Introduction
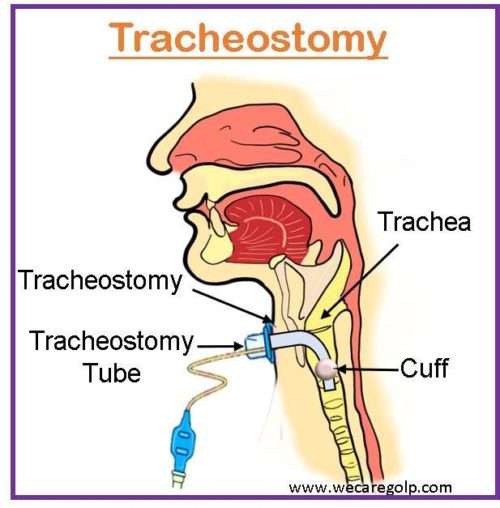
A tracheostomy is a surgically created opening in front of the neck (anterior trachea) to breathe effectively and to allow the air to flow to the lungs. The procedure to make an incision into the trachea is called tracheotomy, and the opening itself is called a tracheostomy (also called a stoma). However, the terms (tracheotomy and tracheostomy) are often used interchangeably.
- It is a life-saving procedure, which is done in critical conditions, such as a severe lung disorder, neurological problem, or infection and often combined with mechanical ventilation to assist in breathing.
- It can be done according to the need of the patients and in emergencies.
- It might be permanent or temporary depending on the indication and patient’s condition.
- Percutaneous dilatational tracheostomy (PDT) is an advanced, minimally invasive approach performed in the intensive care unit at the bedside and is quicker and less expensive.
Anatomy and Physiology of the Trachea
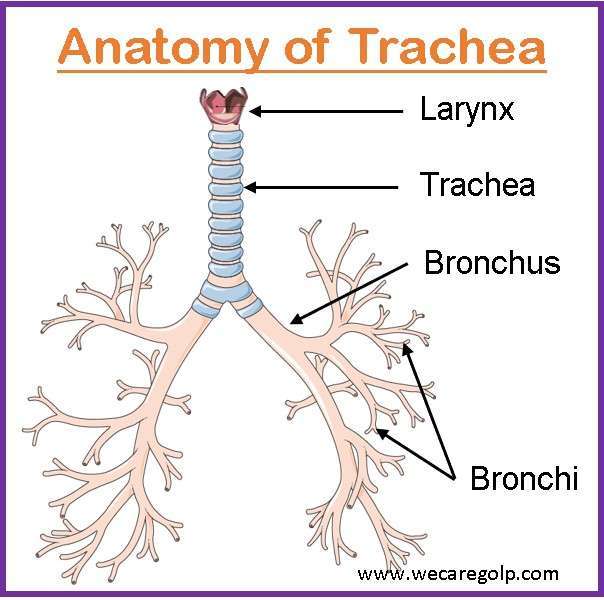
- The trachea is a cartilaginous tube with 15-20 C-shaped cartilaginous rings that extend from the larynx and branch to the two primary bronchi.
- It is 10-11 cm in length and about 1.5-2 cm in inner diameter, and wider in males than in females.
- It starts at the level of the sixth cervical vertebra(C6) and ends at the level of the fourth thoracic vertebra(T4).
- The core functions of the trachea are to allow air to flow into the lungs, mucociliary clearance, and humidification and warming of the air.
Purposes of Tracheostomy
- To maintain a patent airway and provide an alternative pathway for breathing
- TO bypass an upper airway obstruction
- To improve the alveolar ventilation
- To protect the airway
- To remove tracheobronchial secretions
Indications of Tracheostomy
Emergency tracheostomy
It is commonly performed in acute upper airway obstructions such as
- Acute upper respiratory tract obstruction with failed endotracheal intubation due to foreign body, angioedema, infection, or anaphylaxis, etc.
- Post cricothyrotomy
- Laryngeal trauma
- LeFort III fracture
- Epiglottitis
- Inhalation injury to the airway
Elective tracheostomy
It is commonly performed in chronic conditions such as
- Prolonged ventilator dependency
- Prophylactic tracheostomy before head and neck cancer treatment
- Chronic aspiration
- Neuromuscular disease (Amyotrophic lateral sclerosis)
- Subglottic stenosis
- Congenital anomaly of the airway
Contraindications of Tracheostomy
Absolute contraindications
There are only a few absolute contraindications.
- Cellulitis of the anterior neck
- Absence of a cervical trachea due to prior resection
- Uncorrectable bleeding diathesis
Relative contraindications
It includes hemodynamic instability and severe hypoxia (e.g., positive end-expiratory pressure (PEEP) > 12 cm H2O and a fraction of inspired oxygen > 0.6). If there is neck distortion due to hematoma, tumor, thyromegaly, and scarring from previous neck surgery, it may be contraindicated.
