Introduction
The anatomy of the kidney consists of gross and microscopic structures. The kidney is a vital organ in the human body responsible for many functions, including regulating salt and electrolyte, maintaining fluid balance, filtering waste products from the blood, and producing urine. The average adult renal blood flow is 1,000 to 1,400 ml per minute (1500 to 1700 liters/day). This corresponds to 20 to 25% of cardiac output for an organ system that accounts for only 0.5% of body weight. The crucial role of the kidney is to maintain overall health and homeostasis in the body.
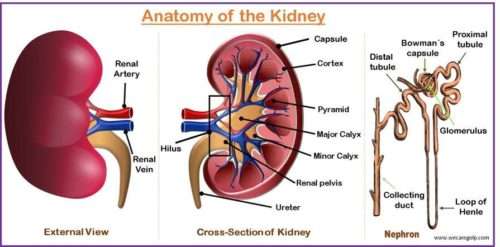
- The kidneys are two bean-shaped, reddish-brown excretory organs, which are also the principal organ of the urinary system.
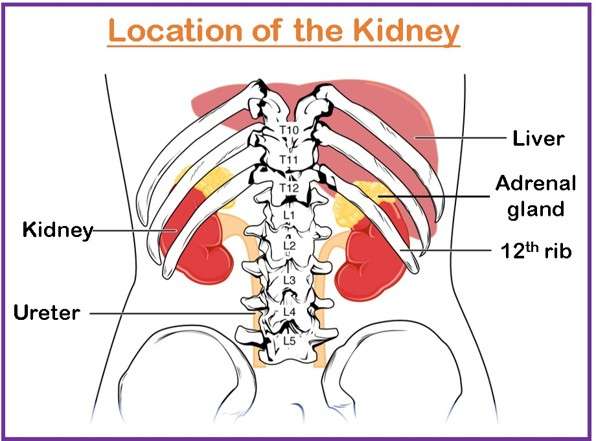
- They are situated on the posterior abdominal wall, retroperitoneally, one on each side of the vertebral column at the level of twelve thoracic (T12) vertebrae to third lumbar (L3) vertebrae.
- Since the massive liver occupies the right hypochondrium, the left kidney is slightly at a higher level than the right one.
Shape and Size of the Kidney
- Each kidney is approximately a size of a fist and weighs from 150-200 g in males and about 120 to 135 g in females according to the body size.
- It measures about 10-12 cm in length, 5-7 cm in width, and 3-5cm in thickness.
- It has two upper and lower poles, two medial and lateral borders, and two anterior and posterior surfaces.
- The upper pole is broad and is in contact with the suprarenal (adrenal) gland, while the lower pole is pointed. The lateral border is convex whereas the medial border is concave. They lie a depressed notch at the middle of the medial border which is known as hilum (hilus).
Covering
- The structure that surrounds the kidney and is closely attached to its surface is called the renal capsule or fibrous capsule or true capsule.
- Covering the fibrous capsule is a perinephric fat or middle fatty capsule, which is basically the collection of fatty tissue. It acts as a shock absorber and helps to maintain the kidney in its position.
- The renal fascia, a collection of connective tissue, lies outside the perirenal fat and surrounds the kidney and suprarenal gland. It has two anterior and posterior layers. Superiorly, these two layers enclose the suprarenal gland and then merge with the diaphragmatic fascia.
- External to the renal fascia is a large quantity forming a part of retroperitoneal fat. It forms a cushion for the kidney.
Structure of the Kidney
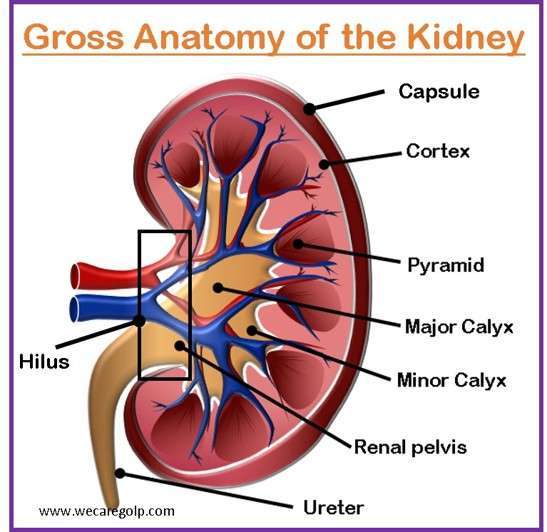
Gross Structure of the Kidney
- Renal capsule: The kidney is surrounded by a thin, fibrous tissue called the renal capsule, which protects the entire kidney from external injury and maintains its shape and integrity.
