Introduction
Diabetes mellitus (DM) is a chronic metabolic condition characterized by increased blood glucose level, polyuria (excessive urine output), polydipsia (excessive thirst), and polyphagia (excessive hunger). If left untreated or uncontrolled may lead to serious damage to the heart, kidney, eyes, and blood vessels.
- In the 2nd century, Aretheus of Cappadocia coined the term diabetes to provide the first accurate description of diabetes.
- Again, in the 17th century, Thomas Wills added the term “Mellitus” to the disease intending to relate extremely sweet taste of urine.
- According to WHO, about 422 million people have diabetes, and 1.5 million deaths are directly ascribed to diabetes each year worldwide. Both the incidence and prevalence of cases have been increasing steadily.
Regulation of Blood Glucose in Healthy Condition
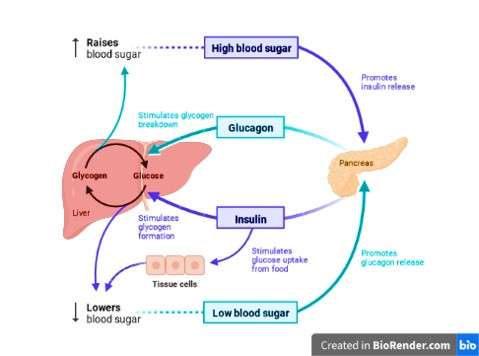
Insulin
- Insulin is a hormone secreted by the pancreas that regulates the blood sugar (glucose) in the bloodstream.
- Insulin helps blood sugar enter into the cells that can use for energy.
- It gives the liver signals to store the blood sugar for later use. Once the glucose enters the cells and liver, the glucose levels in the bloodstream reduce. Thus, insulin production decreases as well.
- Glucose stored in the cells uses as energy. Furthermore, the liver produces glucose when the body is hypoglycemic.
- In conclusion, insulin regulates the metabolism of carbohydrates, fat, and protein.
Types of Diabetes Mellitus
There are different types of diabetes mellitus among which the commonest are listed below.
- Type 1 diabetes mellitus
- Type 2 diabetes mellitus
- Gestational diabetes
- Maturity onset diabetes of the young (MODY)
- Latent autoimmune diabetes in adults (LADA)
- Prediabetes
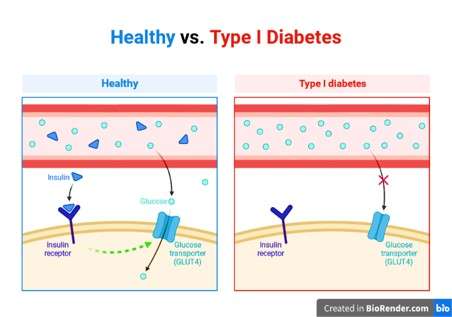
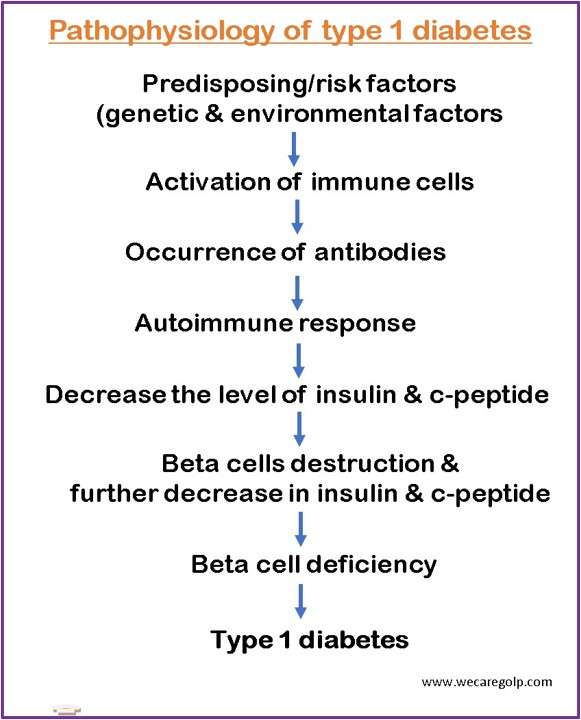
Type 1 Diabetes Mellitus
- It is also called insulin-dependent. In type 1 DM, our body produces little or no insulin. It is an autoimmune condition where our body attacks itself leading to the destruction of beta cells (insulin-producing cells) in the pancreas.