Some relative contraindicated conditions are
- Tracheomalacia
- Cartilage abnormalities
- Obese and/or short neck
- Cervical fusion
- Rheumatoid arthritis
- Cervical spine instability
- PDT is contraindicated in pediatrics, below 16 years old due to immature trachea
- Neck infection, burn, trauma
Types of Tracheostomy Tube
- Tubes vary in size, length, and diameter.
- There are three parts of the tube
- Outer cannula,
- Obturator, and
- Inner cannula.
- The tracheostomy tube should be selected according to
- The outer diameter,
- The inner diameter, and
- The length of the tube.
Single and Dual cannula tracheostomy tubes

- When an adult needs a temporary tracheostomy due to a serious disease, a non-fenestrated single cannula tube with an air-filled cuff is typically used.
- Dual cannula tubes are used for patients who need tracheostomy after discharge from the Critical Care Unit.
Fenestrated tracheostomy tubes
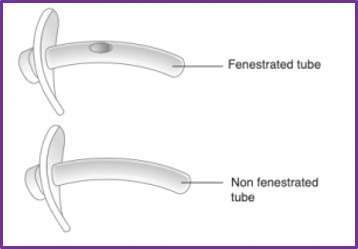
- In contrast to non-fenestrated tubes, fenestrated tubes make it easier for patients to speak and require less exertion to breathe as they are being weaned from ventilation.
Cuffed tracheostomy tubes
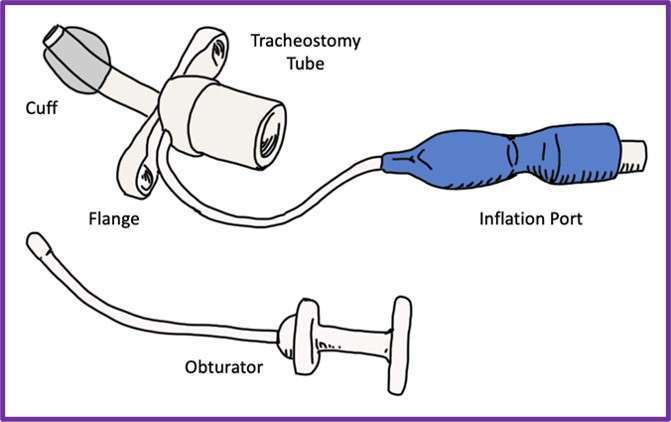
- Cuffed tracheostomy tubes have a soft balloon at the end of the tube that inflates to seal the airway.
- Cuffed tubes are necessary when positive pressure ventilation is required and to reduce the risk of aspiration of oral or gastric secretions.
- It is advised to regularly monitor the cuff pressure throughout each shift (8–12 hours per shift) and to keep it between 25–34 cmH2O.
Uncuffed tracheostomy tubes

- Uncuffed tubes are used in longer-term patients who require continuing suction to remove secretions since they cannot be inflated inside the trachea.
- Since the gas will escape above the tube, these tubes will not allow sustained effective positive pressure ventilation.
- The patients should have an effective cough and gag reflex to protect them from aspiration, as there is no cough to ‘protect’ the airway.
- These tubes reduce the risk of tracheal damage caused by inflation of the cuff and may aid swallowing and communication using a speaking valve.
Procedure
Before the Procedure
- A tracheostomy is most commonly performed in an operating room with general anesthesia or a hospital room.
- The patient should be kept in the NPO.
- All the required equipment will be prepared.
- A video bronchoscopy is done to find the appropriate place to insert the tube.
- General anesthesia/incision procedure should start only after the entire surgical set is prepared, the surgeon, assistant, and personnel are cleaned and draped, and there is less time between skin-to-skin.
During the Procedure
In the operating room, there should always be a variety of cuffed, non-fenestrated sets of tracheostomy tubes available for use.
Open surgical tracheostomy (OST)
- It can be performed in an operating room or a hospital room.
- The muscles around the lower region of the front of the neck are carefully pulled back, a horizontal incision is made, and a little bit of the thyroid gland is cut, exposing the trachea.
- At a specific spot on the windpipe near the base of the neck, a hole will be created.
Percutaneous dilatational tracheostomy (PDT)
- PDT is a minimally invasive procedure.
- A small incision is made near the base of the front of the neck during a standard medical procedure.
- A special lens is fed through the mouth to guide a needle into the windpipe to create a hole, then expands to the appropriate size for the tube.
- For both procedures, a tube is inserted into the hole.
- If the patient needs a machine to help breathe, the surgeon may connect the tube to a ventilator.
- The face plate of the tube is fastened to the neck using a neck strap, and the face plate can be stitched to the skin of the neck with temporary sutures.
After the Procedure
After the tracheostomy is created, tracheostomy care should be done to prevent infection and reduce the risk of complications.
- In the beginning, intravenous (IV) fluids are given to meet the nutritional needs, then nasogastric or orogastric feeding can be done.
- Later, collaboration with a speech therapist can help to regain muscle strength and coordinate swallowing.