- Renal cortex: Renal cortex is the outer layer of the kidney that lies immediately below the capsule and outside the pyramid. It contains nephrons (numerous microscopic filtering units), which are responsible for the filtration of the blood and regulation of salt, electrolytes, and fluid to maintain homeostasis in the body.
- Renal medulla: The inner medulla is dark brown and consists of triangular or conical structures of renal tissue called renal pyramids. It is located beneath the renal cortex. The medulla contains tubules and blood vessels that carry out the reabsorption and concentration of urine. The apex of the pyramid is called the papilla, which fits into the minor calyx. The bases of pyramids are capped by the renal cortex called cortical arches. The part of the renal cortex that projects between the pyramids is called the renal columns.
- Minor and major calyces: The papillae extend into several cup-liked structures (7-13 in number) called minor calyces (singular: Calyx). Minor calyces further extend into 2-3 major calyces. These calyces drain the urine from the nephrons via the collecting ducts and transport it to the renal pelvis.
- Renal pelvis: A funnel-shaped structure located in the middle of the kidney is called the renal pelvis. It collects the urine from the nephrons and passages it into the ureter, which transports the urine to the bladder.
- Hilum: The renal pelvis leaves as the hilum. The hilum leads into a space called the renal sinus. The hilum is a site where nerves, vessels, lymphatics, and ureters lead into and out of the kidney.
Microscopic Structure of the Kidney
Nephron
The nephron is the structural and functional unit of the kidney and lengths about 3 cm. Each adult kidney consists of more than one million nephrons and is responsible for the filtration, reabsorption, and secretion processes involved in urine formation. Since each nephron can carry out each specific function, the kidneys can still work even if thousands of nephrons are destroyed or lost due to illness or injury. Each nephron consists of a renal corpuscle and a renal tubule.
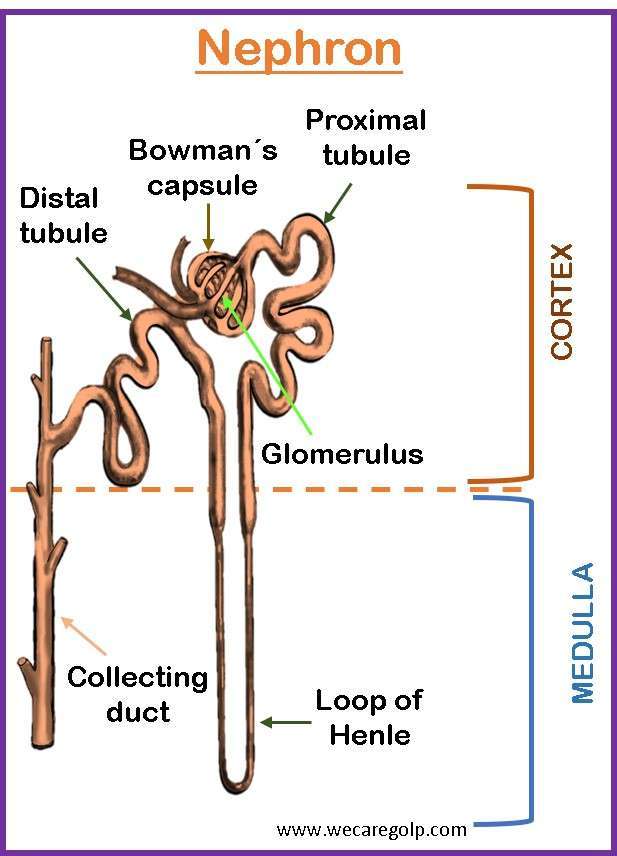
Renal Corpuscle
The nephron begins with the renal corpuscle, consisting of the glomerulus and Bowman’s capsule.
Glomerulus
The glomerulus is a network of specialized high-pressure capillaries that filters blood. An afferent arteriole supplies the glomerulus whereas an efferent arteriole drains it. The positive-pressure gradient helps filter small molecules like water, electrolytes, waste products, and some small proteins through the glomerular capillary walls into Bowman’s capsule. It contains three layers.
- The endothelium: It is the inner layer of the glomerulus containing several pores that allow the filtration of small solutes and fluid from the blood.