- It can take months to a year for the symptoms to appear.
- Another name for type 1 DM is Juvenile Diabetes because it usually appears in childhood. However, it can develop at any age in life.
- It is predominantly genetics. However, many people won’t get type 1 diabetes even if it is in their genes.
- Any stimuli to the environment, such as the virus, may also contribute to developing type 1 diabetes.
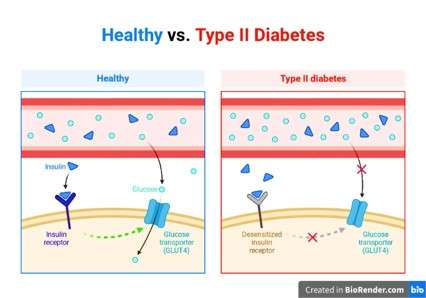
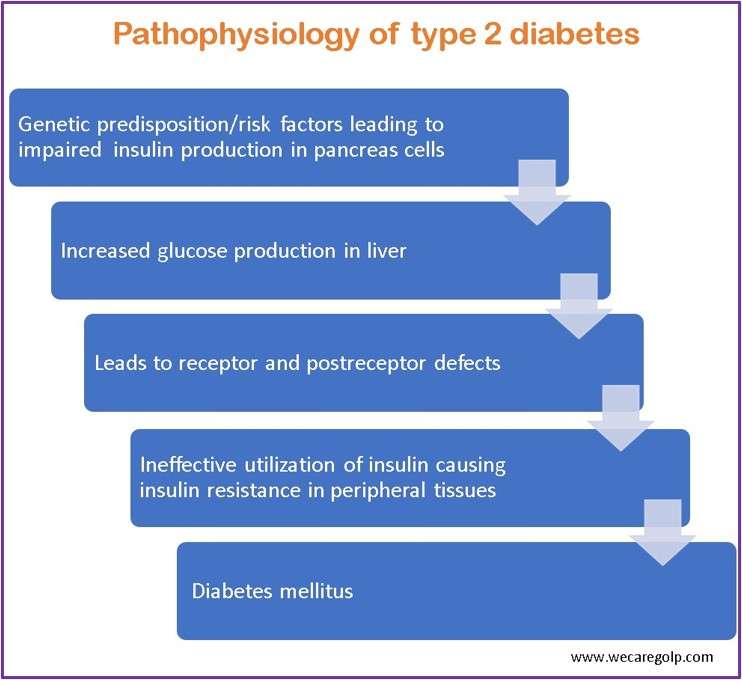
Type 2 Diabetes Mellitus
- It is the most common form of diabetes, where there is impairment in our body to regulate or use insulin in an effective way resulting in unusual blood sugar levels.
- In type 2 DM (also known as adult-onset diabetes), the pancreas produces insulin, but the cells do not respond to insulin (insulin resistance) which affects the process of converting glucose into energy.
- It occurs usually in middle-aged and older people.
- It is more common in African Americans, American Indians, and Asian Americans.
Difference between type 1 & type 2 diabetes
| Type 1 | Type 2 | |
| Condition | β-cells are destroyed and no insulin is released, result hyperglycemia | Insulin is released but no longer effective |
| Start | Usually fast | Usually slow |
| Signs | Mostly clear | Mostly less or not at all |
| Age | Mostly under 40 years | Mostly over 40 years |
| Weight | Differing | Often too high |
| Therapy | Insulin | Movement Diet Weight loss If needed, tablets or insulin |
| Heredity risk | 1-25% | 40-80% |
Gestational Diabetes
- As the name suggests, gestational diabetes can develop in pregnant women, even if they did not have it before.
- Though the causes of GD are unclear, the various pregnancy hormones (e.g., estrogen, human placental lactogen, etc.) could raise glucose levels.
- It occurs when the body fails to produce enough insulin to meet the needs during pregnancy.
- It is most common in 2nd and 3rd trimesters but can appear in any stage of pregnancy. Therefore, the sugar test offers in the 6th or 7th month (or 24 – 28 Weeks) of pregnancy.
- It usually disappears on its own after delivery.
- However, it can lead to type 2 diabetes if the pregnant woman has risk factors for DM.
Maturity onset Diabetes of the Young (MODY)
- MODY adverts to one of the various hereditary forms of diabetes caused by a mutation in an autosomal dominant gene that inhibits insulin production.
