Introduction
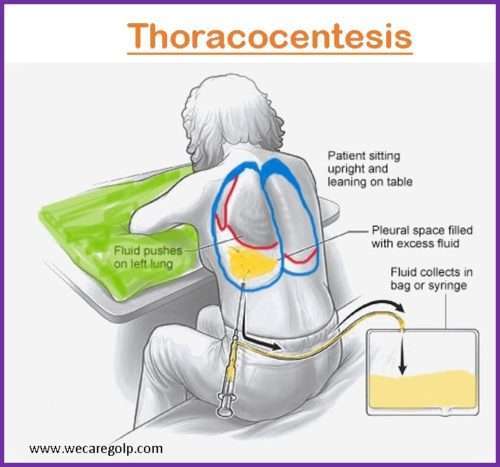
Thoracocentesis is a surgical procedure that removes excess pleural fluid or air from the area between the lung and the chest wall. The procedure is also known as “pleural fluid aspiration,” “pleural tap,” “pleurocentesis,” and “thoracentesis.”
- The pleural space is the area where the fluid gathers. It develops between the visceral pleura (the serous membrane that covers each lung) and the parietal pleura (the serous membrane that covers the chest wall).
- The pleural gap normally contains relatively little fluid, which serves to lubricate the two pleural surfaces so they can easily move over one other during respiration.
- Serous fluid should not exceed 20 mL in the pleural cavity.
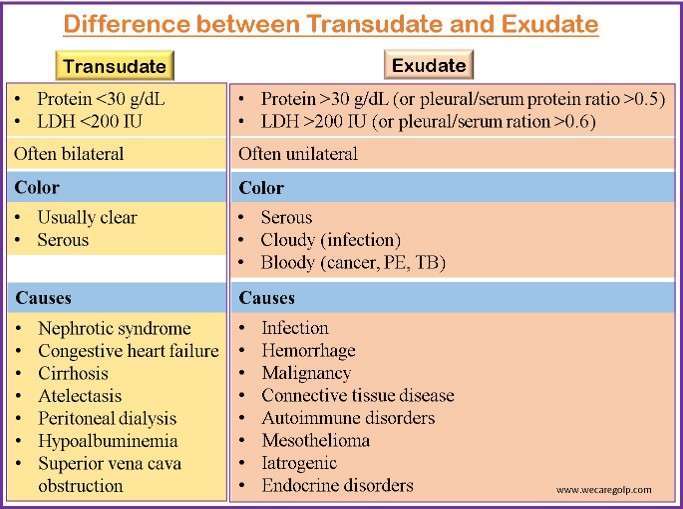
- The improper production or reabsorption of pleural fluid causes pleural effusion. Pleural fluid is categorized as either an exudate or a transudate based on specific features.
Indications of Thoracocentesis
Diagnostic
A diagnostic thoracocentesis involves the removal of a small sample of pleural fluid (approximately 2 ounces [60 mL]) to discover the etiology of pleural effusion and to assist clinicians in determining the appropriate treatment.
- For physical, biochemical, cytological & bacteriological study of pleural fluid to come to a definitive diagnosis
- The reason for excess fluid is uncertain
Therapeutic
A therapeutic thoracentesis is performed to remove a higher volume of pleural fluid (approximately 20 ounces [600 mL] to 40 ounces [1200 mL]) to ease symptoms such as shortness of breath.
The purposes of therapeutic thoracocentesis are
- To ease respiratory distress
- To avoid the risk of massive and rapid fluid collection
- To treat suspected secondary infection of effusion
- To provide symptomatic relief with large pleural effusion
Contraindications of Thoracocentesis
- There are no absolute contraindications for thoracocentesis.
- Relative contraindications may include
- Anticoagulation or uncorrected bleeding diathesis
- Chest wall cellulitis or any active skin infection at the site of needle insertion
- Platelet count less than 25,000/mm3
- Atelectasis
- Bullous emphysema
- Single-functioning lung
- Ventilation with positive end-expiratory pressure support
- Any condition that prevents the patient from being positioned safely
- Circumstances in which the risks of the surgery outweigh the benefits
Procedure
Before Procedure
- Describe the procedure’s goal, risks and advantages, and measures to take while getting the patient’s consent. An explanation gives the patient a better understanding of the procedure, aids in coping, and gives them a chance to ask questions and express their anxiety verbally.