- The basement membrane: This middle layer, also called the glomerular filtration barrier (GFB), is permeable to fluid and small (or midsized) solutes. But, the large solutes like red blood cells (RBCs) and protein do not allow to filter. If there is a presence of large molecules in the urine, it signalized the damage to the glomerular membrane.
- The epithelium. The outer epithelium layer contains larger pores than the inner and middle layers which allow the larger molecules to filter into the Bowman’s capsule.
Bowman’s capsule
Bowman’s capsule surrounds the glomerulus. It forms a lumen and directs the glomerular filtrate to the proximal convoluted tubule (PCT). A simple squamous epithelium covers the outermost part, the parietal layer. There is space between parietal and visceral lacer called Bowman’s space. Bowman’s space contains the initial filtrate from the blood. All molecules and fluid filtered by the glomerulus collect in the space.
Renal Tubules
The renal tubule begins at Bowman’s capsule and has three sections, including the proximal convoluted tubule, loop of Henle, and distal convoluted tubule.
Proximal convoluted tubule (PCT)
From Bowman’s capsule, the hyperosmotic filtrate enters the PCT which is in the renal cortex. Most of the filtrate is resorbed by the PTC like water, glucose, bicarbonate, phosphate, some water-soluble vitamins, potassium, calcium, and chloride. Megalin and cubilin, two specialized receptors that bind albumin and vitamin-binding proteins, are responsible for resorbing proteins in the proximal tubule.
Loop of Henle (LOH)
After leaving the PCT, the filtrate is isosmotic due to the selective resorption of most of the solutes and water in the PCT and enters the LOH, which consists of a descending limb and an ascending limb. It is in the renal medulla and has a crucial role in water reabsorption. The descending limb is very permeable to water but not to sodium, urea, and other molecules whereas the ascending limb reabsorbs sodium, urea, and chloride actively and is impermeable to water.
Distal convoluted tubule (DCT)
The hypoosmotic filtrate then enters the DCT which is in the renal cortex. The reabsorption and secretion processes in the DCT are influenced by hormones like parathyroid hormone (PTH), aldosterone, and anti-diuretic hormone (ADH). That is why the DCT plays a role in electrolyte, acid-base, and water balance. In the presence of ADH, the water is impermeable but resorbs some solutes, and the filtrate remains hypoosmotic. In contrast, if the ADH is absent, it is more permeable to water, and the filtrate may become isosmotic.
The juxtaglomerular apparatus (JGA) is located between the afferent arteriole and the returning distal convoluted tubule of the same nephron. It is responsible for regulating both intrarenal (tubuloglomerular feedback) and extrarenal (renin-angiotensin-aldosterone system) mechanisms to maintain both renal and entire body volume status. The macula densa, juxtaglomerular cells, and specialized mesangial cells located outside of the renal corpuscle make up the JGA. The macula densa, which is responsible for blood pressure regulation, are found in the initial part of the distal tubule.
Collecting Duct
The collecting ducts are not part of the nephron. It continues with the nephron and forms after joining the several distal convoluted tubules in the cortex and extends through the medulla to empty into the papilla. It is responsible for the reabsorption and excretion of substances during urine formation. Each duct gathers filtrate from several distal tubules and prepares for the final modification of the urine, primarily transporting water, potassium, and sodium.
- The ADH, released by the pituitary gland, determines water permeability. The urine becomes dilute with small amounts or in the absence of ADH, whereas the concentrated urine results from larger amounts of ADH.
- Depending on the body’s needs, sodium and potassium can be reabsorbed from the filtrate or secreted into the filtrate along the collecting ducts, helping to maintain the body’s electrolyte balance.
- The collecting ducts regulate the transportation of hydrogen ions (H+) and bicarbonate (HCO3) to avoid acid-base imbalances in the body.
Pyramid forms by combining several collecting ducts. Once the urine leaves the collecting ducts, no change in the composition of the filtrate occurs.
Blood Supply
- About 20% to 25% of cardiac output which is about 1200 ml/min at resting condition is supplied to the kidneys. The kidney is the organ that receives the highest blood supply out of all other organs, which is about 400ml/min/100gm.
- Blood reaches the kidney via the renal artery. The renal artery enters the kidney via the renal hilus. It is the branch of the abdominal aorta, branches simultaneously to form the interlobar arteries, the arcuate arteries, the cortical arteries or the interlobular arteries, and the afferent arterioles.
- Again, each afferent arteriole branches progressively into the glomerular capillary network which joins together to form the capillary network known as glomerulus. The second capillary network around the cortical nephrons is called peritubular capillaries and the other that surrounds the juxtamedullary nephrons are called vasa recta.