- A humidifier or vaporizer can be used to moisten the air and help minimize the irritation, coughing, and secretions due to dry air.
- A speech therapist or a nurse trained in tracheostomy care can help to learn to speak with a tube in place.
Post Tracheostomy Care
- Suction the tube to clear the secretions from the airway.
- Clean the suction catheter to prevent infection.
- Replace the inner cannula to keep secretions from blocking the tube.
- Clean the skin around the tracheostomy to prevent irritation.
- Moisturize the air to loosen secretions.
- Apply a sterile dressing, change the tracheostomy ties, and check for tightness.
Risks/Complications of Tracheostomy
There are immediate and late complications of tracheostomy. It is more likely to cause problems for babies, smokers, immunocompromised patients, diabetes, and the elderly.
Immediate complications
- Bleeding
- Damage to the trachea, thyroid gland, and esophagus
- Misplacement or displacement of the tracheostomy tube
- Subcutaneous emphysema on the neck
- Pneumothorax that results in discomfort, breathing issues, or lung collapse
- A neck hematoma may develop and compress the trachea, impairing breathing
- Pneumomediastinum
Late complications
The longer a tracheostomy is in place, the higher the likelihood of long-term difficulties. These problems include
- The tracheostomy tube obstruction
- Displacement of the tube from the trachea
- Damage, scarring, or narrowing of the trachea
- Tracheoesophageal fistula, which increases the risk of fluids or food entering the lungs
- Tracheoinnominate fistula, which may cause potentially fatal bleeding
- Infection surrounding the tracheostomy or pneumonia or tracheobronchitis of the lungs or bronchial tubes
- Tracheomalacia
Summary
- A tracheostomy is an artificial airway made after an indwelling tube is inserted through a surgically made hole into the trachea through the neck.
- It is a life-saving procedure performed to bypass an upper airway obstruction, maintain a patent airway, protect the airway, remove tracheobronchial secretions, and improve alveolar ventilation.
- The trachea is a cartilaginous tube that extends from the larynx and branches to the two primary bronchi.
- Tracheostomy tubes vary in size, length, and diameter and include single and dual cannula, fenestrated, cuffed, and uncuffed tracheostomy tubes.
- The procedure is commonly performed in an operating room with general anesthesia or a hospital room.
References
- Liu, B., Wang, G., Yu, W., Zhang, Y., & Wang, J. (2022). Comparison of early and late tracheostomy for mechanically ventilated patients: A systematic review and meta-analysis. BMC Surgery, 22(1), 50. https://doi.org/10.1186/s12893-023-01960-5
- Cheung, N. H., & Napolitano, L. M. (2014). Tracheostomy: Epidemiology, Indications, Timing, Technique, and Outcomes. Respiratory Care, 59(6), 895-919. doi: 10.4187/respcare.02971
- Frazier, R. (2014). Tracheostomy care. Nursing Critical Care, 9(6), 36-43. doi: 10.1097/01.CCN.0000458883.13936.85
- National Center for Biotechnology Information. (2022). Tracheostomy. StatPearls Publishing. Retrieved on 2023, May 5 from https://www.ncbi.nlm.nih.gov/books/NBK559124/
- Johns Hopkins Medicine. (n.d.). Tracheostomy. Retrieved on 2023, May 5 from https://www.hopkinsmedicine.org/health/treatment-tests-and-therapies/tracheostomy
- NHS. (2022, Feb 24). Tracheostomy. Retrieved on 2023, May 5 from https://www.nhs.uk/conditions/tracheostomy/
- American Cancer Society. (n.d.). Tracheostomy guide. Retrieved on 2023, May 5 from https://www.cancer.org/treatment/treatments-and-side-effects/treatment-types/surgery/tracheostomy-guide.html
- St George’s Healthcare NHS Foundation Trust. (n.d.). Tracheostomy tubes. Retrieved on 2023, May 5 from https://www.stgeorges.nhs.uk/gps-and-clinicians/clinical-resources/tracheostomy-guidelines/tracheostomy-tubes/
- Memorial Sloan Kettering Cancer Center. (n.d.). Caring for Your Tracheostomy. Retrieved on 2023, May 5 from https://www.mskcc.org/cancer-care/patient-education/caring-your-tracheostomy
- Kindred Healthcare. (n.d.). Tracheostomy Care. Retrieved on 2023, May 5 from https://www.kindredhospitals.com/our-services/ltac/conditions/tracheostomy-care
- University of Iowa Health Care. (n.d.). Tracheotomy/Tracheostomy. Retrieved on 2023, May 5 from https://medicine.uiowa.edu/iowaprotocols/tracheotomy-tracheostomy
- Wayne, G. (2021, Dec). Tracheostomy. Nurselabs. Retrieved on 2023, May 5 from https://nurseslabs.com/tracheostomy-nursing-management/
- Better Health Channel. (2021, November). Tracheostomy. Retrieved on 2023, May 5 from https://www.betterhealth.vic.gov.au/health/conditionsandtreatments/tracheostomy