicted to have saved 66 million lives.
Classification
- Pulmonary Tuberculosis
- Extrapulmonary Tuberculosis
- Lymph nodes TB
- Skeletal TB
- Genitourinary TB
- Miliary TB
- Gastrointestinal TB
- Tuberculous Meningitis
Stages of Tuberculosis
Primary TB infection
- At this point, bacteria enter the body for the first time.
- Most people affected by this have no symptoms, a negative skin test, and a normal X-ray. Although, a few (with a low immune system) may develop a fever or pulmonary problems.
- According to the Centers for Disease Control and Prevention (CDC), most initial TB infections are asymptomatic and are followed by a latent TB infection.
Latent TB Infection (LTBI)
- People with LTBI have TB germs in their bodies but they do not exhibit any signs of the disease. They also cannot transmit bacteria to others.
- However, if LTBI is not treated timely and bacteria become active and multiply in the body, LTBI develops TB disease.
- The patients may have a positive skin test, but a normal chest X-ray.
- The immune system of the afflicted person blocks the TB organisms, and the TB is dormant throughout the life.
Active TB Disease
- The TB bacteria are growing and actively spreading.
- You will feel poorly and spread illness to others.
- This phase describes a person exhibiting symptoms of an infection that is currently active.
- Both the chest X-ray and the skin test would come back positive for the individual.
- It is critical to seek treatment as soon as possible to minimize problems and the spread of the infection.
Causes of Tuberculosis
- Most common
- Mycobacterium tuberculosis which is commonly known as “Koch’s bacillus” or tubercle bacilli or acid-fast bacillus (AFB) is the bacteria responsible for TB.
- They circulate through the air. Despite not spreading quickly, TB is contagious.
- Usually, you must spend a lot of time around an infectious individual to get it.
- Others
- M. Aviumintracellulare
- M. Scrofulaceum
- M. chelonei
- M. Marinum
- M.ulcerence
- M. Kansasi
- M. Fortuitum
Risk factors of Tuberculosis
People of all ages, races, and income levels are impacted by TB. Those who are more vulnerable include:
- Close proximity to a TB patient.
- State of immune suppression (elderly, cancer)
- Alcoholism and drug addiction
- People who do not have access to proper healthcare
- Existing medical conditions (chronic renal failure, diabetes mellitus)
- Immigrants from nations with a higher TB incidence.
- Institutionalization (long-term care facilities)
- Living in poor conditions
- Healthcare professionals that interact with high-risk populations
- The elderly
- People with recent tubercular infection (within the last two years).
Mode of Transmission
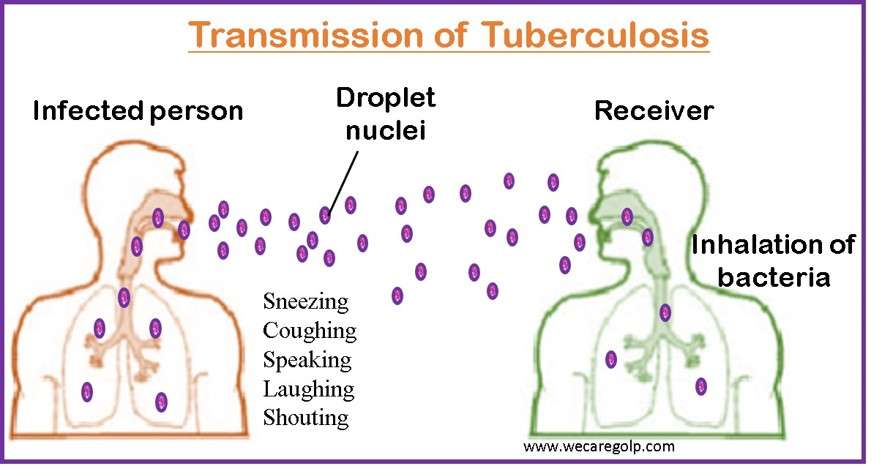
- The transmission of M. tuberculosis occurs when droplet nuclei are inhaled and reach the alveoli of the lungs through the nasal passages, the respiratory tract, and the bronchi.
- Coughing, speaking, laughing, sneezing, shouting, and other respiratory activities can cause another person to breathe in the bacteria and become infected.
Incubation period
- The interval between exposure and the establishment of a positive tuberculin skin test is considered the incubation period for tuberculosis.
- The average person’s incubation period lasts between two and twelve weeks.
