Introduction
Encephalitis is derived from the Greek word enkephalos meaning “brain” and itis meaning “inflammation”, which simply means the inflammation of the brain. It is an infectious condition (mostly viral) of the central nervous system (CNS) and can be life-threatening.
- Encephalitis is usually due to an autoimmune response or infective agent that produces alteration to various parts of the brain and spinal cord.
- The inflammation of the spinal cord is known as myelitis. Encephalomyelitis is the name given to the condition when it affects the brain as well as the spinal cord.
- Pathological changes in the gray and white matter of the brain and spinal cord can signalize encephalitis.
- In extreme cases, this inflammation can result in brain damage, stroke, or even death.
Incidence
- Each year, encephalitis affects 10–15 per 100,000 persons, and more than 250,000 patients have been identified in the U.S. in only the past ten years.
- Anyone can be affected by the illness. However, younger people are more frequently affected.
- Even though both sexes are impacted, most studies have revealed a small male predominance.
- Many encephalitis outbreaks, including West Nile and St. Louis encephalitis, have occurred in the United States in recent years.
- Japanese encephalitis virus (JEV) is the most significant cause of viral encephalitis in Asia. International travelers are most at risk for both tick-borne and Japanese encephalitis.
- Japanese encephalitis is mostly found in China, Japan, Nepal, and Korea and is transmitted by mosquitoes.
- New encephalitis-causing infections have emerged as a result of changing ecology.
Types of Encephalitis
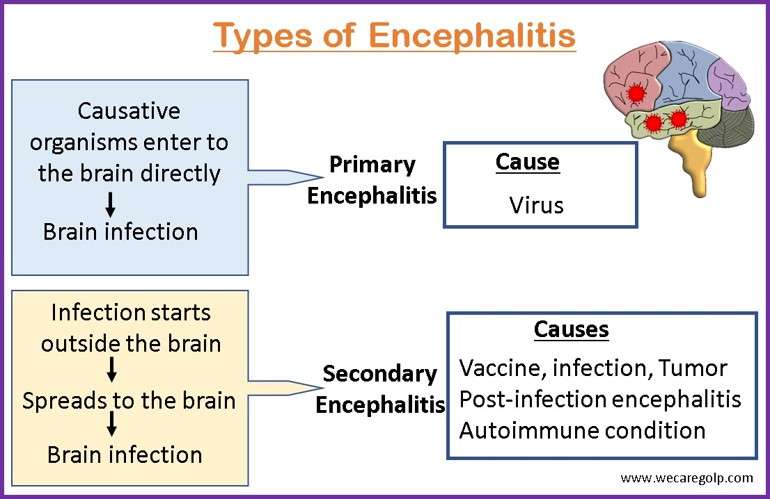
Primary Encephalitis
When a virus directly infects the brain and spinal cord, this is called primary encephalitis.
Some viruses that can cause infectious encephalitis are:
- Enterovirus
- Toxoplasmosis
- Cold sores caused by Herpes Simplex Virus (HSV)
- Viruses transmitted by mosquito bites (including Murray Valley encephalitis, Japanese encephalitis, and equine encephalitis)
- Chickenpox
- Measles
- Mumps
- Rubella (german measles)
Secondary Encephalitis
When an infection begins elsewhere in the body and then spreads to the brain, this condition is known as secondary encephalitis.
- If your immune system starts attacking your brain cells in response to something in your body (like an infection, vaccine, or tumor) secondary encephalitis can occur.
- It often referred to as post-infection encephalitis frequently develops two to three weeks after the first infection.
- It can also occur if there is an autoimmune condition.
Causes of Encephalitis
Viruses
A viral infection is usually the cause of infectious encephalitis. It accounts for approximately 70% of cases.
- The most common encephalitis-causing viruses are
- Herpes simplex virus (HSV) types 1 and 2 (cause cold sores)
- Varicella zoster virus
- Enteroviruses
- Tick-borne viruses
- Other viruses-causing cold sores
- Mumps
- Measles
- HIV
- Chickenpox
- Arboviruses
- West Nile virus
- Japanese encephalitis virus
- La Crosse encephalitis virus
- St. Louis encephalitis virus
- Equine encephalitis virus
- Powassan virus
- Zika virus
- Chikungunya virus
Other organisms (in rare cases)
- Bacteria
- Fungi
- Parasites
Post-vaccination (rare cases)
- MMR (Measles, Mumps, Rubella)
- Rabies
- Pertussis
- Influenza
Autoimmune encephalitis
- When a person’s own antibodies or immune cells assault the brain, autoimmune encephalitis results.