- Ask the patient about any health issues such as
- Breathing issues
- Coughing or hiccups
- Heart problems
- Smoking
- Possible exposure to tuberculosis (TB).
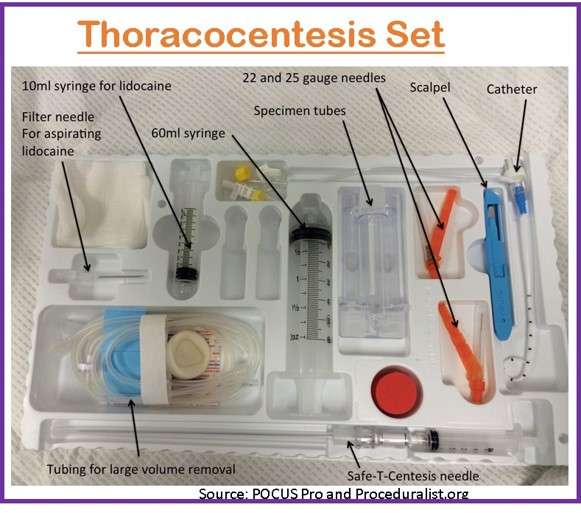
- Gather all necessary equipment.
- Sterile gloves
- Sterile gauze
- Waterproof transparent dressing pack
- Skin disinfectant > 0.5% chlorhexidine with 70% alcohol (if a history of chlorhexidine sensitivity, use povidone-iodine in alcohol).
- Local anesthetic- Lignocaine 1% (50 mg/ 5 ml) or 2% (100 mg/ 5 ml)
- 5mL, 20mL and 50mL syringes
- Thoracocentesis catheterization kit
- Assess platelet count and/or the existence of coagulopathy. If the platelet count is below 25,000 or there is known coagulopathy, it is determined whether platelet transfusion or other action is required to avoid complications such as bleeding during the surgery.
- Assist the patient in maintaining their upright, cardiac position throughout the operation. The upright position helps to remove fluid that typically accumulates at the base of the chest and makes the diaphragm more dependent.
- To lessen the likelihood of injury, instruct the patient not to cough, breathe heavily, or move during the procedure.
- Inform the patient that a local anesthetic will be used to alleviate any pain that occurs during the procedure.
- To prevent infection and adhere to the aseptic technique, clean the patient’s skin with an antiseptic solution.
During Procedure
- Put the patient on continuous cardiac and pulse oximetry monitoring.
- Oxygen therapy should be given during the procedure unless contraindicated.
- The area of intervention is marked with an ultrasound.
- Prepare the area using antiseptic (> 0.5% chlorhexidine with 70% alcohol).
- Make sure that the local anesthesia (1% lignocaine) infiltrates from subcutaneous tissue to the pleura.
- Pay close attention to the patient’s breathing pattern and respiration rate to obtain baseline data to evaluate the patient’s comfort during the process.
- Monitor the patient’s vital signs, such as their blood pressure and pulse, to avoid complications during the procedure, notably hypovolemic shock.
- Assess the state of consciousness of the patient and provide emotional support to soothe the patient’s concern.
- Maintain saturation level to avoid hypoxia
- If the patient experiences any changes the doctor can decide whether to keep forward with the procedure or stop it altogether.
- Pleural fluid can be drained a maximum of 1000 ml per day to avoid the risk of re-expansion pulmonary oedema.
- If a second tap is needed the next day, the pleural aspiration catheter can be left in place after the procedure. However, to avoid pneumothorax, an adequate seal is necessary to avoid pneumothorax.
After Procedure
- To determine the state of the lungs before and after the procedure, get a chest x-ray to assess the fluid level.
- To prevent over intake of fluid into the specimen bottle during specimen handling, just add the necessary amount of pleural fluid to the tubes.
- Check that each bottle is properly labeled with the patient’s complete name, date of birth, and/or medical record number before sending it to the lab for testing to avoid giving the patient inaccurate findings.
- Document the procedure, patient’s response, characteristics of fluid and amount, and patient response to follow-up to develop a further treatment for the patient.
- Provide post-procedural analgesics as needed to prevent the patient from pain related to the incision site.
- To avoid complications like dyspnea, the patient should rest in bed for about 2 hours after the procedure to reduce activity.
- Blood pressure and breathing will be monitored for several hours to ensure there are no issues.
- The patient needs urgent medical help if there are concerns like
- Bleeding from the procedure site
- Signs of infection
- Breathing difficulties
- Remove the dressing/bandage another day, or replace it if it becomes soiled or moist to avoid infection.