- Disease progression is influenced by
- Proximity of contact,
- Disease extent, and
- Sputum positivity.
- The time frame for incubation can range from weeks to years.
Signs and Symptoms of Tuberculosis
The following are the standard clinical signs and symptoms of active pulmonary TB (older people with TB may not have these signs and symptoms).
- Cough
- Anorexia
- Loss of weight
- Fever
- Night sweats
- Chest discomfort and hemoptysis (which can also result from tuberculous acute pericarditis)
- Fatigue
Tuberculous meningitis
- A low-grade or absent fever
- A headache that has been intermittent or constant for two to three weeks
- Minor mental status changes that could lead to coma
Skeletal TB
- Back stiffness or pain
- Pott disease, which may cause lower-extremity paralysis in up to 50% of patients
- Tuberculous arthritis, which often affects just one joint (most often the hip or knee, followed by the ankle, elbow, wrist, and shoulder)
Genitourinary TB
- Dysuria
- Pain in the flank
- Frequent urination In women
- Symptoms resembling pelvic inflammatory disease in men include a painful scrotal lump, prostatitis, orchitis, or epididymitis.
Gastrointestinal TB
- Mouth ulcers or sores that do not heal
- Swallowing issues (with esophageal disease)
- Stomach pain that appears to be caused by a peptic ulcer (with gastric or duodenal infection)
- A lack of absorption (with infection of the small intestine)
- Hematochezia
- Diarrhea (with infection of the colon)
Other extrapulmonary symptoms
Depending on the tissues affected, extrapulmonary TB symptoms can include the following:
- Coma
- Neurologic Impairment
- Confusion
- Chorioretinitis
- Lymphadenopathy
Pathophysiology
- The receiver inhales aerosol droplets through coughing, sneezing, etc. from the infected person.
- In the lungs, drops are left behind.
- The growth of microorganism takes place within alveolar macrophages.
- A tubercle (a granulomatous formation) arises as a result of the cytokines that macrophages secrete.
- The tuberous sclerosis enlarges into the lung parenchyma, causing Ghon’s complex
- Bacteria can then spread to the draining lymph nodes, causing lymphadenopathy.
- Ghon’s complex and lymphadenopathy/calcification lead to Ranke complex.
- If the spread is not controlled by the immune cells, bacteremia with seeding of other organs may occur, causing military TB.
- A caseating granuloma, or erosion of germs into the airways, renders the patient contagious.
- Spontaneous eradication is uncommon, and infection can advance to a chronic stage with bouts of healing and subsequent scarring of the lesions.
Diagnosis of Tuberculosis
Health History
- HIV status
- Infection history with TB
- Former TB therapy illness symptoms exposure
- Demographic TB risk factors
- Other medical disorders, such as diabetes, also raise the likelihood of developing TB illnesses
Physical assessment
- Clumping of the fingers or toes (in patients with advanced disease)
- Enlarged or sensitive lymph nodes in the neck or other places
- Inflamed pleura
- Weird breath sounds (crackles)
Tuberculin Skin Test (TST)

- It is also called Mantoux tuberculin skin test.
- It needs two visits.
- On the first visit:
- The test is performed by injecting 0.1 ml fluid (called tuberculin) into the skin of the lower arm.
- The second visit is made after 48-72 hours after the first visit to check the skin reaction. Diagnosis is based on the size of the wheal response (circular, raised shape).
- <5mm —-negative
- 5mm – 9 mm — hypersensitive to tuberculin protein (previous TB infection)
- >10mm —- positive for TB infection
Blood Test
- It is called interferon-gamma release assays (IGRAs).
- In combination with TST, IGRAs can increase sensitivity.
- The blood test measures the reaction of the immune system to the TB-causing organisms. The positive result confirms the LTBI or active TB disease more precisely.
Other Diagnostic Tests
If skin and blood tests indicate further analysis in case of active disease and lung infection, the following additional test will be done.
- Biopsy of the afflicted area
- Bronchoscopy
- Chest Xray: It helps to detect the following.
- Lymphadenopathy
- Ghon’s complex (lesion in the lung)
- The Assmann focus (infraclavicular infiltration)
- Inflamed pleura
- Apical and upper segments of the lower lobes have infiltrates
- Cavities with layers of air-fluid
- CT scan (computed tomography)
- It is more delicate than a simple X-ray. When a chest X-ray is non-specific, it is recommended for a better view of the lungs or in the case of spinal TB.