- The type of autoimmune encephalitis is determined by antibodies, which may target specific proteins or receptors in the brain like
- Voltage-gated potassium channel (VGKC) brain protein complex: Leucine-rich, glioma-inactivated 1 (LGI1) and Contactin-associated protein-like 2 (CASPR2)
- N-methyl-D-aspartate (NMDA) brain receptors
- Gamma-aminobutyric acid receptor A (GABA-A)
- Gamma-aminobutyric acid receptor B (GABA-B)
- Glutamic acid decarboxylase (GAD)
- Amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid receptor (AMPAR)
- An infection can trigger post-infectious encephalitis which is called acute disseminated encephalomyelitis (ADEM).
- Occasionally, a tumor (benign or cancerous) can cause autoimmune encephalitis.
Mode of Transmission
Some types of encephalitis can transmit from human to human through
- Feces
- Nasal discharge
- Saliva
- Respiratory secretion (kissing, coughing, sharing utensils, etc.)
Risk Factors
Factors that may increase the risk include:
- Age: In specific age groups, some encephalitis forms are more prevalent or more severe. In general, the risk of most viral encephalitis is higher in young children and older individuals.
- Weakened immune system: Individuals who have HIV/AIDS, take immunosuppressive medications or have another condition that compromises immunity are more likely to get encephalitis.
- Geographical regions: Encephalitis-causing mosquitos are found in specific areas.
- Season of the year: Some locations are prone to mosquito- or tick-borne diseases.
Signs and Symptoms of Encephalitis
Prodromal Signs and Symptoms
Headache
- Often severe headache
- May feel different than a normal headache
- Due to brain inflammation and swelling, pain receptor is activated which leads to headache
Myalgias
- Muscles aches and pain
Malaise
- Feeling generally unwell
- Due to the state of inflammation/infection
Severe Symptoms
After prodromal symptoms, the patient becomes more acutely ill within hours to days.
Fever
- Temperature >38 C (>100 F)
- High fever
- Often occurs suddenly
Altered mental status
- This may manifest as difficulty in concentration, decreased alertness/consciousness, confusion (altered sensorium)
- Due to brain inflammation and swelling leading to a reduction in cognitive ability
Cognitive disturbances
- Hallucinations
- Changes in temperament, behavior, mood
- Disorientation
Cognitive decline
- Memory deficits (Herpes Simplex Virus attacks temporal lobes which is the center for memory functioning)
Seizures and Coma
- It is due to brain swelling and increased Intracranial Pressure (ICP)
Focal Neurological Deficits
- Inflamed tissue in particular regions of the brain can cause specific functional, and neurological deficits
- Specific brain anatomic site is affected
- For example, decreased ability to speak, use one limb, etc.
Others
- Some infective etiologies for encephalitis can cause skin manifestations.
- Vesicles in Herpes Simplex Virus
- Lymphadenopathy (Swollen/ Tender lymph nodes), Splenomegaly (enlarged spleen) due to Epstein Barr Virus
Pathophysiology of Encephalitis
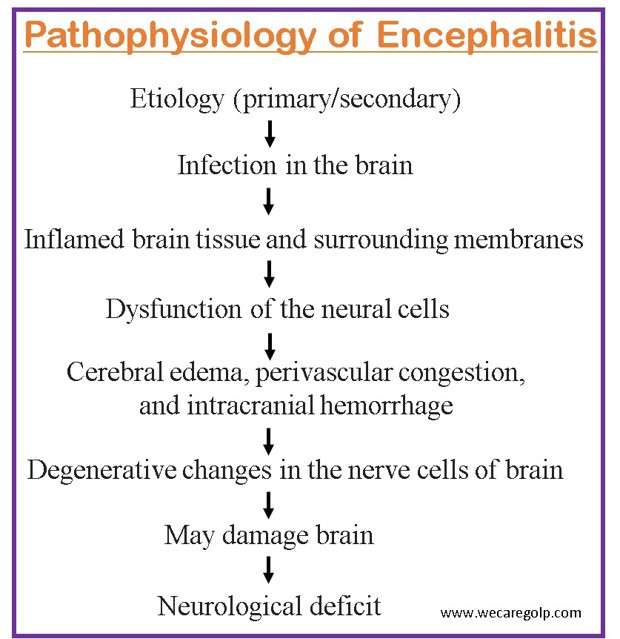
- Viruses replicate outside the central nervous system (CNS) when they enter the host.