- It is a group of a condition characterized by abnormally high blood sugar levels.
- These forms of diabetes usually start before the age of 30 but also can occur later in life.
Latent Autoimmune Diabetes in Adult (LADA)
- LADA is an adult-onset autoimmune diabetes that does not require insulin to control blood glucose levels for at least the first 6 months after diagnosis.
- It shares genetic, immunological, and metabolic features with type 1 and 2 diabetes.
- The World Health Organization’s term for LADA is ‘slowly evolving immune-related diabetes.’
Pre-diabetes
- It is a condition when the blood sugar level rises to a high level but not enough to be diagnosed with type 2 diabetes.
- It is more common in American adults.
- Almost 1 in 3 people in America have pre-diabetes, and the fun fact is almost 80% of people do not even know that they have pre-diabetes.
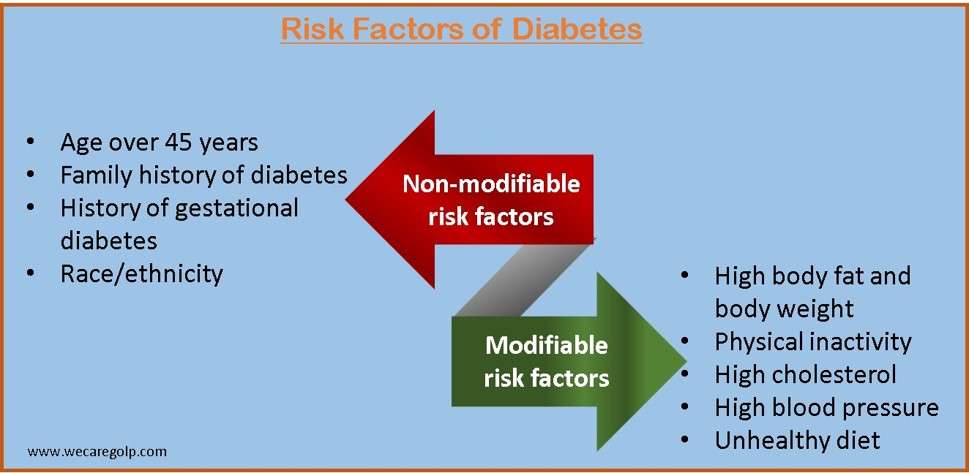
Risk Factors of Diabetes Mellitus
The following diagram shows the modifiable and non-modifiable risk factors for diabetes.
Causes of Diabetes Mellitus
Autoimmune
- The body’s immune system mistakenly attacks beta cells or insulin-producing cells.
- As a result, it damages the beta cells irreversibly. Hence, diabetes occurs due to little or no production of insulin.
Genes and Family History
- Similar to type 1 diabetes, having specific genes may increase your risk of developing type 2 diabetes.
- Some racial/ethnic groups are more likely to experience the disease, which tends to run in the family, e.g., African Americans, American Indians, Asian Americans, etc.
- Genes can also make someone more likely to develop type 2 diabetes by making them more likely to be obese or overweight.
Insulin Resistance
- It is a condition in which muscles, liver, and fat cells do not utilize insulin properly.
- It is typically the first sign of type 2 diabetes.
- Although the pancreas produces more insulin to facilitate glucose uptake into the cells to meet the increased demand, the secreted insulin does not neutralize the blood sugar completely in the bloodstream. It means, it is insulin is not sensitive.
Age
- Because of the combined effects of ageing worsening pancreatic function and rising insulin resistance, older persons are at a greater risk for developing type 2 diabetes.
Overweight, obesity and physical inactivity
- You are more prone to acquire type 2 diabetes if you have a sedentary lifestyle, are overweight, or obese.
- Insulin resistance can occasionally result from excess weight and is widespread in type 2 diabetics.
- Additionally, the distribution of body fat affects results; diabetes, insulin resistance, and heart and blood vessel disease are all associated with excess abdominal fat.
- Also, physical inactivity results in improper utilization of energy and glucose.
Hormonal disease
- Excessive levels of various hormones can occasionally lead to insulin resistance and diabetes, e.g., cortisol and stress hormone (Cushing´s Syndrome), thyroid hormone (hyperthyroidism), and growth hormone (acromegaly).
Others include smoking, stress, high blood pressure
- People with high blood pressure are usually insulin resistant and are at a higher risk of developing diabetes than people with normal blood pressure.