- Reintroduce the patient’s regular diet to aid wound healing.
Complications of Thoracocentesis
- Laceration of intercostals vessels
- Pneumothorax
- Mediastinal shift
- Re-expansion pulmonary edema (RPE)
- Wound bleeding and infection
- Pain or chest wall numbness
- Subcutaneous emphysema
- May require reattempt due to failure
- Visceral injury (lung, diaphragm, liver, spleen, heart)
Precautions for Thoracocentesis
- Thoracocentesis is contraindicated in the patient who has a history of bleeding disorders or anticoagulant therapy.
- A strict sterile technique must be maintained.
- Avoid any movement that may interfere with the procedure.
- Avoid coughing, breathing deeply, or moving during the test to avoid injury to the lung.
- To avoid the intercostal blood vessels and nerves at the lower border of each rib, place the thoracentesis needle slightly and carefully above the top edge of the rib and not below it.
- Initiating Antimicrobial therapy before fluid aspiration for culture can make it difficult to isolate infecting organisms as there is a possibility of a decrease in the number of bacteria.
Interpretation of Thoracocentesis
- Transudate and exudate should be distinguished from the collected fluid.
- Increased hydrostatic forces are the source of a transudative effusion. The capillaries’ permeability to proteins is typical. Capillary permeability is increased or lymphatic blockage results in an exudative effusion.
Normal Results
- Negative pressure in the pleural cavity with less than 50 ml serous fluid
Abnormal Results
- The presence of bloody fluid signals a probable hemothorax, cancer, or traumatic tap.
- Milky fluid indicates chylothorax.
- Fluid with pus indicates empyema.
- Transudative effusion signifies heart failure, cirrhosis of the liver, or renal illness.
- Exudative effusion often suggests lymphatic drainage, infections, lung infarctions, and neoplasm.
- Positive cultures indicate infection.
- The presence of lymphocytes indicates TB, fungal or viral effusions.
- Pleural fluid glucose levels that are 30 to 40 mg/dl lower than blood glucose levels may indicate malignancy, bacterial infection, or metastases.
- Increased amylase indicates pleural effusions linked with pancreatitis.
Summary
- Thoracocentesis is a medical technique that includes removing fluid or air from the chest cavity with a needle and syringe.
- This procedure is often used to diagnose or treat problems such as pleural effusion, pneumothorax, or hemothorax.
- Before the procedure, the patient is positioned upright or slightly tilted, and the skin over the puncture site is cleaned and sterilized.
- A local anesthetic may be administered to numb the area around the puncture site. The physician will then insert a needle through the skin and into the chest cavity to remove the fluid or air.
- The collected sample is sent to a laboratory for analysis to determine the underlying cause of the buildup.
- Thoracocentesis is generally considered a safe procedure, but there are potential risks, such as infection, bleeding, or lung puncture.
- Patients should be closely monitored for any complications after the procedure.
References
- Mandal, G.N. (2019). A Textbook of Medical Surgical Nursing. Makalu Publication House
- Kalifatidis, A., et.al (2015). Thoracocentesis: from bench to bed. Journal Of Thoracic Disease, 7(l1), S1-S4. doi:10.3978/j.issn.2072-1439.2014.12.45
- Mittal, M.K., & Baren, J. (2009). Thoracocentesis. Comprehensive Pediatric Hospital Medicine, 1273-1275. https://doi.org/10.1016/B978-032303004-5.50214-3
- Cantey, E.P., Walter, J.M., Corbridge, T., Barsuk, J.H. (2016, Jul). Complications of thoracentesis: incidence, risk factors, and strategies for prevention. Curr Opin Pulm Med,22(4):378-85. DOI: 10.1097/MCP.0000000000000285
- Leo, F., & Makowska, M. (2018). Pleurapunktion – Schritt für Schritt [Thoracentesis – Step by Step]. Deutsche medizinische Wochenschrift, 143(16), 1186–1192. https://doi.org/10.1055/s-0044-102082
- Wiederhold, B.D, Amr, O., Modi, P., & et al.(2023). Thoracentesis. StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK441866/
- Jackson, K., and et.al. (2021). Complications after Thoracocentesis and Chest Drain Insertion: A Single Centre Study from the North East of England. Journal of Respiration,1(2):135-140. https://doi.org/10.3390/jor1020014