- Most viruses spread to the brain and spinal cord through the bloodstream (hematogenous).
- They travel retrogradely from nerve endings to the CNS.
- In the case of arbovirus infection, the virus invades dendrite cells, replicates within them, and macrophages in lymph nodes, resulting in spread to the central nervous system.
- The virus and the inflammatory response of the host disrupt the function of neural cells once they are in the brain resulting in cerebral edema, perivascular congestion, intracranial hemorrhage, and a diffuse inflammatory response that disproportionately affects gray matter over white matter.
- There are degenerative changes in the nerve cells of the brain.
- These changes cause neurological deficits.
- Sometimes, meninges may also involve causing meningoencephalitis.
- Multiple focal areas of perivenous demyelination and the absence of virus in the brain are hallmarks of acute disseminated encephalomyelitis.
- Perivenous demyelination in multiple foci and the absence of a virus in the brain are the main characteristics of acute disseminated encephalomyelitis (ADEM).
- Calcification frequently occurs following arbovirus encephalitis, particularly in children.
- Herpes simplex typically results in focal necrotic lesions characterized by distinct intranuclear inclusions.
Diagnosis
Medical history
- Vaccinations
- Respiratory illness
- Recent tick and insect bite
- Exposure to animal
- Recently visited areas
- Pre-existing medical conditions and medications
- Contact with ill persons
Physical examination
- Motor and sensory function
- Nerve function
- Hearing and speech
- Vision
- Coordination and balance
- Mental status
- Changes in mood or behavior
Neuroimaging
- Magnetic resonance imaging (MRI) and computed tomography (CT) scan
- MRI and CT scans can help detect whether it is encephalitis or other brain abnormalities like stroke, brain aneurysm, or brain tumor.
- It reveals the changes in the brain structure (inflammation, internal bleeding).
- The affected parts of the brain can help determine the disease-causing virus type.
- Lumbar puncture (spinal tap)
- A lumbar puncture is a procedure to collect cerebrospinal fluid (CSF) to check for signs of infection in the brain or spinal cord.
- In arbovirus encephalitis, specific IgM in CSF and a fourfold change in specific IgG antibodies may detect.
- Electroencephalogram (EEG)
- Electrodes are placed in the brain to determine the electrical activity of the brain, which looks for seizures or specific patterns of electrical activity in the brain
- EEG shows slow brain wave complexes in encephalitis
Blood, urine, and stool tests
It is done to find out the responsible causes of infection.
- Causative organisms
- The presence of antibodies
- Foreign proteins
Additional tests
- Sputum culture tests to see if there is the presence of infections or not.
- In rare cases, a biopsy of affected brain tissue may be performed to allow for examination under a microscope.
- Intracranial pressure monitoring (ICP) to monitor brain swelling.
Treatment of Encephalitis
Supportive Management
- The goals of treatment are to provide supportive care (rest, nutrition, fluids) to help the body fight against the infection and to relieve symptoms.
- Reorientation and emotional support for confused or delirious people may be helpful.
- If brain function is severely affected, interventions like physical therapy and speech therapy may be needed after the illness is controlled.
- Treatment is symptomatic since no effective drugs are known in encephalitis for viral infections.
Pharmacological Management
- Antiviral medications, such as acyclovir (Zovirax) and foscarnet (Foscavir): to treat herpes encephalitis or other severe viral infections (however, no specific antiviral drugs are available to fight against encephalitis)
- Antibiotics or antifungal medicine if there is a bacterial or fungal infection
- Anti-seizure medicine such as phenytoin helps to prevent seizures
- Sedatives to treat irritability or restlessness
- High-dose IV corticosteroids in case of ADEM (Acute Demyelinating Encephalomyelitis) to reduce brain swelling.
- Mycoplasma pneumonia may be treated with doxycycline, erythromycin, azithromycin, clarithromycin
- Acetaminophen for fever and headache
- Immunotherapy: such as steroids, and intravenous immunoglobulin (IVIg) can use to maintain the immune system.
- Plasmapheresis is a procedure for the autoimmune antibodies from the plasma in case of autoimmune encephalitis.
- Immunosuppressant drugs can also be used to treat autoimmune encephalitis.
Medical Management
- Tracheostomy (artificial respiration) is needed if respiratory difficulties occur.
- A breathing tube, urinary catheter, or feeding tube may require if the patient is unconscious.