- Smoking increases oxidative stress by combination of cigarette smoke with oxygen in the body, causing damage to the cells.
- Evidence shows that infection and oxidative stress is associated with an elevated threat of diabetes.
Medicines
- Certain medicine can sometime cause damage to the pancreas or inhibit the working process of insulin. Such as: corticosteroids, psychiatric drugs, anti-seizures, anti-rejection medicine, etc.
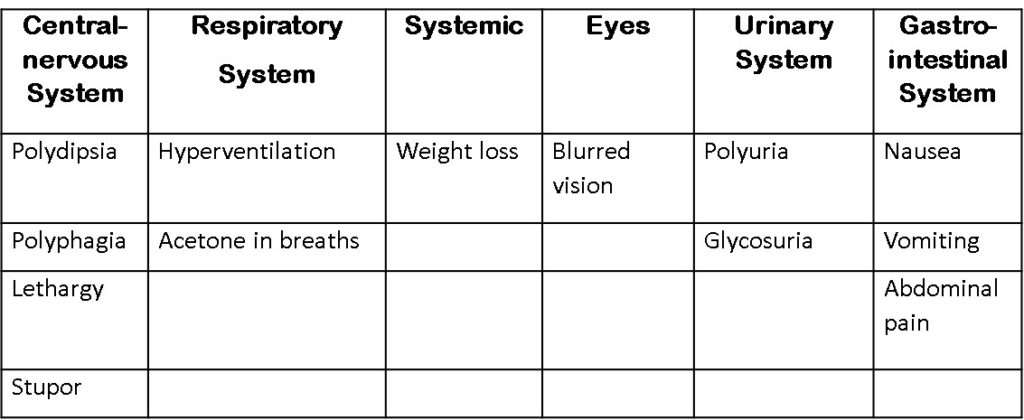
Symptoms of Diabetes Mellitus
Pathophysiology of Diabetes Mellitus
Diagnostic Procedure
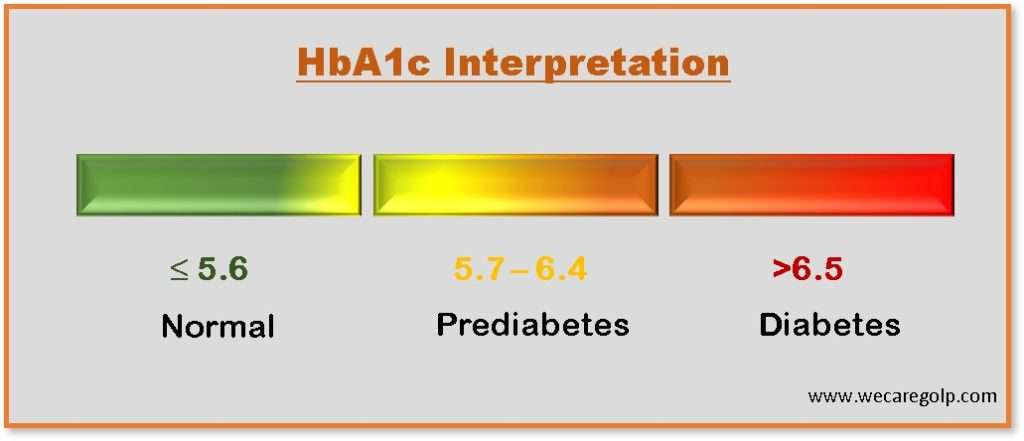
HbA1c
- The gold standard for screening diabetes is the HbA1c test or glycosylated hemoglobin test.
- It provides an average blood glucose level or period of three months as a broad indicator of diabetes control.
- The HbA1c is the measurement of hemoglobin-bound glucose inside the red blood cells.
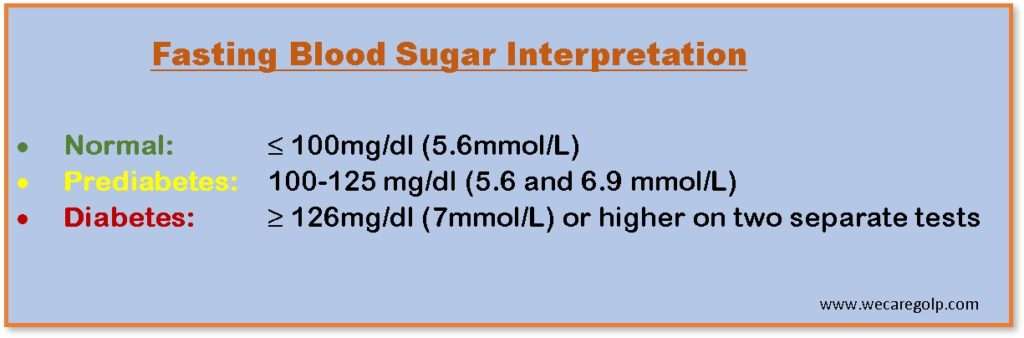
Fating Blood Glucose
- A fasting blood sugar test should perform after not eating or drinking anything other than water for at least eight hours (fasting).