- This could reveal abnormalities in the lungs brought on by active tuberculosis or white areas in the lungs where the immune system has walled off the TB bacteria.
- Thoracentesis
- It is a procedure to remove fluid or air from the pleural space.
- It is done in case of severe and long-term infection.
- Sputum smear and culture
- 3 samples of sputum must be taken for smear testing and culture.
- A positive AFB result does not support a TB diagnosis because some AFB are not M. tuberculosis.
- Therefore, all initial samples should undergo a culture to confirm the diagnosis.
- However, starting, or continuing treatment for TB does not always require a positive culture.
- The diagnosis of tuberculosis is confirmed by a positive culture for M. tuberculosis. Regardless of the results of the AFB smear, all specimens should be subjected to culture examinations.
- QuantiFERON Gold test
- After the blood has been exposed to antigens from M. tuberculosis proteins, the QuantiFERON Gold test analyses interferon-gamma in the test subject’s blood.
Treatment of Tuberculosis
The major aims of TB treatment are to:
- Cure the patient
- Reduce the danger of disability or death
- Stop transmission to others
- Provide the safest, most effective treatment in the shortest amount of time.
First-line drugs
- Isoniazid (INH)
- Rifampin (RIF)
- Pyrazinamide (PZA)
- Ethambutol (EMB)
- Rifapentine (RPT)
Second-line drugs
- Streptomycin (IM)
- Capreomycin
- Aminosalicylic acid
- Cycloserine
Drug-Susceptible TB Disease Treatment Regimens
According to the CDC, there are various recommended treatment plans for TB illnesses. Depending on the regimen, the duration of TB therapy might range from 4 to 9 months. Treatment plans for TB include
The 4-month TB Therapy Regimen
- This regimen includes
- High-dose daily rifapentine (RPT)
- Isoniazid (INH)
- Moxifloxacin (MOX) and
- Pyrazinamide (PZA).
- The intensive phase of the 4-month rifapentine-moxifloxacin regimen lasts for two months, while the continuation phase lasts for two months and one week (total of 17 weeks for treatment).
- It is recommended for people
- Ages 12 and older with body weight at or above 40 kg,
- With pulmonary TB but unknown organisms,
- Suspected to be drug-resistant, and
- Who have no contraindications to this regimen.
- In the treatment of drug-susceptible TB disease, this regimen is as effective as the standard daily 6-month regimen.
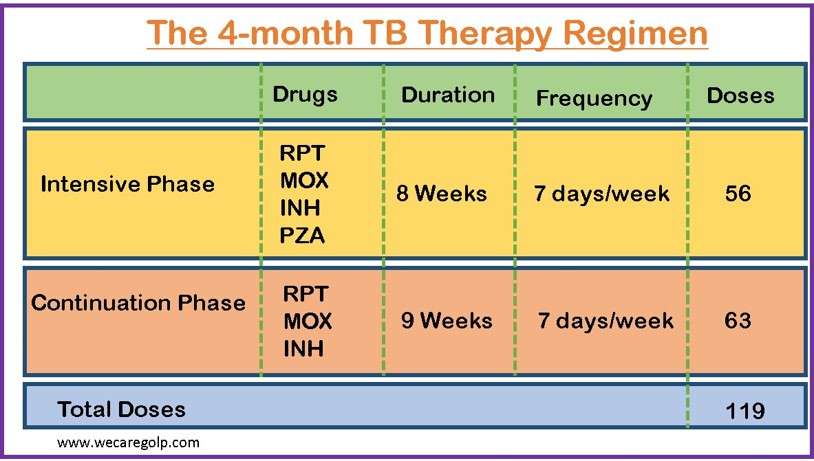
- Treatment must be completed within 70 days of treatment initiation.
- If this target is not met, the patient should be considered to have interrupted therapy and should be managed following TB treatment guidelines.
- At least 5 of the 7 weekly doses should be administered under direct supervision. Directly observed therapy entails a healthcare worker watching the TB patient swallow each dose of the prescribed drugs.
- The healthcare worker should ask the patient how he or she is feeling, double-check the medications before administering them, inquire about any side effects, and answer any questions the patient may have.
- Pyridoxine (vitamin B6), 25–50 mg/day, should be given to all patients in addition to isoniazid.
The 6 to 9-month TB Therapy Regimen
The 6- to 9-month RIPE TB treatment regimens include
- Rifampin (RIF),
- Isoniazid (INH)
- Pyrazinamide (PZA)
- Ethambutol (EMB)
RIPE regimens for treating tuberculosis (TB) have a 2-month intensive phase followed by a 4- or 7-month continuation phase (a total of 6 to 9 months for treatment).