Complications of Encephalitis
- Permanent brain damage may occur in severe cases. It can affect:
- Hearing
- Memory
- Sensation
- Speech
- Muscle control
- Vision
- Learning difficulties
- Personality and behavioral changes
- Seizures or fits- (epilepsy)
- Persistent physical weakness
- Problems with attention, concentrating, planning, and problem-solving
- Breathing difficulties
- Coma
- Death
Prevention of Encephalitis
Although encephalitis is not always preventable, the risk can be lowered with the following measures.
- Controlling mosquitoes may reduce the chance of some infections that can lead to encephalitis.
- Avoid mosquito bites by
- Limit outdoor activities at night,
- Wearing long sleeves and pants when outdoors
- Using insect repellents
- Using screens on windows and doors
- Use proper hygiene and hand-washing to help prevent the spread of viruses and bacteria.
- Avoid sharing glasses, food, utensils, and other items with someone who may have an infection.
Vaccination
- When traveling to areas that are known to have viruses that can cause encephalitis, it is important to keep your vaccinations up to date.
- Ensure that your children receive vaccinations against all encephalitis-causing viruses.
- The available vaccines are:
- Rabies vaccine
- Japanese encephalitis (JE) vaccine
- Measles, Mumps, Rubella (MMR) vaccine
- Herpes zoster vaccine
- Chickenpox vaccine
Prognosis
- The severity of the inflammation determines the prognosis.
- The symptoms go away in a few days in mild cases. In severe conditions, it might require weeks or months to improve.
- It can occasionally result in permanent brain damage or death. The mortality rate is only 5%
- In two-thirds of cases, patients recover without sequelae before discharge from the hospital.
- Some patients may have neurologic complications like spasticity, cognitive impairment, weakness, ataxia, and seizure.
Summary
- Encephalitis is an inflammation of the brain parenchyma.
- While the illness can affect anyone, younger people are more frequently affected.
- There are mainly two types of encephalitis. Primary encephalitis occurs if a virus infects the brain. Secondary encephalitis occurs if the immune system reacts to something in the body, such as an infection, vaccine, or cancer.
- A viral infection is a typical cause of encephalitis. However, other organisms like bacteria, fungi, and parasites can also be the reason for this disease.
- It can be mild or severe. Severe cases need immediate treatment.
- Symptoms of severe cases include Severe headache, sudden fever, drowsiness, confusion, and seizures. In case the condition of the patient is critical, it may require admission to the hospital.
- Treatments include anti-inflammatory and anti-infective medications administered orally and intravenously (IV).
- Patients who have trouble breathing may require artificial respiration.
- Once the illness is under control, some people may require physical, speech, or occupational therapy.
References
- Mandal, G.N. (2019). A Textbook of Medical Surgical Nursing. Makalu Publication House
- K.C, V. (2019). Manual of Pathophysiology. Arcadia Publishing House Pvt. Ltd.
- Granerod, J., & Crowcroft, N. S. (2007). The epidemiology of acute encephalitis. Neuropsychological rehabilitation, 17(4-5), 406–428. https://doi.org/10.1080/09602010600989620
- Chaudhuri, A., & Kennedy, P.G.E. (2002). Diagnosis and treatment of viral encephalitis. Postgraduate Medical Journal, 78 (924), 575-583. DOI: 10.1136/pmj.78.924.575
- NHS. (2019, Dec 3). Encephalitis. Retrieved on 2023, Mar 2 from https://www.nhs.uk/conditions/encephalitis/
- eaHHealth Direct. (2022, Sep). Encephalitis. Retrieved on 2023, Mar 3 from https://www.healthdirect.gov.au/encephalitis#causes
- World Health Organization. (2019, May 9). Japanese encephalitis. Retrieved on 2023, Mar 3 from https://www.who.int/news-room/fact-sheets/detail/japanese-encephalitis
- John Hopkins Medicine. Encephalitis. Retrieved on 2023, Mar 2 from https://www.hopkinsmedicine.org/health/conditions-and-diseases/encephalitis
- Britannica. (2023, Feb 2). Encephalitis. Retrieved on 2023, Mar 2 from https://www.britannica.com/science/encephalitis
- Alam, A.M., Easton, A., Nicholson, T.R., Irani, S.R., Davies, N.WS., Solomon, T., Michael, B.D. (2022, Jun 23). Encephalitis: diagnosis, management and recent advances in the field of encephalitides. Postgraduate Medical Journal. doi: 10.1136/postgradmedj-2022-141812