- Therefore, it recommends taking a blood sample in the morning.
Random blood sugar test
- It measures randomly regardless of what and when you ate last.
- A level of 200mg/dl (11.1mmol/l) or higher suggests diabetes.
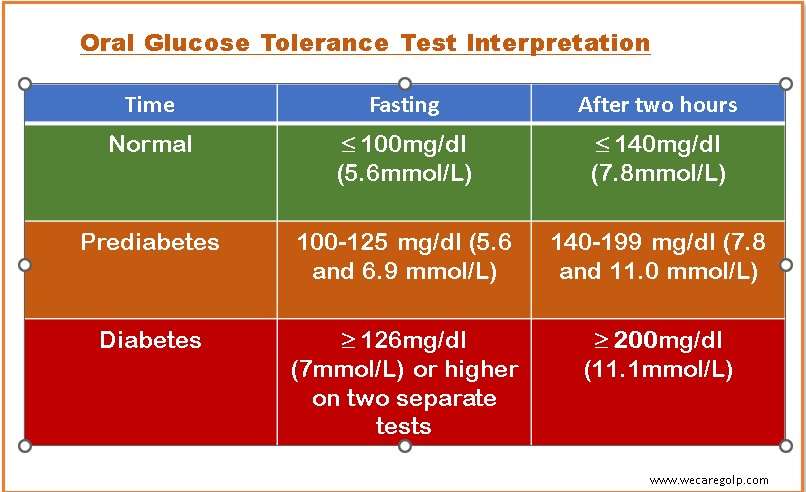
Oral glucose tolerance test (oGTT)
- To do oral glucose tolerance test (oGTT), you must abstain from food for eight hours.
- Firstly, a blood sample will take from the vein, and then you will get 75 grams of glucose dissolved in 250-300 ml of water to drink within 5 mins.
- Another blood sample will draw after two hours.
Screening
The American diabetes association (ADA) recommends diabetes screening routinely for people with the following conditions.
- All adults aged 35 or older
- People younger than 35 who are overweight or obese and have one or more risk factors associated with diabetes
- People who have been diagnosed with prediabetes
- Women who have had gestational diabetes
- Children who have a family history of type 2 diabetes mellitus or other risk factors and are overweight or obese.
Anti-body test
- GAD (glutamic acid decarboxylase) antibody test is reliable serological markers of insulin-dependent diabetes mellitus.
C-peptide
- It shows the difference between the insulin the body produces and the insulin injected into the body.
- A c-peptide level of less than 0.2 nmol/l is associated with a diagnosis of type 1 diabetes.
Treatment of Diabetes Mellitus
Treatment of diabetes can be classified as:
- Non-drug therapy and
- Drug therapy
Non-drug Therapy
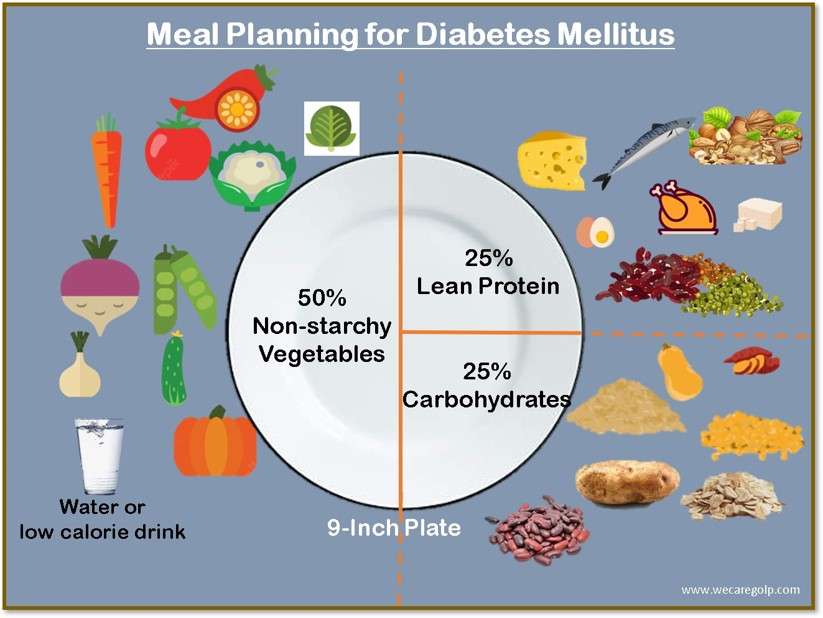
Diet
- Make a proper meal plan; include fiber and protein in your food so that it causes delayed absorption of food that won’t spike up your blood sugar level.