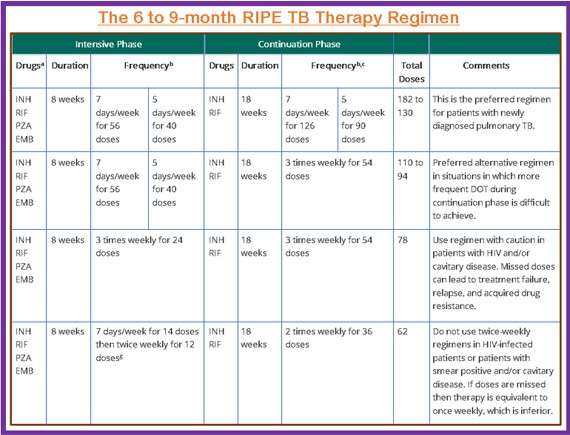
- When using directly observed therapy (DOT), drugs can be given 5 days a week, with the number of doses adjusted accordingly.
- Patients with cavitation on the initial chest radiograph and positive cultures at the end of the first two months of therapy should be given a seven-month (31-week) continuation phase.
- Pyridoxine (vitamin B6), 25–50 mg/day, is administered in conjunction with INH to all patients at risk of neuropathy (e.g., pregnant women, breastfeeding infants, persons with HIV, patients with diabetes, alcoholism, malnutrition, or chronic renal failure, or patients with advanced age).
The regimen is recommended to be completed in 9 months by administering all of the specified doses for the intensive phase within 3 months and those for the 4-month continuation phase within 6 months.
Multidrug-resistant tuberculosis
- Multidrug-resistant tuberculosis (MDR-TB) is resistant to both isoniazid and rifampin (and possibly other drugs).
- When MDR-TB is suspected, begin treatment empirically before culture results are available; if possible, obtain molecular drug susceptibility testing.
- Based on the susceptibility results, modify the initial regimen as needed. Never add a single new medication to an already failing regimen.
- Administer at least 5 drugs during the intensive phase of treatment and at least 4 drugs during the continuation phase.
Drugs of Choice
- A fluoroquinolone, preferably levofloxacin or moxifloxacin
- Bedaquiline
- Clofazimine
- Clofazimine
- Cycloserine
- Streptomycin or amikacin are preferred aminoglycosides.
- Ethambutol
- Pyrazinamide
- Delamanid
- Delamanid
- Para Aminosalicylic acid (PAS)
DOTS (Directly Observed Therapy, Short –Course)
- DOT is a component of case management that aids in the retention of patients on therapy.
- It is the process by which a trained healthcare practitioner or another trained designated person observes and documents a patient’s swallowing of anti-TB drugs.
- The CDC recommends DOT as the preferred core management strategy for treating TB disease and, if resources allow, for treating latent tuberculosis infection (LTBI).
- DOT can help prevent the development of drug resistance, treatment failure, and relapse after treatment has ended.
- Effective DOT is facilitated by good case management, which includes establishing a relationship with the patient and addressing barriers to adherence.
Complications
Tuberculosis can be lethal if it is not treated. Although an untreated active illness typically affects your lungs, it can also harm other areas of your body.
These are some effects of tuberculosis:
- Spinal pain– One of the most frequent side effects of tuberculosis is back pain and stiffness.
- Joint injury. Hips and knees are typically the sites of tuberculous arthritis.
- Meningitis– This may result in weeks of ongoing or sporadic headaches as well as potential mental disturbances.
- Issues with the liver or kidneys. Your kidneys and liver aid in cleansing your bloodstream of pollutants and trash. These organs’ functions may be hampered by tuberculosis.
- Heart Disease– Rarely, tuberculosis can cause swelling and fluid accumulations in the tissues surrounding your heart, potentially interfering with your heart’s normal function.
- Significant lung destruction
- Horner’s syndrome: Itis caused by injury to the cervical sympathetic ganglia.
- Acute respiratory distress syndrome
- Empyema
- Pneumothorax
- Systemic amyloidosis
Prevention
- The best way to avoid TB infection is to keep your immune system healthy and avoid contact with someone who has active TB.
- Identifying and treating cases of latent tuberculosis before the disease becomes active is also critical, particularly in high-risk populations.