- Now the peritubular capillaries and vasa recta both drain into the vessels of the venous system that run parallel to the arterial vessels and break progressively to form the interlobular or cortical vein the arcuate vein, the interlobular vein, and finally the renal vein.
- Finally, the renal vein exits the kidney via the renal hilus and joins the inferior vena cava which carries the blood back to the heart.
- Since the renal circulation has the feature of a double capillary network which is why it is also known as portal circulation.
Nerve Supply
The renal plexus, a network of nerves that extends from the abdominal aortic plexus, provides nerve supply to the kidneys. The renal plexus contains the autonomic nervous system which includes both the sympathetic and parasympathetic fibers. It innervates the kidneys and aid in regulating their function.
Sympathetic nerve supply
- It originates from the thoracic splanchnic nerves and travels through the sympathetic chain ganglia.
- It helps regulate
- Blood flow,
- Control the diameter of the renal blood vessels, and
- Influence the release of renin (an enzyme involved in blood pressure regulation).
Parasympathetic nerve supply
- It is less significant than the sympathetic nerve supply.
- Parasympathetic fibers are derived from the vagus nerve (cranial nerve X).
- It generally helps promote
- Rest,
- Digestion, and
- Relaxation.
- It may influence
- Modulating blood flow and
- Urine production.
Summary
- Kidneys are the primary organs of the urinary system which are situated on the posterior abdominal wall, one on each side of the vertebral column at the level of T12 to L3 vertebrae.
- Each kidney weighs about 120-200 g and about 11 cm long, 6 cm wide, and is 3cm thick.
- The kidney is protected with layers of a fibrous capsule, perirenal fat, renal fascia, and pararenal fat from inside to out.
- The kidney tissue, covered by a fibrous capsule or true capsule consists of an outer cortex and inner medulla.
- The outer cortex which is light reddish-brown in color lies immediately below the capsule and outside the pyramid.
- The inner medulla is dark brown in color and is made up of triangular areas of renal tissue called renal pyramids.
- A nephron, which is the functional and structural unit of the kidney, is 1-2 million in number.
- A nephron has two major parts i.e., renal corpuscle (Malpighian corpuscle) and renal tubule (tubular part).
- The kidney is the organ that receives the highest blood supply out of all other organs, which is about 400ml/min/100gm. it receives blood via the renal artery.
- Kidneys are innervated by the autonomic nervous system.
- A nephron is a complex, microscopic structure responsible for fluid and electrolyte balance in the body.
- The collecting ducts have avital role in the final processing of urine before it is excreted from the body.
REFERENCES
- Soriano, R. M., Penfold, D., Leslie, L.W. (2022, July 25). Anatomy, Abdomen, and Pelvis: Kidney. StatPearls Publishing. Retrieved on 2023, May 20 from https://www.ncbi.nlm.nih.gov/books/NBK482385/
- Jones, O. (2022, Dec 19). The Kidneys. TeachMeAnatomy. Retrieved on 2023 May 20 from https://teachmeanatomy.info/abdomen/viscera/kidney/
- Ashalatha, P.R, Deepa, G. (2015). Text Book of Anatomy and Physiology for Nurses. Jaypee Brothers Medical Publishers.
- Jha, R. K., Jha, R. (2021). J and J Health Science Masters of Nursing Entrance. 164-171. Makalu Publication House.
- Pandey, K., Bhandari, B. (2023). Loksewa Secrets For Nursing Officer. 357-358. Samiksha publication.
- Sharma, M., Paudel, K., Gautam, R. (2017). Essential Textbook of Medical Surgical Nursing. 275-330. Samiksha Publication.
- Adhikari, M. Chaulagain, S. (2079). Staff Nurse/PHN Loksewa Comprehensive Review. 555-556. Safal Publication House.
- Jha, S. K. (2078). A Text Book of IBMS. 507-517. Nirvana Publication.
- Silvestri, L. A., M., Silvestri, A. E. (2020). Saunders Comprehensive Review for the NCLEX-RN Examination. 758-759. Elsevier Publication.
- Mani, M., Chinramani, M.S., Bucher, L. (2015). Lewis Medical Surgical Nursing. Vol II, pp 1097-1100. Elsevier Publication.
- Tuitui, R., Suwal, S.N. (2016). Human Anatomy and Physiology. 297-304. Vidyarthi Pustak Bhandar.