- Make better food choices and emphasize homemade meals rather than junk or takeaways.
- Watch your portion size.
Exercises
- Exercise helps in the proper utilization of energy by our muscles. It also increases the body’s sensitivity to insulin.
- Physical activity of at least 45 minutes per day is beneficial for diabetes patients.
- The recommended exercises include walking, jogging, skipping, yoga, swimming, etc.
Weight loss
- Abdominal fat is one of the main reasons for diabetes mellitus and insulin resistance.
- Weight loss also aids in minimizing the risk of complications from diabetes.
- Some research also suggests that if you lose a substantial amount of weight, then your diabetes is likely to go into remission.
Drug Therapy
Oral hypoglycemic agent
- Sulfonylureas: stimulates beta cells to release more insulin. for e.g., tolbutamide, glimepiride.
- Meglitinides: non-sulfonylurea insulinotropic agent.
- Biguanides: decreases insulin resistance and does not affect beta cells. E.g., metformin phenformin.
- Thiazolidinediones: decrease insulin resistance in the peripheral target tissue.eg: rosiglitazone, pioglitazone.
- Alpha-glucosidase inhibitor: delays carbohydrate absorption from the GI tract. Acarbose and miglitol are some examples. Side effect includes diarrhea, bloating, gas, etc.
Insulin Therapy
Rapid-acting insulin
- Can be injected before the meal
- Onset 5-15 minutes with a peak in 30-60 minutes
- Stays in the bloodstream for 2-5 hours
- E.g., NovoLog, Humalog.
Short-acting insulin/regular
- Usually injected 15-30 minutes before a meal
- Onset 30 minutes and peaks in 1-3 hours.
- E.g., Novolin R, Humulin R.
Intermediate-acting
- Used to control glucose levels between meals
- Can combine with short-acting insulin
- Onset 1-2 hours and peaks at 4-8 hours.
- Eg: Novolin N, Humulin N.
Long-acting insulin
- Usually taken once a day 30 minutes before meals.
- It keeps blood sugar steady throughout the day.
- It cannot mix with other insulins. E.g., Lantus, Levemir.
Management of Diabetes Mellitus
Here are a few measures to manage diabetes mellitus.
- A healthy diet is the cornerstone of a healthy life whether you have diabetes or not. But if you have diabetes, then you must observe how foods that affect your blood glucose level. A better food choice is the key to managing diabetes. Avoid sweetened beverages, prefer whole fruits instead of juices¸ include fibers and protein in your diet that cause slow absorption of food and do not spike up your blood sugar.
- Keep yourself moving. Engage yourself in some physical activities like jogging, skipping, and swimming. You need to sweat it out. Keep moving even if you are in your office. Take 5-10 min of walking around.
- Store your medicines properly. Maintain the temperature of insulin. Take medicine at the same time every day for better results.
- Take care of your body. Make a sick day plan. Infection and illness may interrupt for the better management of diabetes, but plan and consult with your endocrinologist or physician.
- Take care of your foot. Wear thick socks, and apply moisturizers in winter. Take care of cuts and injuries, if any.
- Avoid alcoholic beverages and cigarettes, but if you do, avoid drinking on an empty stomach. Get the doctor’s permission before having some drinks.
- Reduce your stress level. Keep yourself engaged and distracted. Listen to music, dance, and read books to keep your mind busy.
- Get help. Feel free to vent your emotions and feelings because that is okay!
Emergency Management of Diabetes Mellitus
Having diabetes mellitus is just like living on the edge. American diabetes association states that there are three main diabetic emergencies.