- Improving ventilation in indoor spaces can reduce bacteria in the air
- Using germicidal UV lamps can kill airborne bacteria in buildings with high tuberculosis risk people.
- Patients using directly observed therapy (DOT) should be monitored by their healthcare providers, to increase the likelihood of successful treatment.
- Some hygiene measures can prevent infection.
- Thoroughly and frequently wash your hands
- Coughing into your elbow or putting your hand over your mouth while coughing.
- Avoiding close contact with other people
- Do not return to work or school until your healthcare provider has cleared you.
Vaccination
- The BCG (Bacilli Calmette-Guerin) is a live vaccine against tuberculosis.
- Currently, the only licensed TB vaccine is BCG.
- It is one of the most widely used vaccines on the planet and is 80% effective in preventing tuberculosis.
Dosage and vaccination schedule
- Child: 0.05 ml /ID single dose as soon as possible after birth
- Children older than one year: 0.1 ml single dose
Prognosis
- People who receive therapy on time and finish the course without skipping any medication perform very well and recover completely.
- About half of those with active TB eventually pass away from the infection if it is untreated.
- Compared to most other bacteria, TB bacteria reproduce rather slowly. As a result, active TB usually results in a disease that deteriorates gradually.
- Without medical intervention, some people manage to live and even fully recover.
- In immune-compromised patients, TB spreads more quickly and extensively, and if it is not properly and aggressively treated, it can be fatal.
- The rate of tuberculosis recurrence is very low and ranges from 0 to 14%. The long-term prognosis for those who have had tuberculosis in the past and have it again is not always favorable, though.
- The prognosis for tuberculosis in the elderly or those with weakened immune systems is also not good.
Tuberculosis and HIV
- Globally, the number of people infected with HIV and tuberculosis is rising.
- HIV damages the body’s immune system, hastening the progression of tuberculosis into a life-threatening condition.
- If an infected person has HIV, the projected 10% activation rate of dormant TB infection throughout their lifetime increases to 10% activation in one year. Opportunistic infections are the most common cause of death in HIV-positive people.
- People who have both HIV and TB are 25–30 times more likely to relapse with TB than those who only have TB.
- People living with HIV who contract a new tubercular infection can develop a severe illness very quickly.
- A person with HIV is more likely to develop tuberculosis and experience more severe symptoms than someone with a healthy immune system.
- Treatment for tuberculosis in a person with HIV can be complicated, but a doctor can create a comprehensive treatment plan that addresses both issues.
Summary
- Tuberculosis is a bacterial infection that most commonly affects the lungs, but it can also affect the kidneys, spine, brain, and other organs.
- Infection with the tuberculosis bacterium is not the same as active tuberculosis disease.
- Tuberculosis has three stages: exposure, latent disease, and active disease.
- The disease can be diagnosed with either a tuberculosis skin test or a tuberculosis blood test.
- Treatment must be carried out exactly as prescribed to cure the disease and prevent its spread to others.
References
- Hamada, Y., Getahun, H., Tadesse, B. T., & Ford, N. (2021, Aug). HIV-associated tuberculosis. International journal of STD & AIDS, 32(9), 780-790. DOI:10.1177/0956462421992257
- Suarez, I., Funger, S. M., Kroger, S., Rademacher, J., Fatkenheuer, G., & Rybniker, J. (2019). The Diagnosis and Treatment of Tuberculosis. Deutsches Arzteblatt international, 116, 729–735. DOI:10.3238/arztebl.2019.0729
- Christof, C., Nussbaumer-Streit, B., & Gartlehner, G. (2020). WHO guidelines on tuberculosis infection prevention and control. Gesundheitswesen, 82(11), 885-889. DOI.org/10.1055/a-1241-4321
- Sterling, T. R., Njie, G., Zenner, D., Cohn, D. L., Reves, R., Ahmed, A., & Belknap, R. (2020, Feb 14). Guidelines for the treatment of latent tuberculosis infection: recommendations from the National Tuberculosis Controllers Association and CDC, 2020. MMWR Recomm Rep, 69(1), 1-11. DOI: 10.15585/mmwr.rr6901a1
- Sharma, D., & Sarkar, D. (2018, Feb). Pathophysiology of Tuberculosis: An Update Review. PharmaTutor, 6(2), 15-21. https://doi.org/10.29161/PT.v6.i2.2018.15
- Park, K. (2017, Jan). PREVENTIVE AND SOCIAL MEDICINE (24 ed., pp. 185-211). Banarsidas Bhanot Publishers.