Hypoglycemia
- Hypoglycemia is the most common diabetic emergency and occurs in people who have insulin therapy.
- It is the condition when your blood sugar level drops too low or less than 70mg/dl.
- If not managed on time, it may result in a coma or death.
- Symptoms include shakiness, blurred vision, excessive sweating, loss of consciousness, cold skin, excessive hunger, irritation, etc.
- For the management, if you see someone going into hypoglycemia, immediately give some sweet beverages, candies, or glucose orally.
- In hospital settings, givingan intravenous (IV) bolus of 50% dextrose will be the treatment of choice.
- Keeping some sweet candies or juice at home or even in the bag could be a lifesaver for people with diabetes.
Diabetic Ketoacidosis (DKA)
- It is a condition of building acids (called ketones) in the bloodstream due to a lack of insulin.
- It is another life-threatening condition for diabetes patients and usually occurs in type 1 diabetes.
- Symptoms include dry skin and mouth, fruit-smell breathing, nausea, vomiting, confusion, weakness and fatigue, shortness of breath, etc.
- Management: Check your ketones if your sugar is more than 250 mg/dl, test for a sign of infection, and test arterial blood gas for the pH of the blood.
- Emergency management: administer Iv insulin to bring blood sugar levels down immediately and start electrolyte replacement therapy to maintain sodium and potassium levels.
Hyperosmolar Hyperglycemic Nonketotic Syndrome (HHNS)
- It is a life-threatening condition resulting from uncontrolled diabetes mellitus, and is characterized by blood sugar above 600 mg/dl, fever more than 100.4 degrees Fahrenheit, dry mouth, confusion, hallucination, or even passing out.
- It can result from poor management of diabetes, not taking medication as prescribed (non-compliance), and some medications like corticosteroids and diuretics.
- Management typically involves: IV fluid therapy (saline to rehydrate the body quickly), and may also need IV insulin to bring blood sugar levels down.
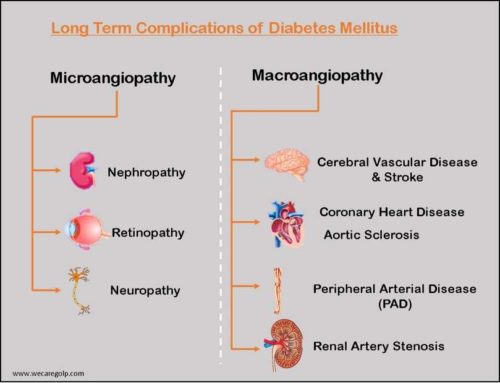
Complications of Diabetes Mellitus
It includes
- Hypoglycemia
- Diabetic retinopathy (eye problem)
- Diabetic neuropathy (nerve damage)
- Diabetic nephropathy (kidney disease)
- Cardiovascular problems and strokes
- Diabetic foot or wound.
- Gum problems
Prevention of Diabetes Mellitus
Because type 1 diabetes is an autoimmune system disorder, it cannot prevent. You also have no influence over some type 2 diabetes causes, such as your genes or age.
However, many more diabetes risk factors are controllable. The majority of diabetes prevention technique involves making small changes to your diet and exercise regimen.
Here are some steps you may take to put off developing type 2 diabetes mellitus if you have been diagnosed with prediabetes or risk factors are there.
- Get 150 minutes or more of cardiovascular activity each week by cycling or walking.
- Eliminate refined carbs, saturated and trans fats from your diet.
- Consume more whole grain, fruits, and veggies.
- Avoid junks and carbonated beverage, smoking and alcohol.
- Check your portion size. Eat a well-balanced diet in a well portion sizes.
- Try to maintain a healthy level of body mass index (BMI).
- Be spiritually, mentally, and emotionally healthy.
References
- https://www.mayoclinic.org/diseases-conditions/diabetes/symptoms-causes/syc-20371444
- https://www.msdmanuals.com/home/hormonal-and-metabolic-disorders/diabetes-mellitus-dm-and-disorders-of-blood-sugar-metabolism/diabetes-mellitus-dm
- https://my.clevelandclinic.org/health/diseases/7104-diabetes-mellitus-an-overview
- https://www.ncbi.nlm.nih.gov/books/NBK551501/
- https://www.who.int/news-room/fact-sheets/detail/diabetes
- https://www.britannica.com/science/diabetes-mellitus